Contributions from the Autonomous University of Zacatecas in the Epidemiology, Diagnosis and Treatment of Trichinellosis, 1986-2021
Introduction
In Mexico, the first reports of Trichinellosis were by Dr. Olvera
in 1896 [1], later by Dr. Perrin in 1939, and Dr. Mazzotti carried
out the first epidemiological studies in 1943 [2]. The latest reports
from the national health secretary are those obtained from 1990-
1994, 2000-2002, 2014, 2015 and 2016, with a total of 1122 cases,
the states with the highest number of cases from 1990-2016 were:
Hidalgo 216, Chihuahua 113, Veracruz 81, Jalisco 76 and Oaxaca 55,
Zacatecas no cases have been reported since 1994, and from 1990-
1994 40 cases were reported [3].
Zacatecas is a state of the Mexican Republic located in the north
of the country, it has an area of 75,275.3 Km2, a population density of
21.5 inhabitants / Km2 that represents 3.8 of the national territory
and with a population of 1,622,138 inhabitants. distributed in 58
municipalities being the most populated Guadalupe, Zacatecas and
Fresnillo, which represents 1.3% of the national population. There
are 95 men for every 100 women. 59.4% have basic education,
77.5% have piped water, 96.3% have drainage, 99.3% electricity,
79.7% have some medical safety regime. The economically active
population is dedicated to agriculture, livestock, mining, services
and industry [4]. The Autonomous University of Zacatecas (UAZ)
is considered the civilizer of the north, it was founded in 1832, and
its autonomy was in 1968, which currently has an approximate
population of 40 thousand students and 6 thousand teachers and
administrative personnel UAZ 2020.
Trichinellosis was detected for the first time in Zacatecas in
1975, and 4 outbreaks were reported in 1978, the most significant
being that of Laguna de Carretero (Municipality of Villanueva), with
a fatality of 33%, from 1979-1988 17 outbreaks were reported.
The most important being Valparaíso (with one death), and Pozo
de Gamboa where a 20-year-old pregnant woman lost the product.
Trichinellosis was found to be more frequent in urban than rural
areas, the age group from 15-44 years being more affected (49% of
cases) and referring to sex 1: 1.8 male / female. Zacatecas currently
has 58 municipalities and Zacatecas, Villanueva, Valparaíso,
Panucho, Jerez, Jalpa and Guadalupe were affected at that time, and
the transmission route was due to the consumption of poorly sewn
chorizo, the diagnosis was by direct plate compression techniques,
that received the name of trichinoscopy, and by the indirect
technique of micro immuno-diffusion-double [5]. The objective
of the present work is to make a report of the work carried out in
this parasitosis during the period of 1986-2021 in the Autonomous
University of Zacatecas.
Materials and Methods
a) Implementation of experimental models, murine (Balc / C
mouse, Long Evans rat), domestic dog, rabbit, York pig [6-13].
b) Characterization of the life cycle of Trichinella spiralis
[11,14,15].
c) Establishment of direct techniques (plate compression,
artificial digestion, and hematoxylin / eosin) and indirect
(double microimmunodiffusion, Dot-ELISA, IFI, Western Blot,
intradermal reaction) for the diagnosis of Trichinella spiralis
[16-23].
d) Evaluation of albendazole in a murine and pig experimental
model, its evaluation with 3, 5, 7, 10, 14 days of treatment. In
the initial phase of the infection, in the intestinal and muscular
phase [11,23,25,26].
e) Evaluation of albendazole in pregnant rats, with the same
treatment days [27].
f) Evaluation of the total antigen of Trichinella spiralis in murine
and pig models, and of the 45 KDa band in murine models. In
the intestinal, muscular phase and after 30, 60, 90 and 120
days of immunogen application. The purpose was to evaluate
the modifications of the T. spiralis nurse cell in Long Evans
rats immunized with total soluble antigen of T. spiralis and
sacrificed at different times. We worked with 25 male rats
of 2 and a half months of age, immunizing 20. Subsequently,
the 25 rats were challenged with infected T. spiralis meat,
sacrificing 5 rats every month, plus a control rat per 4 months,
when sacrificing them, direct plate compression techniques,
artificial digestion and the hematoxylin-eosin technique were
performed; indirect MIDD and Western Blot techniques were
performed on the sera [11,26,28-32].
g) To evaluate the protective effect of Trichinella spiralis Total
Soluble Antigen combined with bacterial vaccine and VITS
via sublingual route in Long Evans rats and to evaluate
Lactobacillus casei and VITS in intestinal infection by T. spiralis
in a murine model [11].
h) In all treatment models, groups of 5 animals were used, the
healthy control, Trichinella spiralis infection control, and the
different groups according to the treatment, and direct and
indirect techniques were performed. And the results were
analyzed by statistical analysis of ANOVA or Student’s t test.
i) Epidemiological studies in humans, pigs, dogs, and domestic
rats for the detection of Trichinella spiralis, by indirect
techniques of double microimmunodiffusion, Dot-ELISA and
Western Blot [33-35].
j) Evaluation of a Diagnostic Kit by Dot-ELISA for detection in the
field.
Methodology
Used in the experiments were obtained from the animal facility
of the Academic Unit of Biological Sciences of the Autonomous
University of Zacatecas.
The parasite (Mexican strain) was identified with Edoardo Pozio
PhD, in the Istituto Superiore di Sanita in Rome, Italy 2000, and has
been maintained by serial passage in mice and rats since 1986 at
the Laboratory of Cell Biology and Microbiology at the Academic
Unit of Biological Sciences from the Autonomous University of
Zacatecas, Mexico. All the animals were maintained in controlledtemperature
rooms and fed with rodent balanced food [6,13].
Ethical Approval
This study was reviewed and approved by the Bioethics Committee of the Biology Faculty of the Autonomous University of Zacatecas, in accordance with the Official Mexican Norm (NOM-062- ZOO-1999), published by the Secretariat of Agriculture, Livestock, Rural Development, Fisheries and Food (SAGARPA) in the Official Gazette of the Federation (Mexico) on June 28, 2001 [13].
Direct Techniques
Plate Compression Technique
For the plate compression technique, approximately 5 mg of tissue were used (diaphragm, masseter, tongue, intercostals, leg), each sample was placed between 2 lamellae and compressed, occupying an area of 1 x 5 mm, it was observed to the optical microscope, with the 10x and 40x lens [10,11,33,36, 37].
Artificial Digestion Technique
30 g samples were used of homogenized tissue, and they were incubated at 37 °C, in a sack-shaped tulle sieve, suspended in a 0.3% solution of pepsin (10,000 U) and 37% HCl (0.2M) in 500 ml of distilled water, inside a separating funnel; 24 hours later, the larval package was separated with the ILs, which were deposited at the bottom of the funnel, observed in a newbawer camera under an optical microscope with a 10X lens, and the larval package was quantified [7,25,36, 38].
Hematoxylin-Eosin Staining
Hematoxylin-Eosin (H-E) stain. Leg, tongue, and diaphragm samples were taken from each experimental model. The tissues were fixed in 10% buffered formalin for 24-48 hours. Subsequently, they were transferred to 70% ethyl alcohol for automatic processing for approximately 12 hours in two steps of 70% OH, 80% OH, 96% OH, 100% OH and xylol. From this last step, the samples were removed and embedded in paraffin, forming support blocks for making 5-8 μm thick histological sections on a Leica Model 820 microtome. The sections were placed in a float bath at 50 °C and they were lifted on a slide to dry, deparaffinize for an hour in an oven and then go on to the staining process with the Hematoxylin and Eosin technique according to the criteria of Viloria [28].
Indirect Techniques
Double Microimmunodiffusion Technique (MIDD)
For double immunodiffusion, a 1% agar gel was made in distilled water with sodium azide, to avoid contamination; It was placed in an amount of 4.5 mL at 55 °C on a glass slide, once in solid form, the rosette was formed with a hole-hole, ensuring an equidistance of 0.5 cm between well and well; the comparison was carried out by always placing the antigen in an amount of 10 μL (10 μg) in the center and, around it, a serum of known reactivity, (in the same proportion by undiluted volume), leaving at room temperature environment in a humid chamber for 24 to 48 hours, until precipitation lines are observed between the positive serum and the antigen; then the gel was stained with Coomassie brilliant blue G 250, 25% by volume [10].
Dot-ELISA
Several nitrocellulose papers were squared, depending on the number of samples to be used, each 1 cm2 square a 10x5 cm paper. The antigen was placed on the undiluted paper placing the equivalent of 10 μg / μL, then it was allowed to dry at room temperature and once dry, it was proceeded to block with 3% fat-free milk in PBS this for 18 hours. Once the blocking time had concluded, it was washed once with PBS 0.5% Tween 20 for 10 minutes and 2 consecutive times with PBS for 10 minutes each time, then, 10 μL of each test serum was placed in each square and incubated again with 3% fat-free milk in PBS for an hour and a half, at the end of this time we proceeded to wash again with PBS 0.5% Tween 20 for 10 minutes and 2 consecutive times with PBS for 10 minutes, then the second antibody, Anti-IgG, Anti-IgM or Anti-IgA at a concentration of 1: 2000 in PBS conjugated with peroxidase, 10 μL of the second antibody and allowed to dry at room temperature, once dry it was incubated once more with Milk 3% fat free in PBS for an hour and a half and the container containing the paper was completely covered with aluminum foil. At the end of the hour and a half, the paper was washed with PBS Tween 20 at 0.5% for 10 minutes and 2 consecutive times with PBS for 10 minutes. The paper was then developed with 3,3-diaminobenzidine DAB, using 37% hydrogen peroxide as substrate [11,19,27].
Indirect Immunofluoresence (IFI)
The infective larvae (IL) were obtained from the rat muscle infected with T. spiralis, 20 μL of IL were taken and washed for three periods with PBS for 5 min in magnetic stirring, they were incubated with 20 μL of the first Ab with a 1: 100 dilution for 45 min with PBS, they were washed with PBS on 3 occasions for 5 min in magnetic stirring, the liquid was extracted with care to avoid absorbing the LI, 200 μL of the monovalent anti-gamma-fluorescein conjugate was added (IgG dilution 1: 1000), it was incubated for 45 min at 37 °C, the liquid phase was extracted, 3 washes were carried out with PBS in magnetic stirring for 5 min each, lamellae were mounted with the IL, covering them with cover objects and sealed with resin, they were observed under a confocal microscope [38].
Western Blot (WB)
The product obtained from the polyacrylamide gel run was transferred to NC paper [17], using the Transblot-Cell camera (Bio- Rad) at 35 volts, overnight at 4 °C. The NC paper was dyed with fast green for 5 min. With constant stirring, the dye was removed and decolorized in distilled water, to verify protein transfer, it was allowed to dry and the strips of the approximate width of each lane (0.5 cm) were cut. After the above, each strip was covered with a solution of PBS-3% milk powder and 0.15% sodium azide at 4 °C, with constant stirring overnight. They were then washed 3 times for 10 min. with PBS, incubation was continued for 1.5 h. with the sera of the rats in a dilution of 1: 100 in PBS-3% milk powder at 37 °C with constant agitation, subsequently they were washed twice with PBS-0.3% Tween 20 for 10 min and three more with PBS for another 10 minutes. Then, they were incubated with the second anti-rat IgG antibody, conjugated with peroxidase 1: 2000 PBS-3% milk powder for 1 h., At room temperature, with shaking, then they were washed 2 times with PBS-Tween 20 at 3% and rinsed with PBS, for 10 min. The Banding pattern of each strip was developed with 3,3´ di amino-benzidine (DAB), 50 mg in 100 mL of PBS, using, as a substrate, 37% hydrogen peroxide [39].
Intradermal Reaction (IDR)
Intradermal reaction was applied with Total Soluble Antigen of T. spiralis which were 10 units (10 μg of protein), the area of application of the AST was observed at 2, 24 and 48 hours [17,11].
Obtaining Immunogens
The antigen of T. spiralis was obtained, by means of extraction with liquid nitrogen, the infecting larvae were obtained by the artificial digestion technique, liquid nitrogen was added in sufficient quantity to cover the IL and by bursting the exit of antigenic components were centrifuged at 3500 rpm for 1.5 hrs. The supernatant was the soluble antigen of T. spiralis, whose protein concentration was determined and used in the different immunological tests, and as an immunogen (secretion / excretion antigens) in protection studies [6,7, 18,19,11,36].To determine that the antigen had the adequate protein concentration, a standard curve was obtained using bovine serum albumin, according to the methodology of Bradford, 1976, adjusting the concentration of proteins obtained to an optical density of 610 nm using Coomassie blue at 0 .06 % prepared in 2.2% HCl. The value of the optical density of the antigen was interpolated, to that of the standard curve of albumin, the concentration of proteins contained in the two types of antigenic extract was obtained [18].To obtain the immunogenic protein of 45kDa, the AST was subjected to polyacrylamide gel electrophoresis to separate by molecular weight (MW) the proteins that were identified by a PM marker of the 45kDa protein and by elution of bands the required protein was obtained.
Results
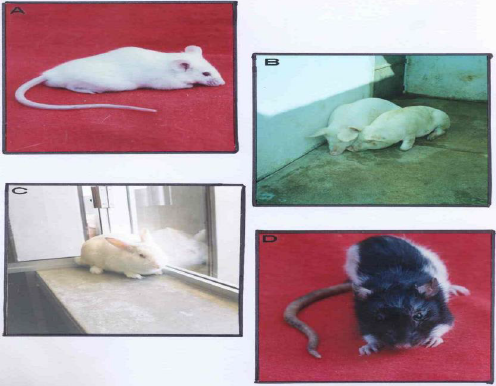
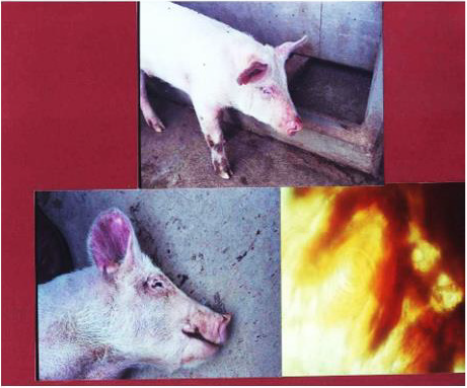
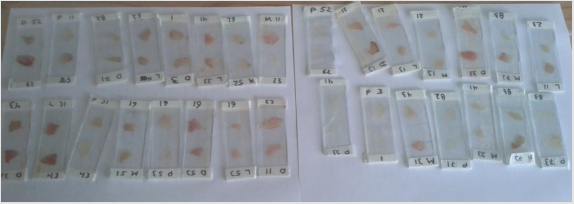
The experimental models of infection were implemented in a murine model, Balb / C mouse, Long Evans rat, domestic dog, rabbit, York pig (Figure 1), in all there was the reproduction of the infection and the life cycle, handling an IL per gram of weight. It was in pigs that we observed the clinical picture of the disease: diarrhea in the intestinal phase, and in the systemic and muscular phase: eyelid edema, joint injury, increased temperature. At sacrifice, IL was detected in muscle and brain tissue (Figures 2 and 3).
Figure 1: Experimental models used: Balc / C Mouse, York Pig, New Zealand Rabbit and Long Evans Rat. Material obtained in the Laboratory of Cell Biology and Microbiology UAZ.
Figure 2: The York pig is shown, which presents joint lesions, eyelid edema, skin erythema, and presents an increase in temperature. Upon sacrifice in the brain, IL was observed under a 40X light microscope and hemorrhage around it, by the plate compression technique. Material obtained in the Laboratory of Cell Biology and Microbiology UAZ.
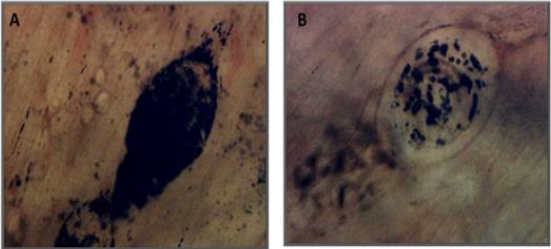
Figure 3: Compression image of the brain plate shows an IL with hemorrhage under a 40X optical microscope, and another in its cyst, but not as we usually see it in muscle. Material obtained in the Laboratory of Cell Biology and Microbiology UAZ.
Characterization of the Life Cycle of Trichinella Spiralis
The 3 stages of Infective Larvae (IL) were observed in muscle,
male and female adults in intestine and Newborn Larvae (NL) in
intestine and muscle.
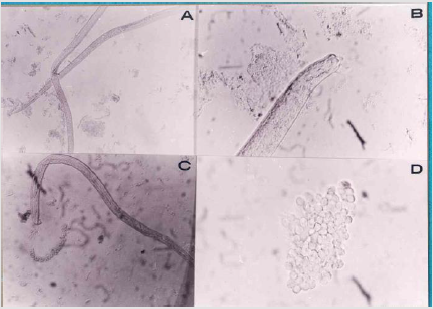
Male and female adults (Figure 4), technical observation of
plaque compression and the small intestine was performed with
the Fernandez Balls Technique (Figures 5&6).
Figure 4: Life Cycle, the male and female adults are observed in the upper part, and in the lower part the female, which is in the pregnant stage, under an optical microscope of light at 10X. Material obtained in the Laboratory of Cell Biology and Microbiology UAZ.
Figure 5: Obtaining adults by Bolas Fernandez technique, in A) Appearance of male and female adults, B) Male and its copulatory organ is observed, C) Expulsion of spermatozoa, D) Non-cialiated spermatozoa of Trichinella spiralis male. Observed under a 40X light optical microscope. Material obtained in the Laboratory of Cell Biology and Microbiology UAZ.
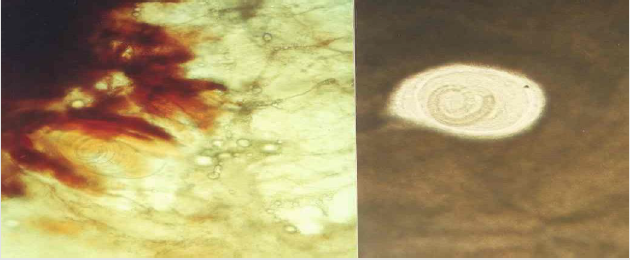
Figure 6: Plate compression technique observed under a 10X light optical microscope, IL of T. spiralis in its cyst or nurse cell, in the images there are from 1 IL to 6 in a single cyst, in the model where we observed a higher number was in the one with the York pig. Material obtained in the Laboratory of Cell Biology and Microbiology UAZ. Muscle tissue, Infective larvae finding from 1 to 6 in a single cyst (Figure 6).
Direct Diagnose Techniques
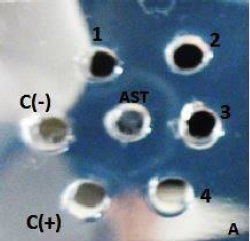
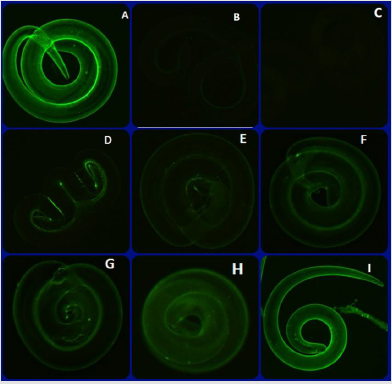
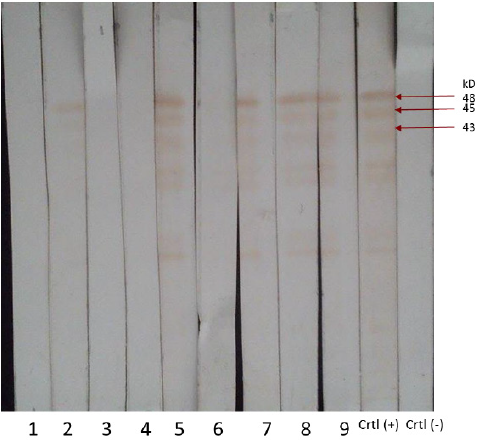
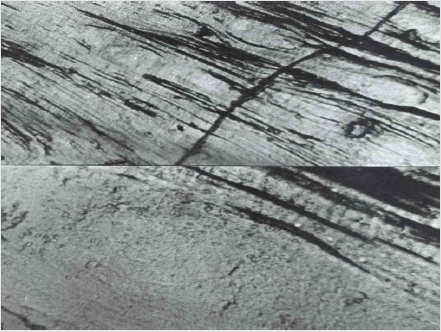
In all the experimental models by plaque compression (Figure 7), artificial digestion (Figure 8) and the Hematoxylin-Eosin technique, IL from Trichinella spiralis (Figure 9) were observed. Indirect Techniques: Indirect techniques, double microimmunodiffusion (MIDD, Figure 9.), Dot-ELISA, Immunofluorescence (IFI, Figure 10), Wester Blot (WB, Figure 11) and Intradermoreaction were positive, in WB a triplet of 42,45 and 48 kDa. The intradermal reaction is effective from the first month of infection with T spiralis, which is a very timely diagnosis for the pig without the need for a specialized infrastructure, as well as being inexpensive and can easily be carried out to the field with simple animal handling and not very aggressive, with a presumptive diagnosis after 2 hours of application of the intradermal reaction and confirmatory after 24 and 48 hours, which can prevent infection in man and even other animals in a timely manner
Figure 7: Plate compression technique. Material obtained in the Laboratory of Cell Biology and Microbiology UAZ.
Figure 8: Shown in A) Separation funnels, with meat in digester solution in an incubator at 37 degrees centigrade. B) Conical tubes with a Trichinella spiralis IL bundle at the bottom. Material obtained in the Laboratory of Cell Biology and Microbiology UAZ.
Figure 9: MIDD 1,2,3,4 positive sera from the murine model are shown, the positive and negative control, it is a specific technique with low sensitivity, but useful in research and massive sampling. Material obtained in the Laboratory of Cell Biology and Microbiology UAZ.
Figure 10: The IFI technique is shown, observed under a 100X confocal microscope, A) Trichinella spiralis positive serum B) and C) negative sera, D), E), F) positive sera from a murine model, G) positive serum from a domestic dog model, H) and I) positive sera of the York pig model, with IgG type immunoglobulin. Material obtained in the Laboratory of Cell Biology and Microbiology UAZ.
Figure 11: It shows 1,3,4 negative murine model sera, 2, 5 and 6 positive murine model sera, 7, 8 positive sera from York pig model, 9 positive serum from dog, and positive control serum for Trichinella spiralis and negative control serum of the murine experimental model. In the positive ones, the triplet of 42,45 and 48 kDa is observed. Material obtained in the Laboratory of Cell Biology and Microbiology UAZ.
Evaluation of treatment with albendazole, it was effective from
day 7, 10 and 14, both in intestinal and muscular phase (Figure 12),
murine and pig models, being statistically significant compared to
the infected control without treatment with a -P <0.001, by ANOVA,
when evaluating the parasite load by artificial digestion.When
performing the trypan blue technique to see viability of the IL
obtained from the digestion, they were dead, there was penetration
of the dye.
Albendazole evaluation in pregnant rats, phenotypic
modifications were observed from day 3 of treatment, being more
important with 14 days of treatment (Figure 13).
Figure 12: A plate compression technique is shown under a 10X light optical microscope, A) shows with 14 days of albendazole treatment, B) shows with 10 days of albendazole treatment in a murine model. Material obtained in the Laboratory of Cell Biology and Microbiology UAZ.
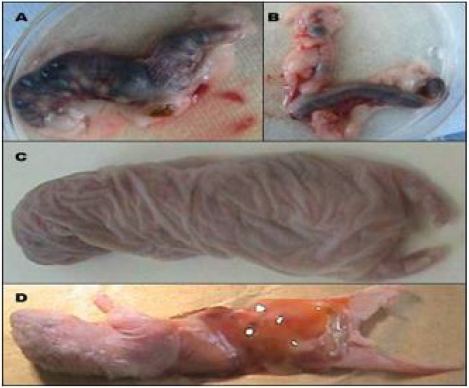
Figure 13: A) and B) Uterine horns obtained from rats with 15 days of Tx. C) Image of a dead rat with alterations in the spine and extremely dehydrated and lax skin. D) ventral image of the rat showing the absence of vital organs in both the thoracic and abdominal cavity. Material obtained in the Laboratory of Cell Biology and Microbiology UAZ.
Evaluation of the Total Soluble Antigen of Trichinella spiralis in Murine and Pig Models
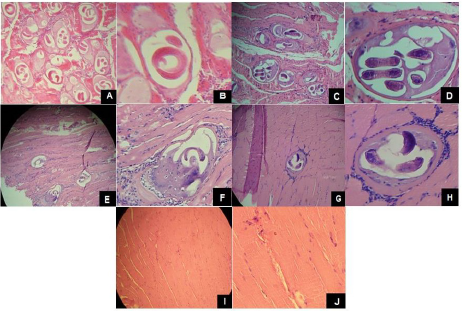
A statistically significant protection effect was observed in muscle phase, by analysis of variance p <0.0001. (Figure 14), in relation to the infection control group.When evaluating the T. spiralis implant at 30, 60, 90 and 120 days it is observed how the recovery of the tissue occurs, The modifications in the nurse cell of T. spiralis in tissues of Long Evans rats immunized with AST and sacrificed in Different times were evident with the direct techniques of C / P, D / A and H / E staining (Figure 15), it is observed how the encystment is lost and the spiral is no longer viable, being statistically significant with a value of P < than 0.01. By ANOVA.
Figure 14: Compression tissue is shown on a plate, where the IL of Trichinella spiralis is not found, in the super part observed with the 40X optical microscope the empty cyst and in the lower part at 100X the absence of the IL of Trichinella spiralis is confirmed spiralis. Material obtained in the Laboratory of Cell Biology and Microbiology UAZ.
Figure 15: The Hematoxylin-Eosin Technique is shown, in A), B), C), D) the Trichinella spiralis implant observed under an optical light microscope in unimmunized animals, E) at sacrifice 30 days after immunization , F) at sacrifice 60 days after immunized, G) at sacrifice 90 days post immunized at 10X, H) at sacrifice 90 days post immunized at 40 X and I) and J) at 120 days where already The nurse cell of T.spiralis is not observed, post immunization. Material obtained in the Laboratory of Cell Biology and Microbiology UAZ.
Evaluation of the Soluble Antigen of T. Spiralis, VITS, Bacterial Vaccine and Lactobacillus Casei
The administration of commercial Lactobacillus casei confers protection at the intestinal mucosa level in T. spiralis infection. Furthermore, based on the results obtained, administering a treatment in the early stages of the infection protects the host against infection by this parasite. The administration of an immunomodulator (VITS) and treatment with commercial Lactobacillus casei promotes a potentiated immune response by producing a greater degree of intestinal mucosa. Immunization with VITS in the experimental model prepares the organism to act against the parasite with a greater degree of effectiveness, thus observing an effective immune response against T. spiralis. An ANOVA statistical analysis was performed with the GraphPad Prism 6 program using the parasite loads obtained from the artificial digestion of each individual and with 95% confidence, resulting in that the groups treated with VITS, Bacterial Vaccine, Lactobacillus casei and soluble antigen of Trichinella spiralis compared to the infection control had a P <0.0001.
Epidemiological Studies
From the sampling of 1096 sera from backyard and technical
farm pigs from various municipalities of the state in 1998, an 8%
incidence of Trichinellosis was found, the Dot ELISA technique for
its diagnosis being reliable and affordable .A study was carried
out in pigs in the municipal slaughterhouse of Zacatecas, Jerez,
and Ojocaliente in 2006, where 85 samples were obtained from
each of them, taking 15 grams of masseter which was analyzed
by compression and artificial digestion, resulting in 2 positives.51
languages of dogs collected in the Department of Pharmacology of
the Academic Unit of Human Medicine and Health Sciences, of the
UAZ, 3 (5.82%) were positive with infection with T. spiralis, which
allows defining that the parasite is found in domestic dogs, more
often than you might think. In 2002.Analysis of 100 diaphragms
of domestic rats and serum from the municipal garbage dump of
Zacatecas. Diagnosis by direct techniques of compression and
artificial digestion and indirect by MIDD, WB, Results: Trichinella
spiralis was detected in 3 diaphragms of domestic rats by direct
compression and artificial digestion technique, and by indirect
MIDD and WB techniques. In 2006.A study was carried out on
3490 open population sera, of which 640 correspond to sera from
children under 15 years of age and 2850 from adults, which were
analyzed using MIDD techniques, presenting. In human sera from
the Zacatecas Health Center, Zacatecas in 2006, 3 positives were
detected by MIDD and WB with a predominance of the triplet of
42,45 and 48 kDa, From the 2008 Guadalupe Zacatecas Health
Center, 12 were positive by MIDD, Dot-ELISA and IET techniques
with a predominance of the 42,45 and 48 kDa triplet, examining
1209 human serum samples.
In human sera from the open child population of the Calera
Zacatecas Health Center, from 2011, 3 positives were detected by
MIDD techniques, and 12 by Dot-ELISA and IET with a predominance
of the triplet of 42,45 and 48 kDa. Ninety-two sera were collected,
which were evaluated using the indirect techniques of MIDD, Dot-
ELISA and WB, from a technical high school in Fresnillo and 2 were
positive by the three techniques in 2017.
Diagnostic Kit
Diagnostic kit based on the Dot-ELISA technique for which a murine model infected with different parasite loads from five to 1500 infective larvae (IL) of T. spiralis was used. The Dot-ELISA technique shows sensitivity from the second week after infection with T. spiralis IL. When making modifications to this technique, a non-significant difference was observed compared to the standardized technique. The objective of making the Trichinellosis Diagnostic Kit in the field was met. Which decreased time and steps. The statistical analysis was carried out in the GraphPad Prism 6 program applying an ANOVA between the results obtained with the standardized technique and after making the modifications. Resulting a non-significant variation with a value of P = 0.5382.
Discussion
The present study is an analysis of the work carried out in the Department of Cell Biology Microbiology of the UAZ, in the line of research of Trichinella spiralis, from 1986-2021.Which has allowed to carry out research work, teaching, training of undergraduate and postgraduate human resources, 80 theses, which have contributed results to the study of Trichinella spiralis., In implementation of experimental models, characterization of the life cycle of T. spiralis, establishment of direct and indirect techniques, evaluation of treatment with drugs and immunogens, epidemiological studies for the detection of the parasite and the proposal of a low-cost and accessible diagnostic kit for the field. Our results coincide with other authors, the investigations have been published. For us it is very important to continue with this line of research, because unfortunately the infection in many cases is not diagnostic, hence our interest in having effective treatments, diagnostic techniques that are preventive against this zoonosis that is increasingly distributed worldwide. climate change favors their presence, the loss of ecosystems, and all this contributes to diminishing and impacting the quality of life not only of humans but also of animals and ecosystems.
Conclusions
The Autonomous University of Zacatecas has a research line in
Trichinella spiralis, which has allowed to carry substantive functions,
including teaching, research, extension, dissemination, and having
an impact on the training of human resources. The findings
reported in this research include: a reproducible experimental model for
the study of Trichinellosis, reliable diagnostic techniques
and confirmatory WB, an effective treatment using albendazole
(which must be used under medical prescription), and the study of
products such as the bacterial vaccine, the VITS immodulator, the
Lactobacillus casei strain, which decrease the parasite load as well
as the immunogen of the total soluble antigen of Trichinella spiralis.
The contribution of this study has been to provide deeper insights
in a disease which is present in the state of Zacatecas, Mexico and is
commonly not properly diagnosed or confused with other diseases,
we consider very important to continue promoting having a proper
diagnosis and prevention of the disease.
For more Articles on : https://biomedres01.blogspot.com/




No comments:
Post a Comment
Note: Only a member of this blog may post a comment.