Intervention of Dream Quality in the Appearance of Concomitant Symptoms in Hospitalized Patients
Introduction
When trying to define the dream it is inevitable to differentiate
the physiological characteristics in the good quality of sleep
depending on the species, where it is a little simpler to enumerate
the behavioral characteristics that are associated with the aspect of
the dream and try to define it properly, where it can be associated
with immobility and muscle relaxation, it is a reversible event
(which differentiates it from other pathological states such as
stupor and coma), decreased consciousness and reactivity to
external stimuli and finally during sleep individuals acquire a
stereotyped posture [1]. The absence of sleep induces different
behavioral and physiological alterations in addition to generating
a cumulative sleep debt that eventually must be recovered. A tool
that has been of vital importance for the study of sleep physiology
is the electroencephalogram (EEG), which is the graphic and digital
representation of the oscillations that show the electrical activity of
the brain, to be recorded by electrodes placed in different regions
of the head. During alert states while keeping the eyes closed on the
EEG, oscillations of electrical activity are observed that are usually
between 8-13 cycles per second, mainly in occipital regions (alpha
rhythm) [2]. Within the dream, characteristic changes of brain
activity occur. which is the basis for dividing the dream into several
phases, where it is usually divided into two phases: without rapid
eye movements, and with rapid eye movements
Sleep NOT MOR
Phase N1 corresponds to drowsiness or the onset of light sleep, light muscular jerks are usually observed (acute vertex waves), phase N2 appear specific patterns of brain activity, called sleep spindle and complex k, heart rate and respiratory begins to decrease gradually, phase N3 or slow wave sleep is the deepest phase observed in the EEG very slow frequency activity (<2 Hz).
MOR Sleep
Now it is called the R phase and is characterized by the presence of rapid eye movements, physically all muscle tone decreases [3- 5]. A young adult spends approximately 70-100 min in non-MOR sleep, which can last between 5-30 min and this cycle is repeated every hour and a half throughout the night, therefore throughout the night they can be presented normally between 4 and 6 MOR sleep cycles.
Sleep Hygiene
Sleep hygiene measures are a series of recommendations about desirable behaviors and habits, as well as modifications of environmental conditions and other related factors, aimed at improving the sleep quality of people who already suffer from a sleep disorder such as insomnia, or that can be used as measures to prevent a sleep disturbance [6,7]. Although there is no global consensus about what these sleep hygiene measures should be and some of these sleep hygiene measures are transplanted with some forms of non-pharmacological behavioral treatment we can generally consider (avoid prolonged naps> 1hr., lie down to sleep at the same time every day, wake up at the same time all day, sleep in a comfortable bed, sleep in a room with low lighting and little ambient noise).
Epidemiology
It is estimated that, in our country, around 45% of the adult population has poor sleep quality. The above is reflected in the difficulty that people have to get up, as well as in constant drowsiness and fatigue during the first hours of the morning.
Method
The present study uses the referential method as a basis, mentioning descriptive surveys, and testing the Pittsburgh quality of sleep scale in which 20 hospitalized patients are evaluated in the Regional Military Hospital of Specialties of Guadalajara, Jalisco, assessing the level of quality of sleep and what concomitant symptoms are added by poor sleep hygiene, February-May trial period [7-10].
Justification
The present investigation will focus on studying the hygiene habits based on the quality of sleep in hospitalized patients, since due to work stress or in hospital instances it has been seen that patients have directly modified their sleep habits, worsening the quality of life and By delaying the recovery in the hospital by increasing concomitant symptoms, we propose then to investigate the evolution of the pathological patterns and their aggregate symptoms; the reasons that led us to investigate the quality of sleep in hospitalized patients are due to the increase in discomfort or somnolence data reported by patients after staying more than 2 days in hospital. We think that by means of the detailed analysis we will be able to make the health personnel aware to improve the hygiene of the sleep thus helping the quick recovery without the appearance of concomitant symptoms in the patients who are hospitalized.
Goals
a) Clinically observe the behavior of hospitalized patients and their quality in sleep hygiene.
b) Intervening and preventing concomitant pathologies that are associated with poor hygienic sleep habits.
c) Improve the quality of life of hospitalized patients.
d) Awareness of the application of hygiene or good sleep habits to improve the quality of life.
e) Locate key events or outstanding problems in the quality of sleep.
Statistical Population
Sampling was done in which people of both sexes were chosen, who underwent a descriptive evaluation through direct surveys, where a sample of 20 people with characteristics with a simple random election type was collected, making a list of participants hospitalized to form the sample to be studied by means of questionnaires.
Results
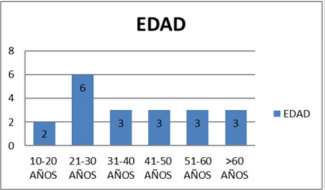
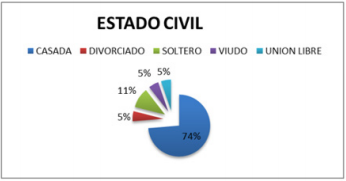
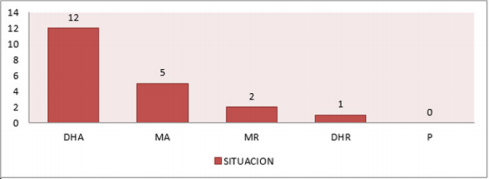
A random sample is taken to carry out descriptive direct surveys at the Regional Military Hospital of Guadalajara, Jalisco, where 14 people of the female sex and 6 of the male sex are taken, having a percentage of 70% female and 30% male. Regarding age, there is an ambiguous percentage where it is observed that 30% corresponds to people between 21 and 30 years of age following proportionally 15% of patients aged 31 to 73 years. In the marital status 74% of the respondents are married, 11% are single, and 15% are proportionally divorced, widowed and in free union (Figures 1-4). The descriptive surveys did not take into account the situations of right-of-way in the institution where the majority of those interviewed or those who were interviewed were the rightful claimants in the asset, having the majority percentage with 60% followed by military personnel in the asset where it was noted that most of the concomitant symptoms corresponded to anxiety and headache (Figure 5). Among the key questions that are characterized in the scale of Pittsburgh manifested bedtime where literally 50% of the patients interviewed reiterated to sleep at around 10:00 pm and 11:00 pm, while the rest were distributed with 25% who go to bed regularly from 08:00 pm to 09:00 pm and the other 25% after 12:00 pm (Figures 6-10).
Continuing with the variability of sleep habits, the question about the total time it takes to sleep is indispensable, where a detailed variability between each point and constant was obtained, obtaining as a result that 45% of the studied population reconciled sleep within the first 10 minutes, while 25% is distributed in patients who sleep within the first 30 minutes and an important fact is that 15% of patient samples last more than 60 minutes to fall asleep (Figure 11). It should be noted the relevance of the time that people take to sleep and the time they have to get up, since it should be noted that within the quality of sleep it is known that a young adult should sleep an average of 7-8 hours, although This amount may vary because it depends on internal factors of the organization and external society, so a preschool child can sleep between 11 or 12 hours and an older adult between 5 and 6 hours not taking into account the periods that doze during the day , so the results are very important in which the percentages of patients who wake up early and sleep late are focused as they begin to have functional and organic damages that are involved in their daily life. Within the Pittsburgh scale it is essential to highlight and highlight the following two patterns:
a) The time when patients regularly wake up from their dreams
b) The total hours of sleep of a patient.
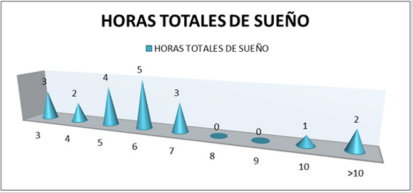
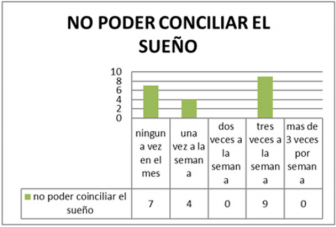
Where the results taking as supremacy that 40% of the studied population wakes up at 7:00 am while the other 40% wakes up on an average between 5:00 and 6:00 am to perform their activities, finally 15% It has a short sleep average waking up between 3:00 and 4:00 am (Figures 12-15). Performing and observing an average within the sleep habits and the quality of sleep of the patients a question is asked to evaluate the amount of hours that people sleep approximately, taking into account their basic pathologies (post-operative, chronic pathologies) degenerative, concomitant pathologies), with the result that 45% of patients only sleep 5 to 6 hours in a row compared to the time a person really has to sleep to refer adequate quality and hygiene of sleep is really low of established parameters, while around 15% of the patients who were taken as a sample sleep an average between 10 and 15 hours a day, it should be noted that these patients mentioned having psychological and psychiatric problems as depression, if we recapitulate the concepts offered by the national sleep foundation 85% of the patients interviewed do not meet the criteria to define that they maintain a to adequate sleep health, while only 5% of patients could enter the criteria already established and mentioned (in the following graph represents the number of patients and the total sleep hours they maintain for a day) the scale of Pittsburgh are observed questions which are worth mentioning that are subjective processes that take relevance in the last 4 weeks, about falling asleep where 45% of hospitalized patients answered that approximately three times a week they are prevented from falling asleep. a proper way.
And evaluating the number of people and how many times they get up during the night, results were obtained that 14 people of the interviewed women get up between 2 and 3 times a week, which is about 70% of the patients surveyed with those bad sleep habits. Regarding the reasons why patients wake up, the following result was obtained (Figures 15-18). Where 65% of respondents in the last month would not have suffered from feelings of shortness of breath, while the number of 6 people reported that three times in the week are awakened by feeling a sense of shortness of breath corresponding to a 30% of the sample investigated.
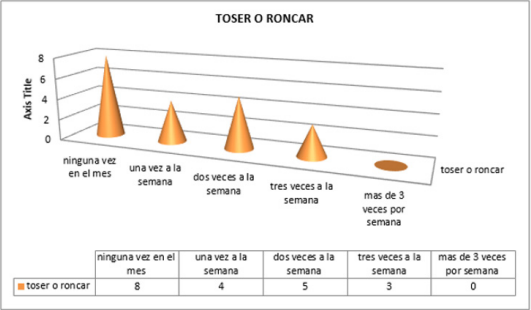
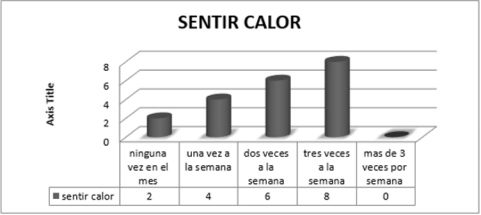
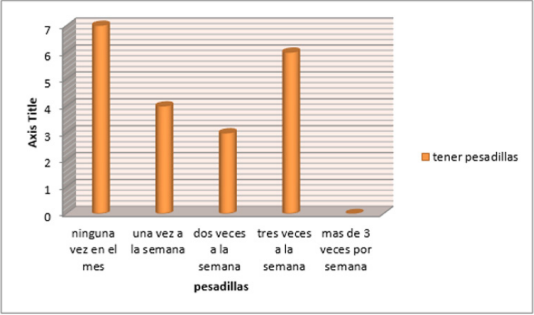
l ask indirect questions about if your family member snored 40% answered that they did not catch such events in the last 4 weeks while 45% answered that on average 1-2 times per week they snored at night what they did the patient will wake up during the night, 50% of patients have not woken up during the night due to cold in the last 4 weeks, and with a total of 5 patients it gives a result of 25% who woke up at least once a week due to cold sensation (Figures 19 & 20). Otherwise, 70% of patients used to wake up during the night due to the sensation of heat. 35% of the patients surveyed had as a result that they have not had problems like nightmares at bedtime, while the other 35% have nightmares 1 or 2 times a week, 30% 3 times a week; the following graph is representative of the results obtained when applying that question to the sample that was investigated.
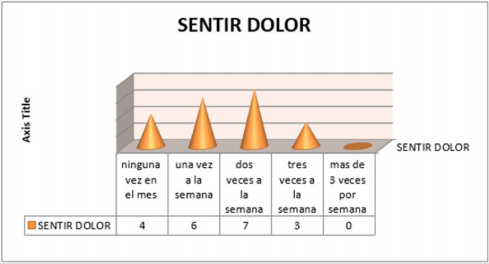
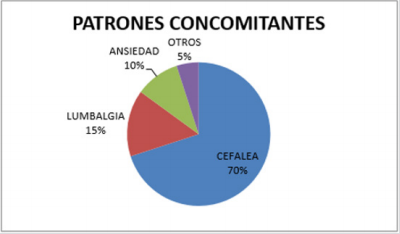
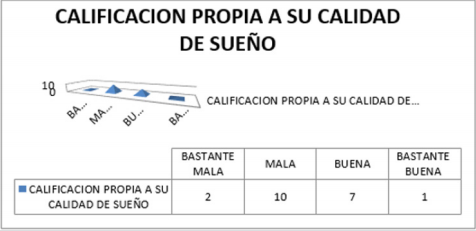
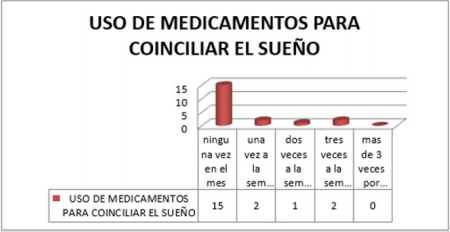
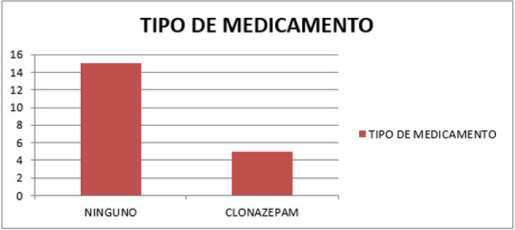
Among the data that we want to highlight in this study is the presence of pain and of what type in the last 4 weeks, referring to pain as some event that keeps them awake or that awakens them during the night, having as conclusion that the 30 % of the patients interviewed answered affirmatively that approximately once a week felt pain, and 35% mentioned that approximately twice a week felt some type of pain. Paulatively evaluating the data provided by the patients, it was obtained that 70% of the hospitalized patients have presented tension headache caused by bad habits or sleep hygiene, adding lumbalgia and even anxiety in a total of 5 more patients that correspond another 25% more of the sample studied. He was asked if they took any medication or taken in the last 4 weeks to be able to fall asleep, where 75% denied having taken medication to fall asleep. While the other 25% agreed to have ingested medication to be able to sleep either 1 to 3 times per week. The unanimous medication that 25% of patients used is clonazepam which is a benzodiazepine that acts directly on the central nervous system, which can create drowsiness and fatigue.
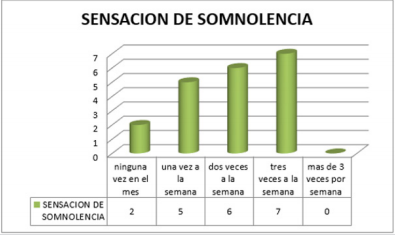
Within the study of sleep hygiene there is variability where it focuses directly on factors such as drowsiness that is directly caused by poor sleep hygiene habits, based on the Pittsburgh scale there is a direct section where questions about the drowsiness that the patient could suffer and finally if that drowsiness or fatigue could prevent the accomplishment of some daily activity, or executive in the day to day. Having as a result that 65% of patients have been in a drowsy status or have felt tired in an approximate period of between two times to three times a week, while only 25% of patients have drowsiness due to at least once a week, preventing their early recovery or decreasing their resistance in everyday life. Taking into account the number of patients who answered affirmatively to the question about sleepiness, a graph was obtained showing the results in which the disability or problem that caused the maintenance of that drowsiness status was shown, obtaining that 35% of the patients do not have no problem when carrying out their daily activities, while another 35% of the people surveyed expressed their concern and described as a slight problem in their daily lives the maintenance of somnolence data which can cause difficulties in their daily life; Finally, 25% classified their level of sleepiness as a moderate problem, defining that in daily activities it is a conflict to be able to perform them with the greatest aptitude and energy.









No comments:
Post a Comment
Note: Only a member of this blog may post a comment.