Does Intestinal Parasite Infection Causes Anemia Among Pregnant Women in Ethiopia A Systematic Review and Meta-Analysis
Research Article
Introduction
Pregnant women with Hemoglobin level less than 11 g/dl are considered to be anemic [1]. In the world, 56 million pregnant women are anemic [2] In Africa the magnitude of anemia among pregnant women was 57.1% [3]. Prevalence of anemia among pregnant women in Ethiopia is 63% and in east Africa countries 55% in Kenya, 58% in Sudan and Eritrea 55.3% [4]. Different factors might leads to anemia among pregnant women. Geohelminth infections during pregnancy were associated with maternal anemia. Hookworm infection causes anemia among pregnant women and it also aggravates anemia in pregnant women [5]. Infections by helminthes leads to malnutrition, iron deficiency anemia, and increased vulnerability to other infections in infected pregnant women [6]. Other recent studies in Ethiopia have reported prevalence of anemia ranging from 16.6% in a facilitybased study in Gondar, northwest Ethiopia to 56.8% in Gode town, Eastern Ethiopia [6 ,7]. Prior studies in Ethiopia have reported significant associations between anemia in pregnancy and parasitic infections [e.g. schistosomiasis, hookworm infection], prior use of contraceptives, use of iron supplementation, birth spacing/ intervals, parity and gravidity, educational attainment, age, body weight, trimester of pregnancy and wealth status [6 -18]. Despite there are many researches done on anemia among pregnant women in Ethiopia, but data on intestinal parasitic infection and anemia among pregnant women in Ethiopia is not adequate. This systematic review and meta-analysis was conducted to assess the relationship between intestinal parasitic infection and anemia among pregnant women in Ethiopia.
Methods
Search Approach and Appraisal of Studies
Studies were Searched using primary key terms of ‘determinant of anemia ‘, ‘anemia ‘, ‘intestinal parasitic infection ‘, ‘ intestinal parasitic infection and anemia ‘, ‘Ethiopia ‘ and to generate additional keywords for the search we were used the following search strategies; ‘ intestinal parasitic infection + anemia +pregnant women + Ethiopia through Electronic databases on reference manager software.
a) The databases searched were PUBMED and Advanced Google Scholar
b) References of studies that meet eligibility criteria were used to identify similar articles
Inclusion Criteria
a) All Studies that were assessed the relationship between intestinal parasitic infection and anemia.
b) The outcome of interest was anemia
c) The study reported the percentage of anemia according to intestinal parasitic infection
d) Meet quality assessment
Exclusion Criteria
a) Studies that were published in languages other than English,
b) Included participants with anemia not dichotomized as anemia and no anemia,
c) Included participants with intestinal parasitic infection not dichotomized as yes and no
d) Studies conducted not in Ethiopia were also excluded to avoid the combination of studies that were not comparable.
Data Extraction
Three researchers were carried out the data extraction The extracted information were the name of the author, study area, the number and percentage of anemia, the number and percentage of intestinal parasitic infection.
Risk of Bias and Quality Assessment
To assess external and internal validity, a risk-of-bias tool was used. The tool has seven items:
1. Random sequence generation [selection bias],
2. Allocation concealment [selection bias],
3. Blinding of participants [performance bias],
4. Blinding of outcome assessment [detection bias],
5. Incomplete outcome data [attrition bias],
6. Selective reporting [reporting bias] and
7. Other bias. All of these items are rated based on the author’s subjective judgment given responses to the preceding seven items rated as low, moderate or high risk.
Three reviewers assessed independently the articles for inclusion in the review using risk-of-bias tool and guided by PRISMA checklist. A discrepancy that would face by reviewers on selection of studies and data extraction was resolved by discussion Additionally, all potential confounding variables were controlled by multivariable analysis in all included studies.
Measures
Outcome variable pregnant women with Hemoglobin level less than 11 g/dl are considered to be anemic [1].
Statistical Analysis
The necessary information was extracted from each original study by using a format prepared in Microsoft Excel spreadsheet and transferred to Meta-essential and Revman software for further analysis. Pooled effect size of anemia was estimated from the reported proportion of eligible studies using RevMan V.5.3 software. Forest plots were generated displaying MH odd ratio with the corresponding 95% CIs for each study. As the test statistic showed significant heterogeneity among studies Heterogeneity: Tau² = 0.13; Chi² = 13.11, df = 5 [P = 0.02 ]; I² = 62% ] the Random effects model was used to estimate the DerSimonian and Laird’s pooled effect.
Assessment of Publication Bias
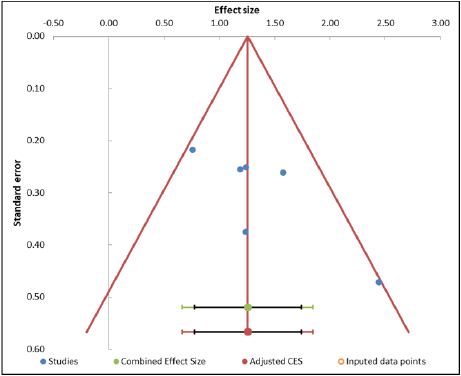
Funnel plot asymmetry and Egger’s test was used to check the publication bias.
Results
Selected Studies
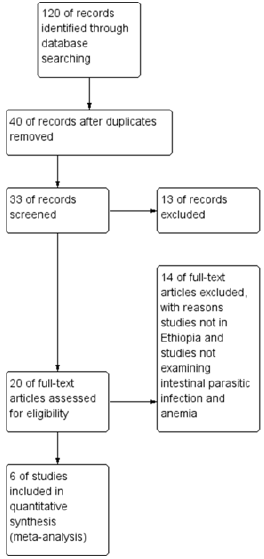
Figure 1 shows selection process of studies 120 of records identified through database searching 40 of records after duplicates removed 33 of records screened and 13 of records excluded, 20 of full-text articles assessed for eligibility and 14 of full-text articles excluded, with reasons, studies not in Ethiopia and studies not examining intestinal parasitic infection and anemia and finally 6 of studies included in quantitative synthesis [meta-analysis].
Characteristics of Included Studies
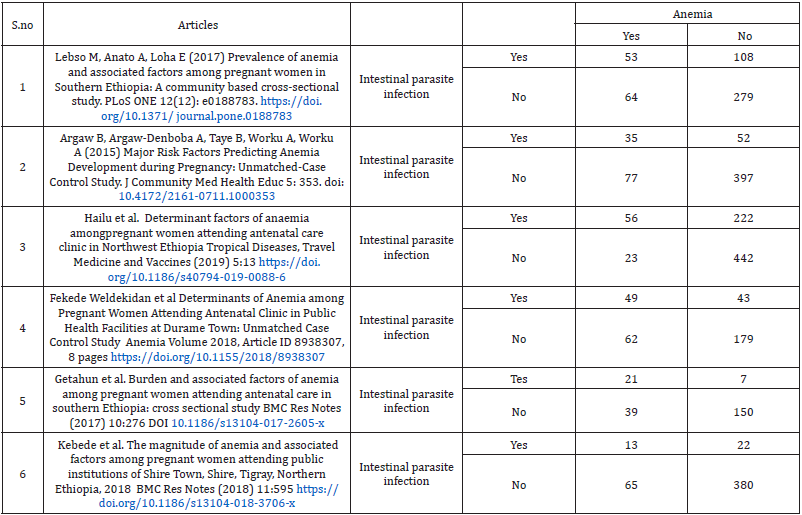
Six observational studies involving 2838 participants, 557 pregnant women who have anemia were included. In all studies, the proportion of anemia among pregnant women who have intestinal parasitic infection during current pregnancy was 227 [33.33%].
Pooled Effect Size
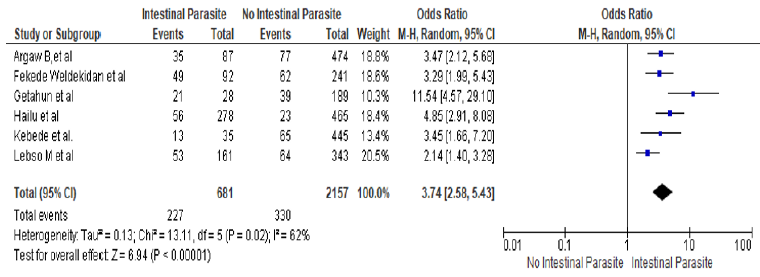
The odds of anemia among pregnant women who had intestinal parasitic infection is 3.74 times higher than those pregnant women who did not have intestinal parasitic infection [ORMH = 3.74, 95% CI 2.58-5.43] Heterogeneity: Tau² = 0.13; Chi² = 13.11, df = 5 [P = 0.02]; I² = 62% Test for overall effect: Z = 6.94 [P < 0.00001] (Figure 2).
Figure 2: Forest plot for the association between intestinal parasite infection and anemia among pregnant women in Ethiopia
Assessment of Publication Bias Analysis
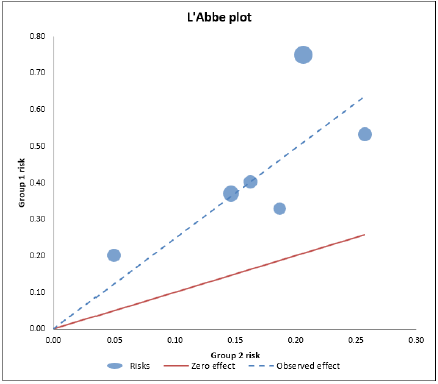
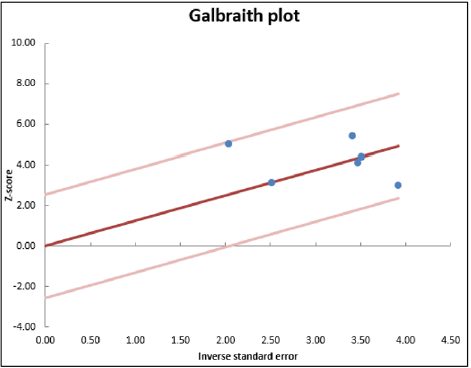
No publication bias was observed [Egger’s test: p = 0.074, Begg’s test: p = 0.091]. The below ‘Abbe plot showed that all studies effect size is above the zero-effect size. The below Galbraith plot showed that 95% of the studies effect size lie between the two-color lines and this indicates there is no outlier of effect size. (Tables 2 &3) (Figures 3-5).
Figure 3: Funnel plot for the association between intestinal parasite infection and anemia among pregnant women in Ethiopia.
Figure 4: ‘Abbe plot for the association between intestinal parasite infection and anemia among pregnant women in Ethiopia.
Figure 5: Galbraith plot for the association between intestinal parasite infection and anemia among pregnant women in Ethiopia.
Discussion
In this systematic review and meta-analysis, pregnant women who were infected with intestinal parasite were 3.74 times more likely to be anemic than who were not infected by any intestinal parasite and this is consistent with previous studies, [6, 19-24]. The worm in the intestine may cause intestinal necrosis and blood loss as a result of the attachment to the intestinal mucosa and chronic infections lead to iron deficiency and anemia resulting from the excessive loss of iron [25]. Therefore, an effective intervention packages need to reduce anemia among pregnant women through iron supplementation, anthelmintic treatment and dietary diversification in the study area [26]. Our finding is similar with other previous study in Ethiopia [27] this possibly happen because most anemic pregnant women who are living in Ethiopia were farmers, bare foot walking is common among Ethiopian farmers, and the chance to be exposed for soil transmitted parasite is very high. Besides this, the low environmental sanitation status may also aggravate the chance of intestinal parasite infection. Parasitic diseases were known to play as a major contributing factor to anemia in pregnancy. For example, blood loss caused by hookworm puts mothers at high risk of iron deficiency anemia [28]. Our finding is similar with many previous studies conducted in Ethiopia and other developing countries that have shown the strong association of intestinal parasitic infection with anemia in pregnant women [23,28-29,30-33] Parasitic infection has a devastating effect on the level of Hgb and causes anemia since they affect iron absorption by the intestine and consumes the red blood cells [34]. There was a strong significant association between intestinal parasitic infection and anemia in pregnant women.in previous studies [35], in Southern Ethiopia [19], Ghana [34], Nigeria [36], and Venezuela [37], Durame Town Ethiopia [38]. , in Yirgalem and Hawassa cities, Dessie town and Canada [27, 39. 33 ]., Shire Town , Tigray, Northern Ethiopia [40], in Shalla Woreda of Oromia region In Ethiopia [16]. This is expected as intestinal parasites, apart from their competition for nutrients, are known to cause blood loss, loss of appetite reduced motility of food through the intestine and damage to the wall of the intestine leading to mal-absorption of nutrients.
Conclusion
The likelihood of anemia among pregnant women is approximately four times higher among pregnant women who had intestinal parasitic infection than who did not have the infection.
| For more Articles on : https://biomedres01.blogspot.com/ |




No comments:
Post a Comment
Note: Only a member of this blog may post a comment.