Asymptomatic Submucosal Lipoma of the Anal Canal: A Report of an Incidental Colonoscopic Finding in an Elderly Patient with Colonic Diverticuli
Background
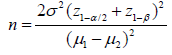
Lipomas are benign adipose tissue tumors commoner between
the ages 40 -60 years and have a preponderance in the male gender
[1]. They may be solitary or multiple, superficial or deep in location
and are usually asymptomatic. Cosmetic concerns (in larger
lipomas), pain or discomfort are the common indications for removal
of superficial lipomas and these commonly occur in the trunk, head
and neck regions. Deep-seated lipomas are relatively uncommon;
they occur in the thorax, retroperitoneum or abdominal cavity [2].
Intra-abdominal lipomas usually affect the omentum, mesentery,
the submucosa and subserosa of the gastrointestinal tract (GIT) [3].
Lipomas are the second most common non-epithelial benign GIT
tumours after leiomyomas [4]. The most commonly affected region
of the GIT is the colon, with the highest incidence at the cecum,
ascending colon, transverse colon, and the left colon (in decreasing
order as one approaches the rectum) [4]. Occurrence of a lipoma in
the anal canal is extremely rare with only one case reported so far
by Porta et al in 1979! [5].
In diverticulosis of the colon, there is a transmural outpouching of the colonic mucosa through an area of weakness. This mural weakness-the primary pathology in diverticulosis-is of multifactorial aetiology and the predisposing factors include weakened points of vascular entry into the colonic wall, reduced dietary fiber, hereditary factor, reduced physical activity and obesity [6]. In ventral abdominal wall hernias, stretching of abdominal musculature (because of an increase in its content as seen in obesity) and separation of muscle fibers with weakening of aponeurosis are known to weaken the integrity of the fascia leading to herniation [7]. Whilst the role of mural adipose tissue in the development of GIT diverticula is yet to be established, Yekeler et al have however reported a case of two coexisting rarities- an oesophageal lipoma that resulted in an oesophageal diverticulum due to extramucosal impact of the lipoma [8]. We present an interesting incidental finding of a submucosal anal lipoma in an elderly man who had a concomitant presence of colonic diverticula with an increased submucosal adipose tissue in the vicinity of the diverticuli. This case is reported in line with the SCARE criteria for case reports [9].
Case Presentation
A 70-year-old male retiree was referred for colonoscopy
on account of recurrent passage of bloody stool of three months
duration, last episode being two weeks earlier. He had no history
of anal pain, discomfort, or anal protrusion. There was no change
in bowel habit, reduction in stool caliber, melaena, abdominal pain
or tenesmus. There was no history of anorexia, haematemesis,
early satiety and he does not have a history of peptic ulcer disease.
He had no fever, weight loss or any comorbid illness. He had no
history of anal trauma or previous anal surgery. No personal or
family history of similar illness or malignancy in the past. He was
not on any anticoagulation. On examination, he was pale, otherwise
other aspects of his general and systemic examinations were
normal with a body mass index of 23.1 kg/m2. A pre-procedural
rectal examination did not reveal any abnormality. Colonoscopy
revealed multiple diverticuli in the caecum, ascending colon and
descending colon (Figure 1a) with a 5mm x 3mm sessile polyp in
the descending colon.
There was a yellowish, oval, submucosal sessile mass (about
10mm x 8mm in widest diameters) with a lobulated surface, about
3cm from the anal verge (Figure 1b). The mass exhibited positive
pillow or cushion sign. The mucosa of the transverse colon, sigmoid
colon (Figure 1c) and rectum was normal. However, there was an
increased yellowish hue to the large bowel submucosa around the
anal canal (Figure 1d) and the sites of diverticula (Figure 1e). No
stigmata of recent bleeding were seen. The descending colonic
polyp was removed with cold biopsy forceps (Figure 2a). The anal
submucosal mass was biopsied revealing the characteristic naked
fat sign (Figure 2b). The anal submucosal mass was reported to
be benign at histology while the descending colonic polyp was
reported as an adenomatous polyp with low grade dysplasia. He
has been on conservative care for the colonic diverticulum and has
remained asymptomatic both for the diverticulum and the anal
submucosal lipoma 3 months post colonoscopy.
Discussion
Lipomas are common benign tumour of mature adipose tissue
that usually occur in superficial locations – most common location
being subcutaneous. The relatively uncommon deep-seated
lipomas either present atypically or as incidental findings [10]. In
the GIT, they are usually subserosal or submucosal in location, the
colon being the most affected region. Involvement of the rest of
the large bowel decreases anal-ward. We presented an extremely
rare report of a submucosal lipoma of the anal canal with a curious
finding of concomitant existence of divertculi at areas of increased
submucosal adipose tissue. We discuss this case in terms of rarity
and then, its peculiarities. The rarity of this case lies in the fact that
it is a deep-seated lipoma occurring in the anal canal. The most
distal GIT lipomas reported in the literature are those of the rectum
and these presented as polypoid submucosal masses protruding
through the anal canal or casuing rectal bleeding [11,12]. Beyond
the rectoanal canal, the perianal region, lipomas are also rare with
a report of a perianal lipoma occurring years after surgery for a
perianal abdscess [13].
The aetiology of the perianal lipoma was likely traumatic,
similar to the report by Uscilowska et al on para-anal lipoma
resulting from perineal trauma [14]. Beyond trauma, the other risk factors for lipoma formation include genetic predisposition,
obesity, hyperlipidaemia and diabetes mellitus [15]. There risk
factor for lipoma in our patient was not apparent. This was not a
surprise since such deep-seated lipomas are incidentalomas like
in our patient. Colonic lipomas are usually asymptomatic except
when they are larger than 2cm, torsed, or pendulated. The small
size, submucosal location and sessile nature of the lipoma in our
patient may explain the asymptomatic nature. The sigmoid colon
is said to be the commonest site of colonic diverticulosis, although
a study on our patient population by Akere et al revealed right
colonic preponderance [16,17] The endoscopic appearance of
most colonic diverticuli is that of an outpouching of the mucosa
with an otherwise pink-looking mucosa/submucosa due to the
rich vasculature of these layers. In diverticulitis, the mucosa of the
diverticulum is reddened with or without a surrounding fibrinous
slough [18].
The peculiarity of our report is the increased submucoal
adiposis in the vicinity of colonic diverticuli, with a predominantly
yellowish (than pink) hue to the mucosal color (Figure 1e). These
diverticuli involved the caecum, ascending and descending colon
with none in the sigmoid colon, the mucosa of which appeared
normal (Figure 1c). It therefore stimulates curiosity as to a possible
link between increased large bowel mural adiposi and a possible
predisposition to subsequent diverticulum formation in the areas
where these adipose tissues are located. The plausibility of this
link may not be far-fetched if the underlying pathology of colonic
diverticulum- mural weakness-is considered. It is therefore more
compelling to associate increased submucosal adiposis in our
patient with his colonic diverticuli considering the established
effect of same adipose tissues on tougher tissues like aponeurosis in
abdominal wall hernias. Whilst colonic diverticulosis is commoner
in older patients like our patient, Brouland et al reported a large
colonic diverticulum in a young male arising due to colonic mural
weakness by multiple colonic lipomatosis [19].
The risk factors for colonic diverticulosis include comorbidities
(like hypertension and diabetes mellitus), increased luminal
pressure (from colonic dysmotility, reduced dietary fiber), genetic
risk factors (like Ehlers-Danlos syndrome, Coffin-Lowry and renal
polycystic disease), obesity/reduced physical activity, smoking
and increasing age [20]. Age alone may not explain the diverticuli
seen in our report and none of the other known risk factors was
apparent. Although the endoscopic features of the submucosal
anal mass we reported were in keeping with a lipoma, histological
report did not show the presence of adipocytes. This is a common
limitation of endoscopic biopsies where only the mucosal layer is
usually biopsied except multiple biopsies are taken at the same
spot to include deeper layers. A limitation of this report is our
inability to do endoscopic ultrasound which would have confirmed
the location of the lipoma. Facility for endoscopic ultrasound is not
available in Nigeria as at the time of this report to the best of our
understanding.
Conclusion
Lipomas of the anal canal are rare. Although an incidental
endoscopic finding in this report, coexistence of large bowel
lipomas with increased submucosal adiposis in the vicinity of
colonic diverticuli may suggest an aetiological role of such lipomas
in colonic diverticulosis.
For more Articles on : https://biomedres01.blogspot.com/

No comments:
Post a Comment
Note: Only a member of this blog may post a comment.