The Importance of Radio Allergosorbent Testing Early in the Management of Atopic Dermatitis in Children referred to Secondary Care
Introduction
Atopic dermatitis is a chronic itchy inflammatory skin condition which can affect up to 2% of the population [1]. It has hereditary predisposition affecting infants, children extending to adulthood. In children different studies demonstrated prevalence of 8-20% [1,2]. In children a strong association has been demonstrated between IgE mediated food allergy and atopic dermatitis [3]. Atopic dermatitis is usually linked to certain allergies [3] and despite the term atopic, up to 60% of children with the condition do not demonstrate IgE- mediated sensitivity to allergens [4]. In general patients suffer from atopic dermatitis or parents of young patients often suspect allergies causing the problems and they point out food as a cause or flare up factor. However, only a small percentage specifies these as a possible factor [5]. The clinical picture and presentation can also be more complicated by other factors including psycho-emotional, environmental, viral or bacterial infection [5]. Atopic dermatitis was viewed to be an allergic disease for a period [6,7]. Immune mediators in maternal breast milk influence the development of childhood eczema in that elevated Li- 1B, IL-17 of CCL17 is associated with more than a halved risk of childhood eczema in a high-risk cohort [8,9]. There are many tests advocated to be helpful in the diagnosis, identifying the triggering factor and grading of atopic dermatitis. These include skin prick testing, RAST, Food challenge and Patch Test. Other commercially available tests not necessarily recommended by doctors due to the lack of scientific evidence supporting them include allergy testing kits, such as hair analysis tests, kinesiology tests and VEGA tests. In the United Kingdom patients with atopic dermatitis are usually seen by Primary Care General Practitioners. Diagnosis and initial treatment are usually given. Only those who fail to respond sent to the secondary care for specialist assessment and management.
Materials and Methods
133 patients under the age of 12 were enrolled. Standard RAST testing was requested for all. This included dairy products, house dust mite, grass, nuts, seafood, cereals, dog dander and cat epithelium. The result and lever of IgE (IU/ml) was graded as follows: -ve if IgE (IU/ml) is less than 0.35, Grade 1: 0.35-0.69, Grade 2: 0.70-3.49, Grade 3: 3.5-17.49, Grade 4: 17.50-52.49, Grade 5: 52.50-99.99, Grade 6>100.52.49.
Results
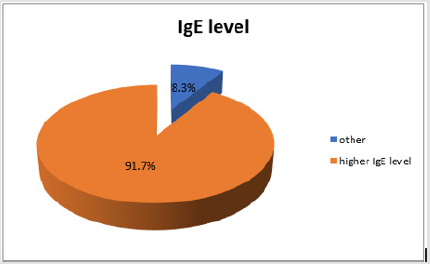
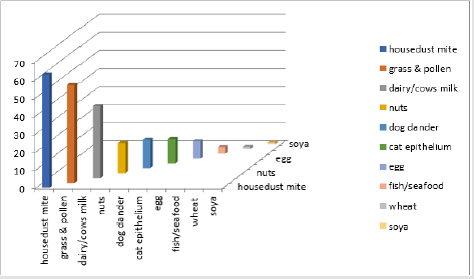
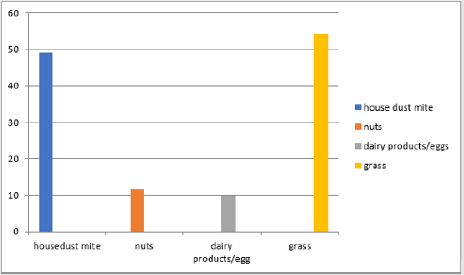
One hundred and thirty-three children with eczema were referred to the Royal Wolverhampton NHS Trust were tested. RAST test showed that 91.7% of children (122/133 patients) having high/abnormal figures for IgE level (Figure 1). Results of individual specific IgE level among those patients who tested positive (Figure 2) was as follows; house dust mite 62.7%, grass pollens 54.2%, dairy/cow’s milk 39.9%, nuts 16.7%, dog dander 15.9%, cat epithelium 13.6%, egg 9.7%, wheat 4.9% and fish/seafood 3.7%, wheat 1.2% and soya 0.9%. As for the severity level of IgE measured for the scoring levels above 52.50 (IU/ml), Grade 5 and 6 (Figure 3), house dust mite (49.2%), nuts (11.5%), dairy products/egg (9.7%) and grass (54.2%). In the moderate grading of severity (3.5-52.49 IU/ml) Grade 3 and 4 dairy products/egg (9.7%), nuts (9.7%), house dust mite (18.1%), cat epithelium (14.7%), dog dander (14.4%), wheat (3.1%) and soya all (1%). On follow up, a significant number of patients reported an improvement in their atopic dermatitis symptoms after introduction of allergen avoidance strategy.
Figure 1: Percentage of patients with atopic dermatitis showing high IgE level which is 122 patients out of the 133 who participated in this study.
Figure 2: This figure demonstrates the individual specific IgE levels among patients who tested positive for RAST testing.
Figure 3: This figure demonstrates the grade 5&6 severity positive RAST tests in the patients who were studied.
Discussion
The relationship of atopy, dermatitis and IgE mediated food allergy is not clear; neither extensive research has been conducted in the field. IgE mediated food allergy and atopic dermatitis prevalence peak at the first 12 months of life. The risk of atopic dermatitis in infancy increase by threefold with high levels of IgE sensitization to foods. Children with atopic dermatitis have higher prevalence of food allergy. IgE mediated food allergy affects 35% of children with moderate to severe atopic dermatitis and 6-8% of asthmatic children have wheezing which is thought to be food induced although 80% of those outgrow their food allergy [9]. In a recent study 27% of patients diagnosed with atopic dermatitis suffer from food allergy to wheat, soya, egg, peanuts and milk, while 32% suffer from sensitisation to these foods. Also, it found that food allergy, can act as a triggering factor in provoking and flare up of atopic dermatitis children in 7% [10]. Our study was aimed to evaluate the importance of carrying out RAST testing in patients with atopic dermatitis referred to the specialist secondary care hospital within the National Health Service in the UK. These patients usually moderate to severe grade as most of the mild cases are treated by General Practitioners in primary care. We found high population of these patients to have high total serum IgE levels at 91.7%. High severity grades of allergens specific IgE were also detected in these patients and this helped to guide patients to which specific allergen to avoid.
Despite the wealth of information in support of the link between IgE mediated allergy, RAST testing and atopic dermatitis a study showed that some patients with positive tests have no clinical manifestations of disease when exposed to the allergen [11]. Atopic dermatitis or eczema often occurs first in the atopic march or atopic triad of eczema, asthma and hay fever [12]. A positive for an allergen specific IgE measured by RAST indicates a sensitised state to the allergen which is not synonymous to a clinical diagnosis. The RAST results provided by our study helped to increase our ability to rank allergens according to their likely contribution to the symptoms of each patient. The significant reporting by atopic dermatitis patients in improvement of symptoms after avoiding the possible offending allergen gives promising evidence that specific allergen avoidance, guided by RAST, can contribute positivity in the management of atopic dermatitis. However, there still need to be further investigations and assessment to draw a conclusion.
Conclusion
RAST testing is an available tool in investigating and managing of atopic dermatitis. It has been undervalued and underestimated in the past. Our results demonstrated significant positive results to an association of severity of atopic dermatitis and the grade of allergen specific IgE antibody. Therefore, we recommend considering RAST testing to all those children with atopic dermatitis who failed first line of treatment.
For more Articles: https://biomedres01.blogspot.com/



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.