Incidence, Prevalence, And Complications of Pressure Ulcers In General Medical and Surgical Units Using A Multidisciplinary Model (Prospective Cohorte)
Introduction
Pressure ulcer is defined as a localized lesion or injury to the skin and/or the underlying tissue as a result of unrelieved pressure, shear, friction or a combination of all these, over a bony prominence. [1] It is graded based on the depth and damage to the skin ranging from non-blanching erythema of intact skin to full-scale tissue destruction. [2] Despite the great successes in medicine, pressure ulcers burden remains significantly huge and is ranked as the third costing disease after cancer and cardiovascular diseases. [3] The increased cost is related to the treatment of wound infections, debridement/closure procedures, dressing supplies, special mattresses/cushions, hospital stay, home care services, and time lost from work. More importantly, pressure ulcers impact the patients’ quality of life by limiting their mobility and social activities. [2,4,5] Globally, the incidence of pressure ulcers varied from 2 - 20 ulcer/1000 patient-days, depending on the institution and the population of patients studied. Also, the prevalence varied from 5-13%. [6-9] Nationally, there are no data regarding pressure ulcers in general medical and surgical units.
The objectives of the study were to calculate the prevalence and incidence of pressure ulcers. In addition, to describe the clinical care delivered to inpatients with pressure ulcers by identifying the clinical disciplines involved in their care, the frequency of their visits, and the complications documented among patients with pressure ulcers.
Methods
The design of the study was a prospective cohort and was conducted over one month. Weekly visits to all general medical and surgical units (6 units) at King Abdulaziz Medical City-Jeddah were done during the month of August 2016. All inpatients with preexisting pressure ulcers from home, along with those with new pressure ulcers developed while in-hospital, were included in the study and followed weekly until discharge or the end of the study. Patients from the Pediatric, Obstetrics and Gynecology, Cardiac, Oncology, and Intensive care units were excluded. Data collection team consisted of four medical students who were trained to use the data collection tool. The variables included in the study were patient variables (age, body mass index, hemoglobin level, mobility, urinary catheter, length of stay, number of ulcers) and wound variables (EPUAP grading scheme, PUSH score for wound healing, wound infection, surgical debridement). In addition, the clinical disciplines involved in the care of patients with pressure ulcers (nutritional services, wound care nurse, occupational therapy, plastic surgery, home care) and the frequency of their visits were documented. The outcome measures used in the study (PUSH score for wound healing, EPUAP grading scheme) are valid and reliable [10-13]. Ethical approval to conduct the study was obtained from the king Abdullah International Medical Research Center (KAIMRC).
Statistical Analysis and Results
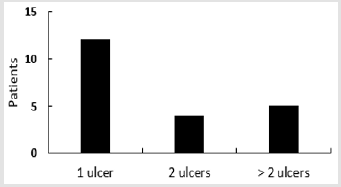
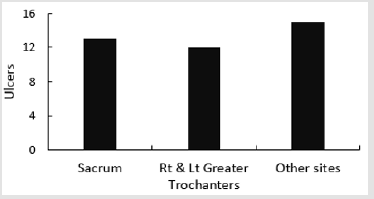
A sample size of 278 was estimated using Epi Info™ to have a confidence level of 95% assuming that prevalence of patients with pressure ulcers is 7% and the margin of error is 3%. Data was entered, cleaned, and analyzed using SPSS Statistics Version 25. The total number of patients admitted to the medical and surgical units during the study period was 370 patients, and their total length of stay during the four-week period of the study was 2444 days. Twenty-one patients with a total of 40 pressure ulcers were identified. There were only four new ulcers developed in the medical and surgical wards; the rest developed either at home or in the intensive care unit. The calculated prevalence of patients with pressure ulcers in the medical and surgical units was 5.7% (95% CI 3.4 -8.0), and incidence of pressure ulcers was 1.6 (95% CI 1.1- 2.1) ulcer/1000 patient-days. Majority of the patients [12] had one ulcer 57%, Figure 1. The most common stage for pressure ulcers was stage two (15 ulcers) 38%, and the most common site was the sacrum (13 ulcers) 33% Figure 2.
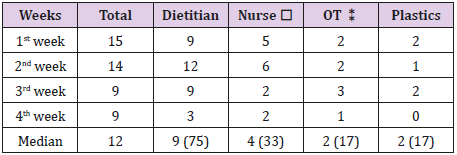
The median age of the patients was 70 years. In this cohort, sixteen patients, 76%, were bedridden and with urinary catheters (incontinent). Also, seven patients, 33%, received antibiotics for infected ulcers, and two of them died due to sepsis. In addition, twenty patients, 95%, were anemic with mean hemoglobin level of 9.4 g/dL, but only three of them had low body mass index (BMI <18). On discharge from the hospital, nineteen patients, 91%, needed home care. Paired t-test that was done to evaluate the healing process of pressure ulcers (40 ulcers), and it showed a significant statistical and clinical improvement in ulcers’ healing after a total follow up time of 209 patient-days. The estimated mean difference in PUSH score between the initial and last follow up visits was 3 out of 17 with p-value of 0.007. Based on requests from the primary physician, the pressure ulcer patients were assessed and managed by the multidisciplinary wound services (dietitians, wound care nurses, occupational therapists, and plastic surgery). The proportions of pressure ulcers patients, who were seen during the four-week period of the study by dietitians, wound care nurses, occupational therapists, and plastic surgery during the study period, were 75%, 33%, 17%, and 17% respectively Table 1.
Table 1: Numbers of patients seen weekly by Multidisciplinary wound care services (%).
⁎wound nurse, ⁑ occupational therapy.
Discussion
The calculated incidence 1.6 ulcer/1000 patient-days and prevalence 5.7% in this study is very close to the figures published in the literature previously. These findings show that the burden of pressure ulcers at KAMC-Jeddah is as huge as its burden worldwide. [6-9] Also, findings show that pressure ulcers patients are likely to be bedridden, incontinent and at risk of malnutrition and wound infection. The typical pressure ulcer patient in this cohort was an elderly patient with a single (stage II) sacral ulcer. Patients with pressure ulcers at KAMC-Jeddah receive consultation based multidisciplinary wound care services from dietitians, wound care nurses, occupational therapists, and plastic surgery. In this model of care the primary physician responsible for the patient decides when to refer the pressure ulcer patient and which wound care service is needed. Subsequently, wound care professionals do not assess all patients who may potentially benefit from their services, nor collaborate to guide the care of individual patients. As a result, patients may receive fragmented and uncoordinated care. For example, the average number (median) of patients seen during the study period by wound care nurses and plastics service weekly was four and two pressure ulcers patients respectively, which represented only 33% and 17% of all pressure ulcers patients Table 1.
According to the KAMC-Jeddah Bed Management Department, the median length of stay for patients with pressure ulcers is 25 days in comparison to 6 days for patients without pressure ulcers. This increased length of stay can be partially explained by the lack of assessment and managment of all the pressure ulcer patients by all the wound care services, and by the lack of the collaboration between the services when managing individual pressure ulcer patients. Multidisciplinary and interdisciplinary care are terms used to describe team approaches to clinical management of diseases. Multidisciplinary approach describes a team of two or more health care workers representing different disciplines and working independently to manage a medical problem. While in the interdisciplinary approach, the team members work together, communicate and collaborate more effectively to manage the patient. [14-18] In the area of pressure ulcer management, there is no evidence that one of the two approaches are better than the other; however, this is not a definite answer and certainly more researches are needed in the field. The study had two strength points: being the first national study to report incidence and prevalence of pressure ulcers in general medical and surgical wards and the prospective nature of data collection. Although four weeks is a short period, it was considered appropriate for patients who get admitted with acute conditions to general medical and surgical wards.
Conclusion
Pressure ulcers prevalence and incidence was 5.7% and 1.6 ulcer/1000 patient-days respectively. Majority of pressure ulcer patients were anemic, bedridden, incontinent, and needed home care on hospital discharge. Further research is needed to clarify the best team approach to manage patients with pressure ulcers.
For more Articles: https://biomedres01.blogspot.com/



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.