Comparison of Three Treatment Methods of Ⅰ-Ⅲ Degree Hemorrhoids: A Meta Analysis
Introduction
Hemorrhoids is a common clinical disease and its pathogenesis is not yet clear. The theory of anal cushion displacement is widely accepted at present, that is, supporting tissue degeneration, including fibrous tissue fragmentation, elastic connective tissue and submucosal muscle fiber weakening, which may be related to lack of dietary fiber, constipation, improper defecation habits and lifestyle. The main clinical manifestations of hemorrhoids are bleeding during defecation, pain, anal prolapse, swelling, pruritus and perianal secretions [1]. Depending on the location of the disease, hemorrhoids can be divided into internal hemorrhoids, external hemorrhoids and mixed (internal and external) hemorrhoids. Internal hemorrhoids are formed by tissue covered by columnar epithelium, and located above the dentate line; External hemorrhoids are formed by tissue covered by squamous epithelium, and located below the dentate [2]. Mixed hemorrhoids appear at the top and bottom of the dentate line. The staging of internal hemorrhoids is not completely unified in the world. Goligher’s classification is more commonly used, which divides internal hemorrhoids into gradeⅠ-Ⅳ.
i. Grade Ⅰ: Bleeding during defecation, but not prolapse, most
patients have no obvious symptoms.
ii. Grade Ⅱ: The hemorrhoids protrude out of the anus during
defecation, and the prolapse can be returned by itself.
iii. Grade III: Prolapse out of the anus during defecation,
fatigue, long walking, or coughing. After prolapse, internal
hemorrhoids cannot be repaid by themselves, and they need
to be repaid by hand.
iv. Grade Ⅳ: With external hemorrhoids, the hemorrhoids
remain outside the anus for a long time and cannot be repaid
or prolapse immediately after being repaid.
The treatment methods of internal hemorrhoids include
non-surgical treatment and surgical treatment. Most internal
hemorrhoids of grade I-III can be alleviated by non-surgical
treatment such as drug treatment, RBL, IS, and IRC; grade IV internal
hemorrhoids, internal hemorrhoids that fail or have complications
should undergo surgical treatment [3]. RBL is a simple, quick and
effective method for treating patients with grade I-II and part of
grade III internal hemorrhoids. The method is to ligate with ligator
above the dentate line, and the internal hemorrhoids are necrotic
due to blood flow blockade and fall off automatically [4]. IS is an
endoscopic or anal endoscopic injection of sclerosis agent into
the submucosal layer of internal hemorrhoids, forming fibrosis
and scars. IRC is to coagulate the hemorrhoid blood vessels or
cause fibrosis of the hemorrhoid submucosa through the instant
high heat generated by infrared rays, to fix the anal cushion. IRC
is mainly used for the treatment of internal hemorrhoids of grade
I - III [2]. The purpose of this study was to compare the efficacy and
safety of RBL, IS and IRC in the treatment of internal hemorrhoids.
We evaluated the evidence from the random control trial (RCT)
and the research data from the systematic review of the RCT, and
performed a meta-analysis, which is reported below.
Materials and Methods
Search strategy
Use keywords such as “Hemorrhoids”, “Hemorrhoid sclerotherapy”, “Injection sclerotherapy”, “Rubber band ligation”, “Hemorrhoid ligation”, “Infrared coagulation”, “Hemorrhoid infrared coagulation”. Searched the literatures from PubMed, Cochrane Library, and Embase database up to 2021. The research method limited the RCT to improve the sensitivity and did not limit the language, and the related references in the included literature were manually searched, and consistent standards were used to determine the included and excluded literature.
Inclusion and Exclusion Criteria
• Participants of the study included patients ≥18 years of age
who met the Goligher’s grading classification criteria and
patients with grade I-Ⅲ internal hemorrhoids; patients
diagnosed with grade IV hemorrhoids and patients with other
anorectal diseases other than the study disease were excluded.
• The original text is publicly published literature; it is limited to
RCT, in which patients are randomly assigned to two or more
treatment groups, clinical results are recorded, and follow-up
time is at least 3 months.
• The original literature provides corresponding indicators of
effectiveness and safety: including effective rate, recurrence
rate, complication rate, etc.
• The type of literature is limited to treatises, and literatures with
incomplete original data are excluded. reviews, conference
reports, reviews, case reports, etc. are excluded.
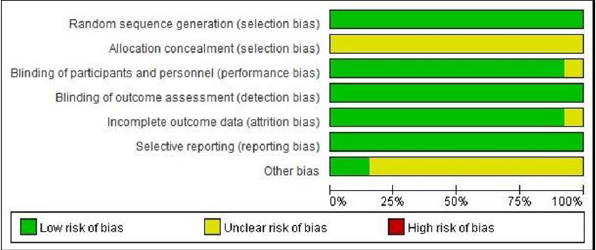
• The included RCTs are all evaluated by the Cochrane handbook
to evaluate the quality of the literature.
Data Extraction
General data of the literature were extracted: including the first author, year of publication, number of patients included, observation data, etc. The extraction of all data was done independently by two researchers. For the controversial data, the third researcher participated in the discussion and decided.
Outcome Indicators
Main Outcomes: Effective Rate, Recurrence Rate.
Secondary Outcome: Complications.
Statistical Analysis
Meta-analysis was conducted with Review Manager 5.4 software to study the effective rate, recurrence rate and complication rate of RBL, IS and IRC in the treatment of patients with internal hemorrhoids. As a dichotomous variable analysis, odds ratio (OR) was used as the effect index, and 95% confidence intervals (95%CI) is calculated. The Cochrane Q test was used to evaluate the heterogeneity among studies, and the magnitude of heterogeneity among studies was determined by combining the I2 value. Moderate to high heterogeneity was considered when I2 was greater than 50%, and the test level was α=0.1. The data were combined and analyzed for heterogeneity. If there was no heterogeneity (I2≤50% and P≥0.1), the fixed-effect model was selected for analysis; If there was heterogeneity (I2>50% and/or P<0.1), then analyze its sources and discuss, choose random effects model analysis. Meta analysis test level was α=0.05. For highly heterogeneous variables, the single study deletion method was used to conduct sensitivity analysis to find the source of heterogeneity. If the heterogeneity decreased after deleting the document, the document was the source of heterogeneity, and the forest figure was finally made. Regarding the analysis of publication bias, by observing whether the two sides of the funnel chart were symmetrical, if the two sides were symmetrical, there was no obvious publication bias, and if the two sides were asymmetric, there may be publication bias.
Meta Analysis Results
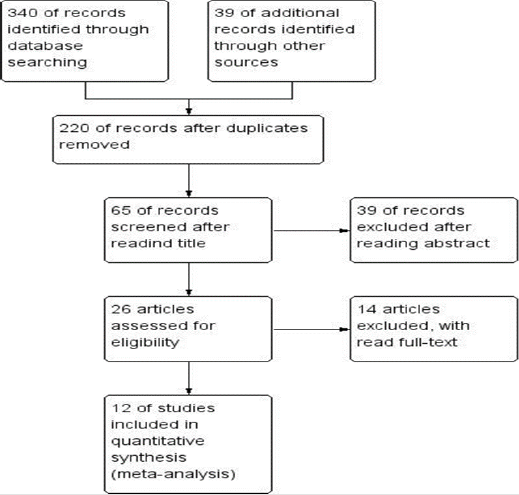
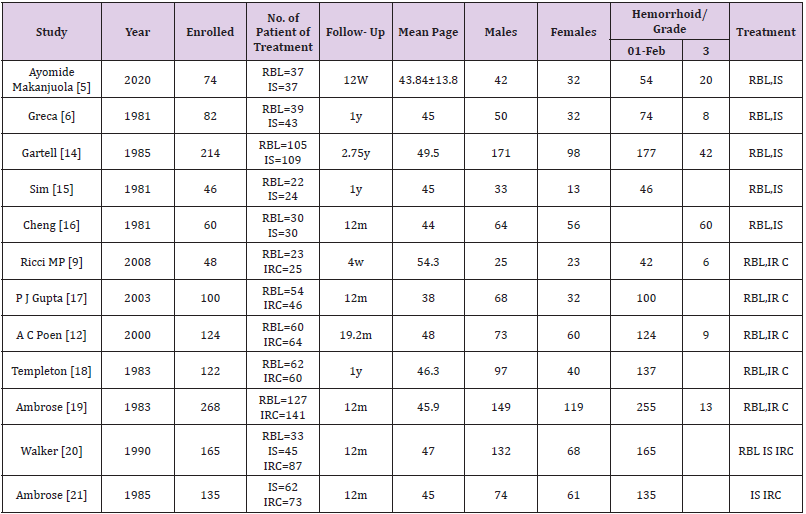
A total of 379 relevant literatures were retrieved, 159 duplicate literatures were excluded, 155 were excluded after reading the title, 39 were excluded after reading the abstract, and 14 were excluded after reading the full text. A total of 12 literatures were screened according to the inclusion criteria (Figure 1). A total of 1438 patients were included, including 592 patients in the RBL group, 350 patients in the IS group, and 496 patients in the IRC group. The detailed data of the included literatures were shown in Table 1 (Figure 2).
Effective Rate
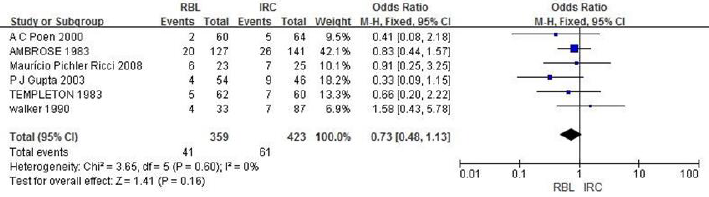
a. RBL vs IRC: A total of 782 cases are included in 6 literatures, and heterogeneity analysis indicates no heterogeneity (P=0.60, I2=0%). The fixed-effect model analysis is carried out, and the results shows that there is no significant difference in the effective rate between the RBL group and the IRC group (OR=1.36, 95%CI:0.89-2.09, P=0.16), indicating that the treatment effect of the two groups is similar, as shown in Figure 3.
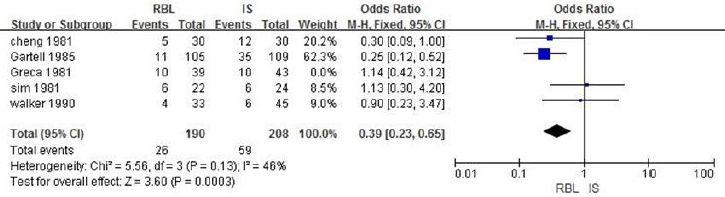
b. RBL vs IS8: A total of 480 patients are included in 5 literatures. Fixed effect model analysis is used, and the heterogeneity analysis indicates that there is heterogeneity (P=0.06, I2=55%). By eliminating literatures one by one, it is found that the heterogeneity decreases after eliminating literatures Greca.1981, with statistical difference (OR = 2.56, 95% CI: 1.53-4.27, I2 = 46%, P = 0.0003). It suggests that the effective rate of RBL group is better than that of IS group, as shown in Figure 4.
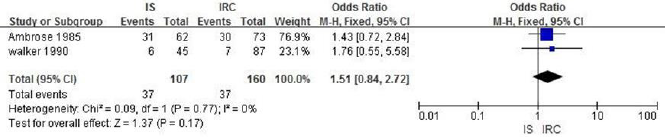
c. IS vs IRC: A total of 267 patients are included in 2 literatures. Heterogeneity analysis shows that there is no heterogeneity (P = 0.77, I2 = 0%). Fixed effect model analysis is carried out. The results shows that there is no significant difference in the effective rate between IS group and IRC group (OR = 0.66, 95% CI: 0.37-1.19, P = 0.17), indicating that the treatment effect of the two groups is similar, as shown in Figure 5.
The Recurrence Rate
a. RBL vs IRC: A total of 612 patients are included in 4 literatures. Fixed effect model analysis is used and the heterogeneity analysis indicates that there is heterogeneity (P=0.004, I2=77%). By eliminating literatures one by one, it is found that the heterogeneity decreases after eliminating literatures Walker.1990, with statistical difference.(OR=0.40, 95%CI:0.24-0.67, I2=44%, P=0.0003), suggesting that the recurrence rate of the RBL group is lower than that of the IRC group, as shown in Figure 6.
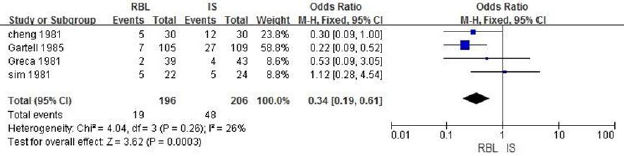
b. RBL vs IS: A total of 480 patients are included in 5 literatures. Fixed effect model analysis is used and the heterogeneity analysis indicates that there is heterogeneity (P=0.02, I2=67%). By eliminating literatures one by one, it is found that the heterogeneity decreases after eliminating literatures Walker.1990, with statistical difference (OR=0.34, 95%CI:0.19-0.61, I2=264%, P=0.0003), suggesting that the recurrence rate of the RBL group is lower than that of the IS group, as shown in Figure 7.
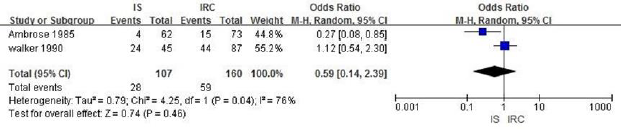
c. IS vs IRC: A total of 267 patients are included in 2 literatures, and the heterogeneity analysis indicates that there is heterogeneity (P=0.04, I2=76%). Since there are only 2 literatures, random effect model analysis is carried out, and the results showed that there is no significant statistical difference in the recurrence rate between IS group and IRC group(OR=0.59,95%CI:0.14- 2.39,P=0.46), suggesting that the recurrence rate of IS group and IRC group is similar, as shown in Figure 8.
Incidence of Complications
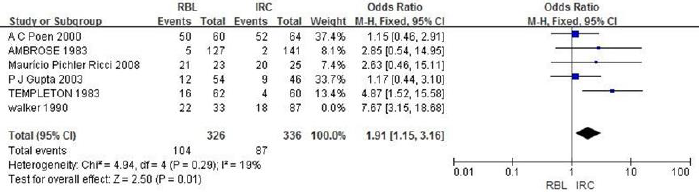
a. RBL vs IRC: A total of 782 patients are included in 6 literatures. Fixed-effects model is used and the heterogeneity analysis indicates that there is heterogeneity (P=0.03, I2=59%). By eliminating literatures one by one, it is found that the heterogeneity decreases after eliminating literatures Walker.1990, with statistical difference (OR=1.91, 95%CI: 1.15~3.16, I2=19%, P=0.01), suggesting that the incidence of complications in the RBL group is lower than that in the IRC group, as shown in Figure 9.
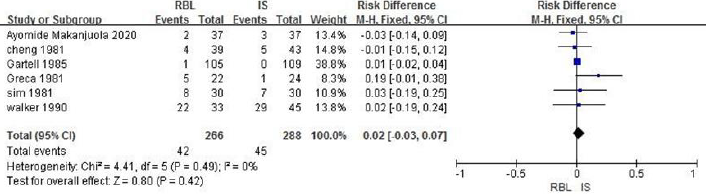
b. RBL vs IS: A total of 554 patients are included in 6 articles and heterogeneity analysis indicates no heterogeneity (P=0.49, I2=0%). The fixed-effect model analysis is carried, and the results shows that there is no significant difference in the incidence of complications between the RBL group and the IS group (OR =0.02, 95%CI: -0.03~0.07, P=0.42), as shown in Figure 10.
Discussion
Hemorrhoid is a soft venous mass produced by the dilation
and flexion of the submucosal and cutaneous inferior venous
plexus at the end of the rectum, which contains normal spongy
tissue structures such as minute arteriovenous anastomosis,
connective tissue, and nerve tissue, thus playing an important role
in assisting and controlling defecation. Hemorrhoids are the most
common anorectal diseases in adults, accounting for 89.25% of all
anorectal diseases, and treatment needs are huge. The main clinical
manifestations of internal hemorrhoids include bleeding, prolapse,
pain and perianal itching, and in several cases, it can be complicated
with thrombosis, incarceration, strangulation and difficulty in
defecation, which significantly affects the patient’s quality of life.
The treatment of internal hemorrhoids focuses on the elimination
of symptoms caused by internal hemorrhoids. The commonly used
treatment methods for internal hemorrhoids include non-surgical
treatment and surgical treatment, among which non-surgical
treatment includes RBL, IS, and IRC. The national guidelines of
the United States, Japan, France, and China countries recommend
that the above methods are mainly used for the treatment of I-III
degree internal hemorrhoids [1,5,6], but the efficacy and safety of
various methods are still controversial. In this article, the efficacy,
recurrence rate and complication rate of the above three methods
for the treatment of internal hemorrhoids are analyzed and
compared in order to comprehensively and objectively evaluate the
efficacy and safety of RBL, IS and IRC in the treatment of internal
hemorrhoids. The results of this study show that the efficiency
of RBL group is better than that of IS group, which is consistent
with the research results of Jacobs, D et al. it is mentioned in the
research report that the long-term effective rate of RBL group is
about 90% among patients with internal hemorrhoids of grade
I-III, while the long-term remission rate of only one-third of the
patients treated with IS, indicating that the long-term effective rate
of RBL is superior to that of the IS group [7]. Similarly, the research
results of MacRae HM et al. also show that for I-III degree internal
hemorrhoids, it is recommended to use RBL as the first-line
treatment, and its curative effect is better than IS. Compared with
patients receiving IS or IRC treatment, the need for retreatment in
RBL group is obviously reduced [8]. This study has shown that the
efficacy of the RBL group was comparable to that of the IRC group.
The research by Ricci MP et al. also reported that the success rate
of 4 weeks after RBL was not different from that of IRC, that is, the
short-term clinical efficacy of RBL was comparable to that of IRC
[9].
This study shows that the efficiency of IS group is equivalent to
that of IRC group, which is similar to the research results of MacRae,
MD et al. . It is mentioned in the research report that there is no
difference in any outcome index between IS group and IRC group
[10]. IS is the most effective for I-II degree internal hemorrhoids,
and postoperative bleeding is rare. For patients with high risk of
bleeding, such as patients receiving anticoagulant therapy, this
method should be considered [7]. This study suggests that the
incidence of complications in RBL group is lower than that in IRC
group. However, the research of Johanson JF et al. Showed that
RBL has better long-term efficiency, but the incidence of pain after
treatment is higher. In contrast, the complications of IRC are few
and not serious [11]. The reason for the analysis may be that the
current guidelines classify pain as a type of complication. This
article does not analyze pain alone, but classifies it as a complication
for analysis. This study shows that the recurrence rate of RBL group
is lower than that of IS group and IRC group. A C Poen et al. reported
that 18% of the patients receiving RBL treatment had symptomatic
recurrence, while 20% of the patients receiving IRC treatment had
symptomatic recurrence to the level before treatment [12], and the
longer the follow-up time was, the higher the symptom recurrence
rate was [13]. Meta-analysis of non-surgical treatment showed
that the recurrence rate of Ⅰ-II internal hemorrhoids patients after
IS was relatively high, while the discomfort caused by RBL was
relatively high [14-24].
The Limitations of this Study
1) Although the research documents included in the systematic
review are all RCTs, the follow-up time varies, and there is a
lack of multi-center, large-scale, long-term follow-up RCT
research results.
2) Some studies have a small sample size, and some evaluation
indicators only have 2-3 literatures for effect combination, and
the outcome indicators of the analysis are not fully mentioned,
such as: surgical recovery time, cost-benefit ratio, patient
satisfaction, etc. To systematically evaluate the three methods,
there is still a lack of high-quality RCTs research.
3) The cases of internal hemorrhoids in some literatures are not
classified.
In conclusion, for the treatment of grade I - III internal
hemorrhoids, the safety of RBL group is better than IS group and
IRC group, and the efficacy is better than IS group or equivalent to
IRC group. Therefore, RBL can be the first choice among the three
treatment methods, but it still needs to be verified by multi-center,
large-sample and high-quality RCTs.




No comments:
Post a Comment
Note: Only a member of this blog may post a comment.