Introduction
The molecular targeted therapy started with introduction
of tyrosine kinase inhibitor (Imatinib) that selectively inhibit
phosphorylation of BCR-ABL protein with subsequent inhibition
of growth of BCR-ABL positive cells [1]. Imatinib was approved in
2001 as a first targeted therapy for treatment of BCR-ABL positive
chronic myeloid leukemia (CML) and in 2003 for treatment of ckit or CD 117 positive gastrointestinal stromal tumor (GIST) [2,3].
The safety and efficacy profiles of imatinib were explored in the last
decades and have been well known, the most common reported
side effect and dose limiting toxicity of imatinib was fluid retention
(FR) [4]. Manifestations of FR usually presented as mild periorbital and/or lower limbs (LLs) edema that was easily manageable
[5]. Development of sever FR manifested by marked subcutaneous
and LLs edema, ascites, pleural and pericardial effusions were
less frequently seen with imatinib treatment [6]. Due to rarity
of imatinib induced sever FR, we reported this case of imatinib
induced marked FR presented after long time of imatinib treatment
and was refractory to drug withdrawal and conventional treatment.
Case Report
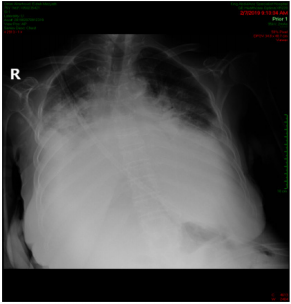
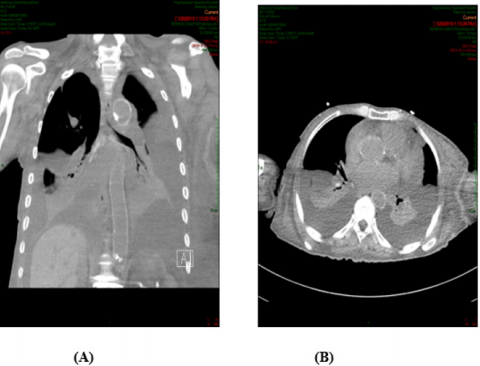
A 88-years old female with remarkable history for diabetes, ischemic heart disease, known case of CML for which she received imatinib for more than 10 years and still under treatment. This patient presented with two weeks history of gradually progressive breathlessness, mild cough associated with LL swelling and not associated with fever. The patient came to emergency department where ECG and echocardiography were normal apart from mild to moderate pericardial effusion, X-ray chest showed bilateral moderate pleural effusion (Figure 1) then patient was admitted for further evaluation and management. We asked for full investigations, CT chest showed moderate bilateral effusion more in the left side (Figure 2A) with mild pericardial effusion (Figure 2B), abdomino-pelvic ultrasound showed normal abdominal and pelvic organs with moderate free fluid in abdomen and pelvis, complete blood count, renal function tests, liver function tests and serum electrolytes are all within normal limits. Aspiration of both ascetic and pleural fluids was done and subjected to chemical, microbiological and cytological analysis which showed features of transudate with no growth of any organism. So based on history, clinical examination and investigations, all causes of generalized edema were excluded and the only explanation for development of this generalized FR was imatinib use. As the patient was in hematological and molecular complete response(CR) for last year, we stopped the imatinib and the patient was followed and treated symptomatically. We expected that the conditions of the patient will improved after imatinib withdrawal and diuretics, but there is no improvement after more than 3 weeks of stoppage of imatinib.
Figure 2: (A): CT chest showed bilateral pleural effusion more in the Lt side, (B): With minimal pericardial effusion.
Discussion
CML is a myeloproliferative disorder of hematopoietic stem cells with 1.5 per 100,000 population incidence rate every year in US and accounted for about 15% of all leukemia’s in adults [7]. The pathognomonic diagnosis of CML is established by presence of Philadelphia chromosome which resulted from reciprocal translocation (t9,22) to form ABL-BCR signal transduction tyrosine kinase protein [8]. Treatment of CML was revolutionized after development of imatinib which remain the 1st line therapy in all newly diagnosed CML [9], however, development of adverse effects of imatinib was observed and resulted sometimes in dose reduction or drug interruption. The course of imatinib associated FR usually developed acutely after short duration of drug administration and known as acute or progressive form or developed after longer duration of treatment and named intermittent or steady course characterized by chronic and persistent fluid accumulation [5]. Various studies reported long-term adverse effects of imatinib as cardiac toxicities, myositis, renal failure, secondary malignancy, multiple sclerosis, dermatitis, gynecomastia, pancreatitis, hypogammaglobulinemia, hypophosphatemia, opportunistic infections, cerebral edema, although some authors reported generalized edema in less than 10% of cases as a short term toxicities not long-term as in our study [10]. In most of case reports, the occasional or unusual forms of FR due to imatinib therapy usually resolved and improved after discontinuation of the drug [11]. However, in our case the condition not improved after imatinib cessation that we considered it as a prolonged refractory FR state.
Our explanation was that old age with presence of some comorbidities might be the aggravating factors for this prolonged and persistence of FR. Although chronic and prolonged generalized FR is unusual adverse effect of imatinib therapy, this case report should raise this issue for physician to be cautious during treating patients with imatinib and expect that FR may develop even after long-term duration specially if there is aggravating factors that trigger fluid retention and accumulation in the body elsewhere. Also, chronic mild FR either localized or generalized might progressed to refractory state not responding to cessation of the drug and diuretics. So, this case should raise the question for the need of more advanced monitoring systems either radiologically or sonographically to evaluate the cases under imatinib treatment periodically during the hall course of treatment and do not exclude the cases with long-term therapy not get FR as this side effect may develop at any time with mild form pass to chronic state that may not respond to treatment.



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.