Successful Treatment of Extranodal Natural Killer T Cell Lymphoma Nasal Type Complicated by Severe Hemophagocytic Syndrome A Case Report
Introduction
Extranodal Natural Killer/T-Cell Lymphoma, Nasal Type(ENKL),
is a rare malignancy of Non-Hodgkin lymphoma characterized by
an aggressive clinical course and poor prognosis [1]. It is mostly
endemic to East Asia and is associated with Epstein–Barr Virus
(EBV) infection [2]. Its lesions are predominantly present in
the Upper Aerodigestive Tract (UADT) such as the nasal cavity,
nasopharynx, paranasal sinuses or palate. Less commonly, ENKL
can manifest at extra nasal locations like the lung, skin, soft tissue,
gastrointestinal tract, and testis. Since the neoplasm can destroy
the midline facial structures, the disease used to be known as lethal
midline granuloma [3,4].The presentation of the disease at extra
nasal locations is nonspecific and may mimic many other benign or
malignant lesions. Patients with extra nasal presentation often have
more adverse clinical features such as an advanced stage, elevated
LDH and poor performance status, and the survival rate is inferior
compared with the nasal sites [5-7]. Hemophagocytic Syndrome
(HPS), also known as Hemophagocytic Lymphohistiocytosis (HLH),
is highly heterogeneous and comprises primary and secondary
types.
Secondary HPS is associated with a variety of underlying
conditions such as infection, malignancy, and autoimmune
diseases. ENKL is frequently complicated with HPS, and survival
is discouraging in this circumstance [8]. However, no standard
treatment has been established based on the results of randomized
controlled trials because of the rarity of the disease [9]. Here,
we report a case of ENKL complicated by severe Lymphoma-
Associated Hemophagocytic Syndrome (LAHS). The patient
was treated according to the R-DEP (ruxolitinib, liposomal
doxorubicin,VP-16,dexamethasone) chemotherapeutic regimen,
and the hemophagocytic lymphohistocytosis gradually improved
during chemotherapy. Then P-Gemox (pegaspargase, gemcitabine,
oxaliplatin) chemotherapy in combination with the use of anti-
PD1 antibody (Sintilimab Injection ) were performed and achieved
PR(partial remission). For personal reasons, the patient chose
a different hospital to continue the treatment. He achieved CR
(Complete Remission) with the therapy of anti-PD1 antibody and
Chidamide. Unit now the patient has received the therapy for
almost one year and follow up regularly in outpatient department.
Case Report
A 32-year-old non-smoking man was emergently transferred to our hospital on June 30, 2019, because of a month-long highgrade fever, cough, left-sided chest pain and blood in phlegm. Prior to this, the patient had a history of trauma to the right lower limb and the wound healed itself. About ten days later he presented to a local hospital with the above-mentioned chief complaint and a chest computed tomography scan showed multiple nodules, ground-glass opacities and patchy infiltration scattered in both lung fields. Then he had been treated as for pneumonia. However, his clinical condition did not improve. The patient was therefore admitted to our hospital for further evaluation and treatment. There was no relevant personal or family medical history for this patient. The physical examination upon admission revealed a palpable mass(3cm)on the left dorsal side and the lower margin of the right 9th rib, respectively. Fine rales were heard in the lower left lung. Hematologic examination showed a white blood cell count of 2.67×109/L, a hemoglobin concentration of 11.6 g/ dL, and a platelet count of 77×109/L. Serum chemistry showed abnormal results as follows: aspartate aminotransferase (AST)115 IU/L, alanine aminotransferase (ALT)133 IU/L, fibrinogen 1.13g/L, lactate dehydrogenase 966IU/L (normally 114–240 IU/L),Creactive protein 25.53 mg/L (normally less than 10mg/L),the procalcitonin level 0.17ng/ml(normally<0.05ng/ml),triglyceride 2.96mmol/L (normally 0.33-1.7 mmmol/L), serum ferritin8141.3 ㎍/L (normally 20–200 ㎍/L), soluble interleukin (IL)- 2 receptor>7500U/mL (normally 223–710U/mL) and natural killer (NK) cell activity 1.75%.In addition, his plasma EBV DNA level was 4300copies/ml. A bone marrow aspiration did not show lymphoma involvement (Figure 1).
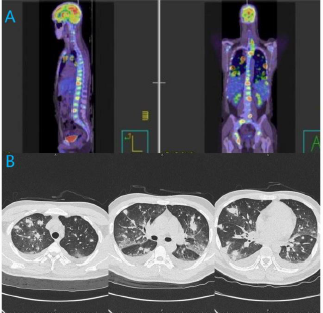
Figure 1:
a) PET/CT revealing heterogeneous hypermetabolic masses in both lung fields, as well as hepatic, splenic, osseous, soft tissue,
and multiple lymph node metastases that involved the mediastinum, porta hepatis, bilateral hilum of lung.
b) Chest CT scan showing multiple nodules, ground-glass opacities and patchy infiltration in both lungs.
The patient was HIV negative. Two sets of blood cultures, and tumor markers, including CEA,SCC, CFRA21-1,Pro-GRP, and NSE were all normal. The G test and GM test were both negative. Antinuclear antibody, anti-ENA antibodies, and anti-neutrophil cytoplasmic antibodies were all negative. Administration of broadspectrum antibiotics did not resolve hissymptoms. Bronchoscopic examination did not give a definite diagnosis. Lung nodules increased and grew larger, and hypoxia progressed. A CT-guided transthoracic needle biopsy of the left lower lung was performed (Figure 2). During the course of treatment, FDG PET/CT was conducted and revealed heterogeneous hypermetabolic masses in both lung fields, as well as hepatic, splenic, osseous, soft tissue on the left dorsal side and the lower margin of the right 9th rib, and multiple lymph node metastases that involved the mediastinum, porta hepatis, bilateral hilum of lung. Then we also performed a ultrasound-guided percutaneous puncture biopsy of soft tissue at the lower margin of the right 9th rib. Immunohistochemical staining of these two specimens both yielded positive results for CD56, CD3, CD2,and the Ki-67 proliferation index was 80%;in situ hybridization for EBV-encoded early small RNAs (EBER) was also positive; however, results were negative for CD79a,CD20.
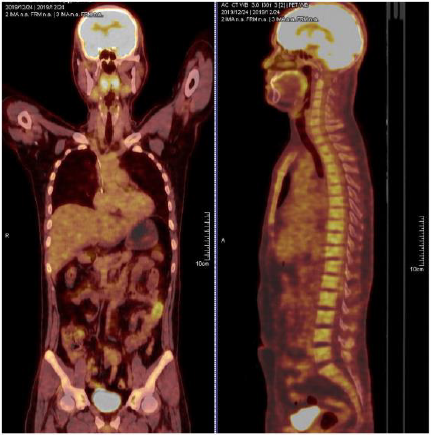
Moreover, Hemophagocytic lymphohistiocytosis was confirmed by cytopenia, fever, splenomegaly, hyperserotonemia, hypertriglyceridemia, low natural killer (NK) cell activity and increased circulating soluble IL-2 receptor. A diagnosis of ENKL complicated by LAHS was made. The markedly elevated circulating plasma EBV-DNA level supported the diagnosis. R-DEP(ruxolitinib, liposomal doxorubicin,VP-16,dexamethasone) chemotherapeutic regimen was performed to control the LAHS and it gradually improved during chemotherapy. Then six cycles of P-GEMOX(pegaspargase, gemcitabine, oxaliplatin) chemotherapy in combination with the use of anti-PD1 antibody(Sintilimab Injection) were performed and achieved PR(partial remission) after the treatment. Although the patient suffered from septic shock caused by Klebsiella pneumoniae in the neutropenic period, he was cured by broad-spectrum antibiotics when neutrophil improved. For personal reasons, the patient chose a different hospital to continue the treatment. He achieved CR(complete remission) confirmed by using positron emission tomography-computed tomography (PETCT) with the therapy of anti-PD1 antibody(Tislelizumab Injection) and Chidamide. Until now the patient has received the therapy for more than one year and follow up regularly in outpatient department (Figure 3).
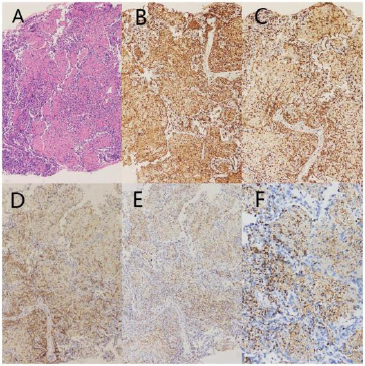
Figure 3: Pathologic findings in CT-guided transthoracic needle biopsy specimens.
a) Histologically, a small number of nuclear hyperchromatic cells presented with large areas of observable
necrosis(HEstaining;magnification,×400).
b) Immunohistochemical staining positive for the expression of CD2(magnification,×400).
c) Immunohistochemical staining positive for CD3 expression (magnification,×400).
d) Immunohistochemical staining positive for the expression of CD56 (magnification,×400).
e) Immunohistochemical staining positive for the expression of TIA-1(magnification,×400).
f) In situ hybridization positive for EBV-encoded RNA (magnification,×400).
Discussion
To our knowledge, there have been only a few reports
documenting long-term remission in patients with ENKL
complicated by severe LAHS. Han et al conducted a study comparing
NK/T-LAHS with LAHS associated with other T cell lymphomas,
which indicated that both had poor prognosis with a median survival
time of 28 and 33 days, respectively [10]. Chang, et al. [11] identified
that a long diagnosis time was a poor prognostic factor for patients
with LAHS. So the early identification of lymphoma-associated HPS
is essential to improve patient, prognosis. However it is challenging
since misdiagnosis often occurs as fever and pancytopenia may
also be caused by severe infection. The CT findings of pulmonary
non-Hodgkin’s lymphoma are varied and nonspecific. Patchy
consolidations, nodules, and masses are the most frequent CT
findings and infiltrations can also be seen [12]. It is reported that
PET-CT may act as a significant tool to assess patients with LAHS,
as it is highly sensitive in detecting neoplasms of the majority of
histologic subtypes of lymphoma, and also demonstrates extensive
18‑fluorodeoxyglucose (FDG) uptake in tumor tissues [13]. Anyhow
there is no non-invasive test specific enough to make a correct
diagnosis of ENKL. So lymphoma complicated with HPS should be
considered in patients presenting with fever, cough, dyspnea and
pancytopenia, associated with unilateral or bilateral pulmonary
consolidation and pleural effusion, when combination therapy
involving numerous antimicrobial agents has failed. A proper
diagnosis may be established by a histopathological examination.
The International Peripheral T-cell Lymphoma Project
demonstrated that extranasal NK/T-cell lymphoma (nasal type)
has worse clinical features and survival rate, even in cases with
apparently localised disease, than nasal NK/T-cell lymphoma in
extranodal NK/T cell lymphoma [14].In this report, the tumor
involved multiple organs throughout the patient’s body. As with
the progressive disease courses and poor prognosis, effective
therapeutic strategies are urgently needed. As for HPS, the
patient was treated according to the R-DEP(ruxolitinib, liposomal
doxorubicin,VP-16,dexamethasone) chemotherapeutic regimen,
and the overall condition of the patient gradually improved during
chemotherapy. Nevertheless, it was equally important to treat
primary diseases as well as treating HPS [11]. Regarding ENKL, no
standard treatment has been established based on the results of
randomized controlled trials because of the rarity of the disease [9].
ENKL cells are associated with a high expression of P-glycoprotein,
leading to multidrug resistance that is likely responsible for the poor
response to conventional anthracycline-based chemotherapy [15].
P-GEMOX is a modification of the Gemcitabine, L-Asparaginase, and
Oxaliplatin (GELOX) regimen in which L-asparaginase is switched
to pegaspargase and was also included as a suggested treatment
regimen for ENKL in the NCCN guidelines [16]. In a retrospective
analysis of 117 patients with ENKL (96 with newly diagnosed ENKL
and 21 with relapsed/refractory(R/R) disease), the P-GEMOX
regimen resulted in an ORR of 88% and responses were similar for
patients with newly diagnosed and R/R ENKL [17].
Recently, newer agents for ENKL, including immune checkpoint
inhibitors and histone deacetylase inhibitor, have been shown
to exhibit promising efficacy. Tislelizumab is an anti-human
programmed death receptor-1 (PD-1) monoclonal IgG4 antibody
that is being developed by Bei Gene as an immunotherapeutic,
anti-neoplastic drug. Tislelizumab has been investigated in
haematological cancers and advanced solid tumours, leading to
its approval in December 2019 in China for patients with relapsed
or refractory classical Hodgkin’s lymphoma after at least secondline
chemotherapy [18].The registration of tislelizumab for other
indications is currently underway. Chidamide (CS055, HBI-8000),a
novel oral benzamide class of subtype-selective inhibitor of HDAC
1,2,3 and10,inhibited cell proliferation and interfered withPI3KAkt-
mTOR and MAPK signaling. A prospective phase II trial in China
illustrated that chidamide monotherapy was effective in 15 patients
(detailed disease stages not reported) with relapsed/refractory
extranodal NK/T-cell lymphoma [19]. In our case the patient has
already received the therapy of anti-PD1 antibody with Chidamide
for more than one year, showing that this treatment is effective
and safe. As randomized trials comparing different regimens have
not yet been conducted and standard therapy has not yet been
established for these patients, treatment should be individualized
based on patient, tolerance and comorbidities.
Conclusion
At this moment, there is no recommended treatment for ENKL complicated with HPS because of the extreme rarity of this entity. It was equally important to treat primary diseases as well as treating HPS. L-asparaginase-containing regimens are the cornerstone for treating ENKL. In this modern ENKL treatment era, newer agents are being investigated for treating ENKL and prospective multicenter trials need to be performed to establish an optimal treatment for this rare and dismal disease.
For more
Articles on : https://biomedres01.blogspot.com/

No comments:
Post a Comment
Note: Only a member of this blog may post a comment.