[18F]FDG-PET/CT Texture Analysis in “Hot” Thyroid Nodules: Results of the validation Cohort
Introduction
The incidence of thyroid incidentalomas is increasing according to the fact that PET/CT is increasingly used for oncological and non-oncological applications. The chance of malignancy among the incidentalomas detected by [18F]FDG is higher than incidental nodules discovered with other imaging modalities and the 2015 American Thyroid Association Management Guidelines [1] recommend fine-needle aspiration (FNA) in case of focal [18F]FDG uptake within a thyroid nodule. However, if it is true that a focal [18F]FDG uptake within a thyroid nodule has an increased risk of malignancy, it is also true that not all thyroid nodules characterized by a focal [18F]FDG uptake are malignant. Therefore, it would be really useful an approach able to select patients proposed for FNA. In our previous publication, we explored the role of textural analysis of [18F]FDG-PET to refine the selection of the patients with “hot” nodules to be referred for cytology. Seven indices including SUVstd, SUVmax, metabolic tumor volume (MTV), total lesion glycolysis (TLG), Skewness, Kurtosis, and Correlation calculated from the grey level co-occurrence matrix (CorrelationGLCM) were selected as potential diagnostic biomarkers able to stratify the patients with thyroid incidentaloma identified on [18F]FDG-PET/CT scans, with respect to the risk of a malignant thyroid nodule [2]. However, the role of the identified candidate biomarkers needs to be tested on a separate patient cohort to be validated. Therefore, the aim of this study was to validate the ability of texture analysis on [18F]FDGPET/ CT to predict final diagnosis in “Hot” Thyroid Nodules.
Materials and Methods
Patients
We retrospectively evaluated the medical records of all the patients who performed an [18F]FDG-PET/CT from January 2017 to December 2018. Methods for patient selection and data collection were previously detailed [2].
Among all subjects who underwent a [18F]FDG-PET/CT (8465 scans) and had a thyroid uptake described in the medical record (398 scans), we selected 52 patients who performed further diagnostic steps in our institution. Twelve patients, referred to ultrasonographers, did not perform cytology. Eight patients were excluded from the analysis because a final diagnosis was not available. Accordingly, 32 patients (male:female=5:27; age 64±12 years) were included in the analysis. Indication for [18F]FDGPET/ CT was oncological in 30 cases and non-oncological in the remaining 2 cases (1 vasculitis, 1 Langerhans cell histiocytosis). In the oncologic group, [18F]FDG-PET/CT was performed for breast tumor (8 cases), lymphoma (6 cases), gastro-intestinal tumors (5 cases), head and neck (2 cases), thymic masses (2 cases), bladder cancer (1 case), mesenchymal tumor (case 1) and lung cancer (1 case). In the remaining 4 cases [18F]FDG-PET/CT was performed in metastatic patients to search for the primary tumor (4 cases). This retrospective observational study was reviewed and approved by the Local Ethics Committee.
Cytology
Methods for fine-needle aspiration and cytology were previously detailed [2]. All cytological results were reported according the SIAPEC-IAP 2014 classification [3].
In case of negative cytology (TIR2), no further studies were immediately performed, and the nodule was considered benign. In case of non-diagnostic (TIR1) or doubtful (TIR3) results, further cytological samples or histology were used as final diagnosis when available (n=6), otherwise patients were excluded (n=8).
[18F]FDG PET/CT acquisition protocol and analysis
[18F]FDG-PET/CT image acquisition and visual interpretation were previously detailed [2]. PET images were segmented using LifeX software (http://www.lifexsoft.org) [4] settled with a threshold of 40% SUVmax. The region of interest (ROI), set in the target tissue (i.e., incidentaloma), was delineated in 3D and then textural features were extracted using the same package (http:// www.lifexsoft.org) [5]. LifeX was settled up using the following parameters for calculation of the features: 64 gray levels to resample the ROI content which was performed in absolute terms between a minimum of 0 and a maximum of 20 [6]. A total of 43 features were extracted from the analysis of the volumes inspected. The correction for partial volume effect was not applied. As previously detailed, LifeX calculated shape, second order and higher-order features only for a ROI including at least 64 voxels.
Statistical Analysis
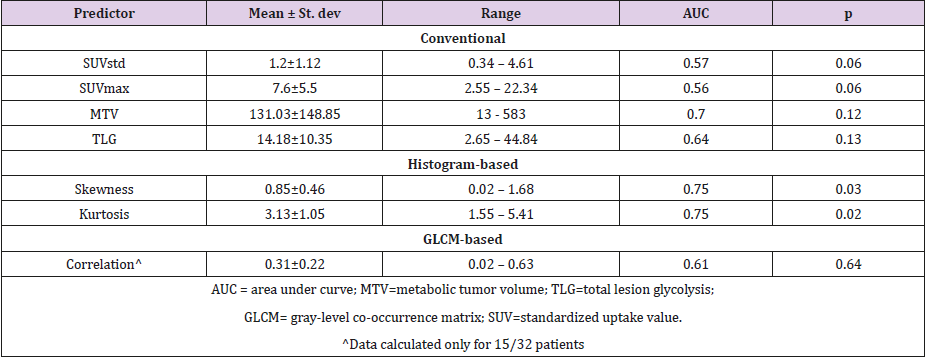
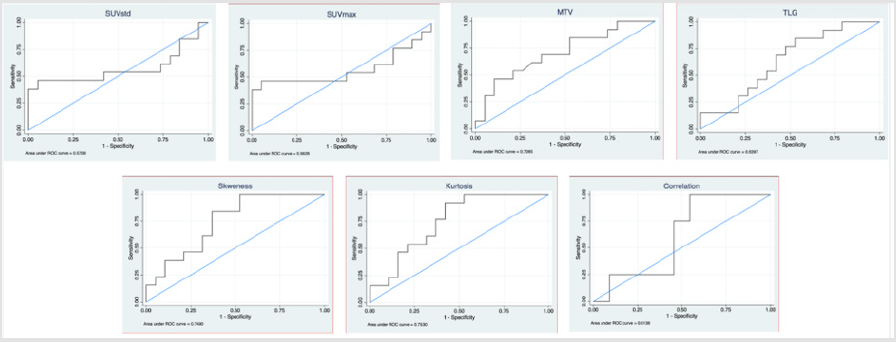
Statistical analysis was performed using the STATA package (StataCorp. 2017. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC). Continuous normally distributed data were expressed as mean ± standard deviation. Conventional PET parameters and textural features previously identified as possible diagnostic biomarkers (SUVstd, SUVmax, MTV, TLG, Skewness, Kurtosis, CorrelationGLCM) [2] were compared to final diagnosis using logistic regression. For each predictor the truth table (true and false positive and negative values) was determined. Receiver operating characteristic (ROC) curves were plotted and for each curve, the area under the curve (AUC) was calculated. Additionally, Compacity, previously identified as predictor able to identify TIR classes [2], was assessed by multinomial logistic regression. A p-value < 0.05 was considered statistically significant.
Results
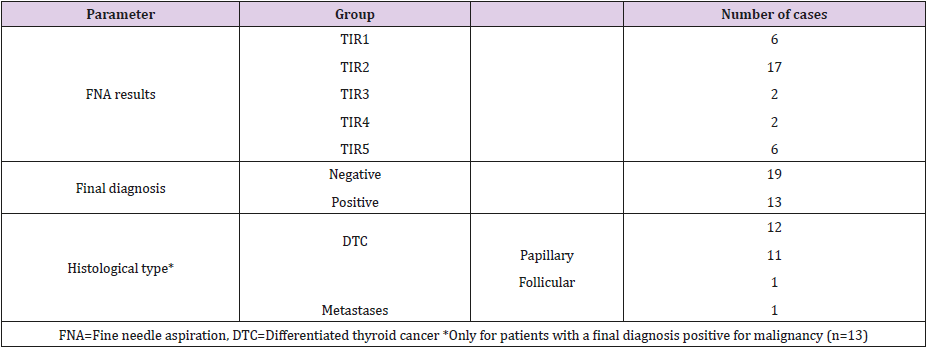
Overall 32 patients were included in the study Table 1 summarizes the characteristics of the cohort of patients included in the analysis. FNA was non-diagnostic in 6 cases, negative in 17 cases, doubtful in 2 cases (TIR3), suspected in 2 cases, and positive for malignant tumor cells in 6 cases. Patients classified as TIR1, repeated the FNA which resulted non-diagnostic (TIR1) in 5 cases and suspicious (TIR4) in one case. The cases that resulted non-diagnostic twice, presented suspicious characteristics on ultrasonography and underwent surgery; pathology resulted positive for DTC in all cases. Both TIR3 cases underwent surgery resulting negative for malignancy (oxyphil cell adenoma = 1, thyroid hyperplasia =1). All TIR4 or TIR5 were proven to be malignant. Nodules resulted malignant (n=13) included 12 thyroid cancers (papillary thyroid cancer = 11, follicular thyroid cancer =1), and 1 metastasis from neuroendocrine tumor.
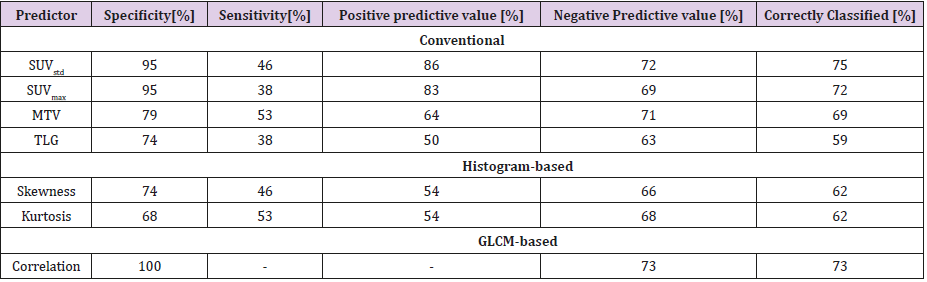
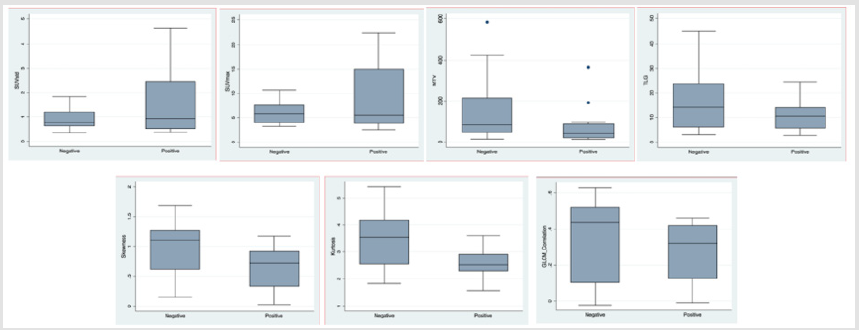
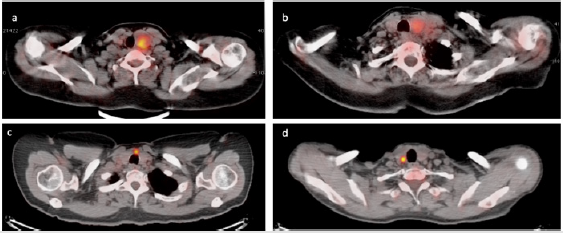
Thyroid [18F]FDG uptake was unilateral in the majority of patients (n=31) occurring in the isthmus in 1 case, in the right and left lobe in 15 and 13 cases, respectively. In the remaining case [18F] FDG uptake involved both thyroid lobes. Fifteen patients (8 with a final diagnosis of DTC) had small ROI (i.e., < 64 voxels), therefore all features were available only for 17 patients (5 with a final diagnosis of DTC). Table 2 summarizes results of the 7 features tested as predictors. Skewness and kurtosis were significantly different in benign and malignant nodules Table 2. Figure 1 shows the box-plots of the 7 tested features stratified for the two subgroups within the cohort. Figure 2 shows the ROC curves (together with the reference 50% AUC line) for the metabolic volume and the texture related features. Table 3 summarizes the predictors and their power in the identification of the negative or positive subgroups in the cohort. All features showed higher specificity than sensitivity. SUVstd classified as correct the highest number of nodules. Compacity failed in differentiating TIR classes (p=0.16). Figure 3 shows examples of four patients with thyroid nodules characterized by different patterns of [18F]FDG uptake (low-moderate uptake in a and b, high uptake in c and d).
Table 3: Summary of predictive power of the significant predictors previously identified as potential diagnostic biomarkers.
Figure 1: Box plots of the 7 tested features stratified for the two subgroups (benign versus malignant) within the cohort.
Figure 3: Cases of four patients with thyroid nodules characterized by different patterns of [18F]FDG uptake. Upper panels show benign (TIR2 in a) and malignant (TIR5, final diagnosis of papillary DTC - pT4apN1apM1 - in b) thyroid nodules with low-moderate [18F]FDG uptake. Lower images show benign (TIR3b, final diagnosis of oxyphil cell adenoma in c) and malignant (TIR4, final diagnosis of papillary DTC - pT1a - in d) thyroid nodules with high [18F]FDG uptake.
Discussion
TOur results confirmed that textural analysis on [18F]FDG-PET/ CT might be used to refine the selection of the patients with “hot” nodules to be referred for cytology. The prevalence of thyroid incidentaloma on [18F]FDG-PET/CT was higher than previously reported and literature data (about 4.7% versus 1.2-4.3%) [2,7-9] while the percentage of patients who performed additional workup was lower than our previous findings (ultrasound available in 13% versus 19%). However, the number of patients who underwent an FNA was comparable to our previous findings (10% versus 12% of subjects). In fact, the prognosis associated with underlying malignancy should be considered before investigation of [18F]FDG–avid thyroid incidetalomas and certainly before any treatment [10].
Skeweness and kurtosis confirmed to be significantly different in negative and positive nodules with a better discriminative power than previously reported (AUC=0.75 versus AUC=0.66 and AUC=0.55, respectively). Interestingly, the AUCs of most of the tested parameters resulted higher than in the “discovery” cohort (MTV, skeweness, kurtosis, correlation). In fact, generally, validation analysis present lower performance than obtained in the training phase. Distribution of image-derived indices within benign and malignant nodules were confirmed except that for MTV and TLG. In the present cohort, volumes of malignant nodules were smaller than benign ones, possibly negatively affecting the results. In fact, small volumes prevent the possibility to calculate shape and higher-order features by LifeX. In our population, all features were available for 17/32 patients (only 5 with a final diagnosis of DTC). However, small size is a typical feature of thyroid incidentaloma.
These results are promising since they confirmed most of our previous findings. Different approaches have been tested to identify [18F]FDG-avid nodules at high risk of malignancy with some disappointing results, mostly lacking of any type of validation [10-18].
Essential requirement for biomarkers research is the validation phase. In fact, novel parameters need to be confirmed reliable using an internal approach (e.g. cross-validation or bootstrapping) or an independent one (e.g. split sample, temporal or geographical), being the latter more robust [19]. We adopted a temporal inclusion strategy. The parameters that resulted significant in the discovery study have been tested in the present and resulted significantly associated with malignancy. The present study suffered from some limitations. Firstly, it was retrospective and evaluated a limited number of patients. Secondly, textural features were not available for the entire cohort. Thirdly, partial volume correction was not applied, however it should be considered according the small size of nodules.
Conclusion
Our results confirmed that textural features differed in benign and malignant [18F]FDG-avid nodules. Accordingly, textural analysis on [18F]FDG-PET/CT might be used to refine the selection of the patients with “hot” nodules to be referred for cytology.
For more Articles: https://biomedres01.blogspot.com/



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.