Number of Foci Increases Risk of Central Compartment Lymph Node Metastasis in Papillary Thyroid Cancer
Research Article
Introduction
The incidence of papillary thyroid carcinoma (PTC) has increased in a dramatic pattern in recent years [1,2]. PTC often presents with multifocal tumors, i.e., presence of two or more non-contiguous tumor foci either unilaterally or bilaterally, which is one of the most prominent characteristics of PTC. It is well established that multifocality represents a higher propensity for a more advanced staging, and multifocality per se is a qualitative parameter to assess the risk for LNM. However, it is not easy to quantify its effects on pathological outcome and clinical features. The prevalence of the multifocal PTC ranged from 32% to 39% in large series of PTC [3-5]. In clinics, multifocality is often empirically treated as a high-risk factor for aggressiveness of PTC and reported to be associated with extensive LNM [4], higher recurrence rate [5], and more aggressive biological behavior [6,7], compared with unifocal PTC. However, inconsistent and even contradictory findings also exist [4,8,9]. It is well accepted that active surveillance should be recommended to patient with microcarcinoma at low risk. However, a clinical dilemma is how do physicians handle with multifocal microcarcinoma which all the foci are less than 1cm in diameter. In other words, whether multifocality could be used as a quantified parameter rather than a qualitative parameter need to be addressed. Moreover, although prophylactic central compartment neck dissection is not routinely recommended according to ATA guidelines, insidious LNM do exist and be the cause for the recurrence of PTC. Thus, is it safe to recommend not receiving central compartment neck dissection for all patients with multifocal papillary thyroid microcarcinoma?
In this study, we retrospectively analyzed 1034 patients with papillary thyroid carcinoma to evaluate the how the multifocality affects the central compartment LNM and try to quantify the multifocality to further predict the possible insidious central compartment LNM.
Material and Methods
Patients
Patients diagnosed with papillary thyroid cancer (classic type) between April 2013 to September 2013 in Tianjin Medical University Cancer Institute and Hospital were recruited. Medical records, ultrasonographic and histopathological reports were reviewed. Patients with histological variant (follicular, tall cell, trabecular or others) or patients whose tumor is in the isthmus were not included. Sex, age, tumor size, bilateral disease, tumor foci number, and cervical LNM were determined in each patient. Ethics approval was obtained from The Institutional Review Board of Tianjin Medical University Cancer Institute and Hospital (approval: BC2021023), and the requirements for patient approval and informed consent were waived because of the retrospective nature of the study.
Data Collection/ Definition of Parameter
Bilateral disease was defined as the presence of PTC foci in the right and left lobes of the thyroid gland. The size of the largest focus of PTC was used for analysis. Multifocal disease was defined as the presence of two or more foci of PTC.
Determination of Number of Tumor Foci and Tumor Size
To define the number tumor foci and tumor diameter of each tumor, ultrasonographic and histopathological reports were reviewed by two independent researchers. The number of tumor foci is determined according to the histopathological reports. As for each tumor’s largest diameter, we refer to the ultrasonographic reports for each tumor and record its ultrasonographic diameter. The largest diameter is recorded if three-dimensional data is given by the ultrasonographers.
Statistical Analysis
Statistical analysis was performed using IBM SPSS Statistics for Windows v21 (IBM Corp., Armonk, NY). Univariate analysis was performed using Chi-squared test or Fisher’s exact tests for categorical variables, Student’s t-tests for normally distributed data, and Mann–Whitney U-tests for continuous variables that were not normally distributed. Cox regression analyses was used for univariate and multivariate analysis. All p-values represented were two-sided and considered statistically significant when p<0.05.
Results
Clinical and Pathological Features
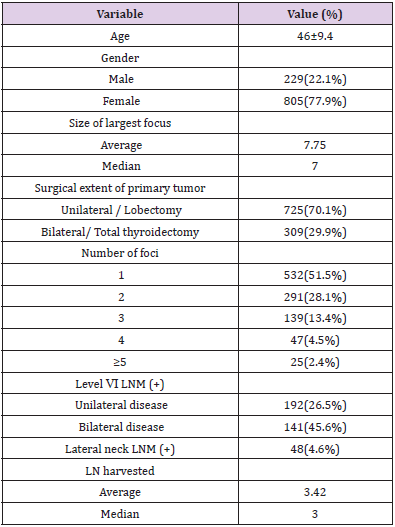
A total of 1034 patients were diagnosed as PTC or PTMC in our department during April 2013 to September 2013. The mean age was 46 years (range, 18-76), of which 229 (22.1%) were male and 805 were female (77.9%). The median tumor size was 7mm (range, 1-45). Multifocal cancer lesions were found in 502 patients (48.5%), in which the number of patients with 2 to 4 foci were 291(28.1%), 139(13.4%), and 47(4.5%), respectively, with 25(2.4%) patients with ≥5 foci. Of all the multifocal PTMCs, 273 (57.2%) were bilateral and 177 (42.8%) were unilateral. The level Ⅵ LNM rate for unilateral and bilateral cancer patients were 26.5% and 45.6%, respectively. The clinical and pathological features of these patients were summarized in Table 1.
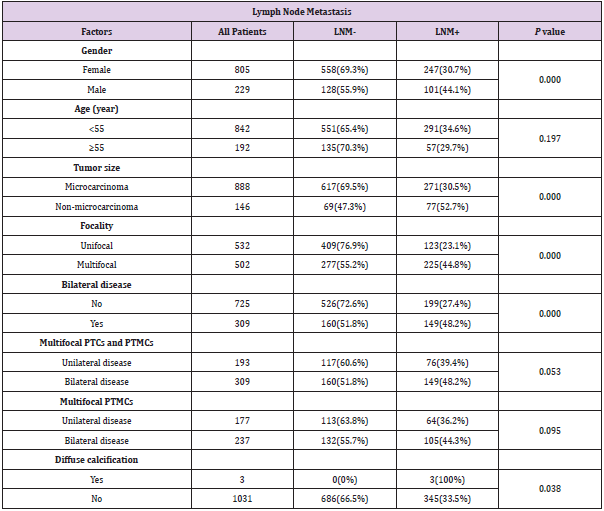
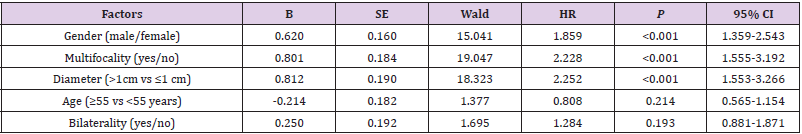
Factors Associated with Central Compartment LNM
Univariate analysis was done to assess the risk factors of central compartment LNM. As for all the patients included, male gender, tumor size larger than 1cm, multifocality, bilateral disease, diffuse calcification were risk factors for central compartment LNM Table 2. Interestingly, when multifocal diseases were considered (including both multifocal PTCs and multifocal PTMCs), bilateral disease was no longer a risk factor (P=0.053, P=0.095, respectively). We then calculated the independent risk factor for LNM by multivariate analysis, we found that male gender, multifocality, diameter larger than 1cm, diffuse calcification on ultrasonography are all independent risk factors for LNM. However, age and bilaterality are not independent risk factors for LNM Table 3.
Central compartment LNM rate is associated with multifocality irrespective of unilateral or bilateral disease.
In PTCs that larger than 1cm in diameter, the LNM rate of unifocal PTC is 36.2% (21/58), whereas the LNM rate of multifocal PTC is much higher at 63.6% (56/88, P=0.001). We then analyzed the effect of bilaterality on central compartment LNM. Of note, the LNM rate of unilateral multifocal PTC is 75% (12/16), which is comparable to the LNM of bilateral multifocal PTC 61.1% (44/72, P=0.296). Similar results were observed in PTMC patients. The LNM rate of unifocal PTMC is 21.5% (102/474), whereas the LNM of multifocal PTMC is 40.8% (169/414), in which LNM of unilateral multifocal PTMC is 36.2% (64/177), which is comparable to the LNM rate of bilateral multifocal PTMC 44.3% (105/237, P=0.095), as summarized in Table 2.
Table 2: Factors predictive of lymph node metastasis in the univariable analysis.
Abbreviations: PTMC, papillary thyroid microcarcinoma; PTC, papillary thyroid carcinoma; LNM, lymph node metastasis.
Number of Foci Increases the LNM Rate
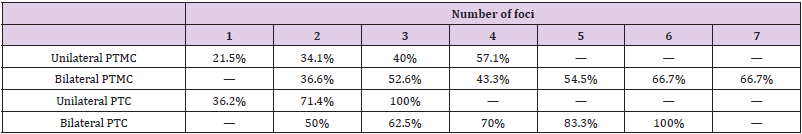
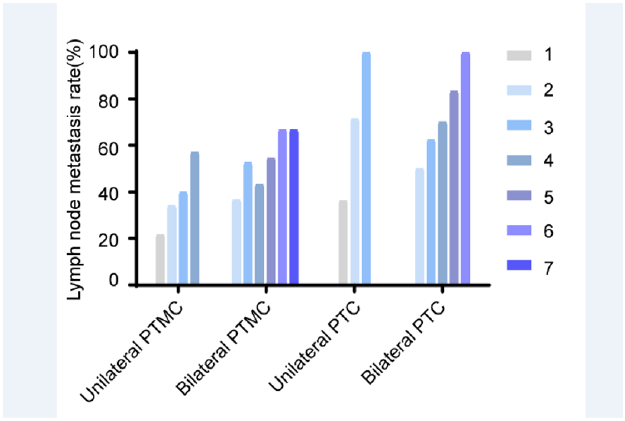
The above results showed that multifocality is a risk factor for increased LNM rate irrespective of unilateral or bilateral disease. This finding suggests that multifocality might be interpreted in the setting of one “thyroid lobe”, rather than “one thyroid gland”. Thus, the effect of the number of PTC foci on central compartment LNM was further examined. As shown in Table 4, for all the unilateral PTMC, 102 of 474 (21.5%) patients with unifocal PTMC had level VI lymph node metastases. Whereas 46/135 (34.1%) patients with two foci of PTMC were found to have positive lymph nodes. The proportion of patients with positive level VI nodes increased in the group with three foci, where 14/35 (40%) patients were found to be positive. In patients with 4 foci, 4/7 (57.1%) were found to have positive lymph nodes in level VI. Interestingly, a gradual increase in LNM proportion is observed, with respect to foci number, as displayed in Figure 1. In bilateral PTMC patients, 41 of 112 (36.6%) patients with two foci bilateral PTMC had level VI lymph node metastases. Whereas patients with 3 to 7 foci of bilateral PTMC were found to have positive LNM were 41/78 (52.6%), 13/30 (43.3%), 6/11 (54.5%), 2/3(66.7%), 2/3(66.7%), respectively.
Table 4: Lymph node metastasis rate at various number of foci.
Abbreviations: PTMC, papillary thyroid microcarcinoma; PTC, papillary thyroid carcinoma
Figure 1: Central lymph node metastasis rate is increased with respect to increased foci number. For all unilateral or bilateral PTMCs and PTCs, the LNM rate is increased in accord with the increased foci number.
A similar result was also observed in PTC patients with largest diameter larger than 10mm. As for unilateral PTC patients with largest diameter larger than 10mm, the LNM proportion is 21/58 (36.2%), 10/14 (71.4%) and 2/2 (100%) for unilateral PTC patients with 1 to 3 foci. For bilateral PTC patients with largest diameter larger than 10mm, the LNM proportion is 15/30 (50%), 15/24 (62.5%), 7/10 (70%), 5/6 (83.3%), 2/2 (100%) for bilateral PTC patients with 2 to 6 foci Table 4.
LNM Rate for Multifocal PTMC Is Comparable to Unifocal PTC When Ptmcs Largest Diameter is Between 6-10 mm
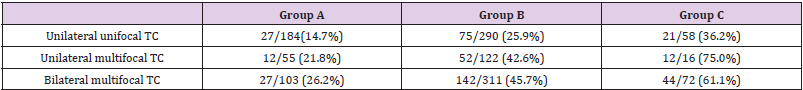
To further assess the effect of multifocality on LNM, patients were stratified according to the largest diameter. Patients were divided into three groups: A. largest diameter is ≤5mm; B. 6mm≤largest diameter≤10mm; C. largest diameter >10mm. As shown in Table 5, in group A, the LNM proportion in unilateral unifocal PTMC, unilateral multifocal PTMC and bilateral multifocal is 27/184 (14.7%), 12/55 (21.8%) and 27/103 (26.2%). In group B, the LNM proportion in unilateral unifocal PTMC, unilateral multifocal PTMC and bilateral multifocal is 75/290 (25.9%), 52/122 (42.6%) and 142/311 (45.7%). In group C, the LNM proportion in unilateral unifocal PTC, unilateral multifocal PTC and bilateral multifocal PTC is 21/58 (36.2%), 12/16 (75.0%) and 44/72 (61.1%). For unilateral PTMCs and PTCs, the LNM proportion in patients from group A, B and C were 12/55 (21.8%), 52/122 (42.6%) and 12/16 (75%). For both unilateral and bilateral PTMCs and PTCs, the LNM proportion in patients from group A, B and C were 27/103 (26.2%), 142/311 (45.7%) and 56/88 (63.6%). Interestingly, when we compare the risk of LNM for multifocal PTMCs, we found that the LNM rate for multifocal PTMCs in group B (6mm≤largest diameter≤10mm) is comparable to unilateral unifocal PTCs whose largest diameter is greater than 1cm (52/122, 42.6%, vs. 21/58, 36.2%; P=0.413), indicating that multifocal PTMCs might have the same propensity to LNM with unifocal PTC which largest diameter is greater than 1cm.
Table 5: Lymph node metastasis rate according to largest tumor diameter.
Group A: PTMC’s largest diameter is ≤5mm; Group B: 6mm≤largest diameter≤10mm; Group C: largest diameter >10mm.
Abbreviations: TC: thyroid cancer
Discussion
Previously, multifocality has been implicated as a qualitative parameter to assess the risk for central compartment LNM. However, few studies have shown how the number of foci affect the LNM. In this study, the risk factors for lymph node metastasis were studied, then the effect of multifocality was further investigated between the number of PTC foci and LNM to central compartment. Multifocality is a common clinical characteristic of PTC and has been reported in 18–87% of patients with PTC [10] and was seen in 48.5% of patients in the present study. Our results show that the risk of level VI lymph metastasis increases proportionally with the number of tumor foci, both in PTMCs and PTCs which diameter is larger than 1cm. When the number of foci reaches 3 or more, the level VI LNM rate exceeds 50% or higher (52.6% and 62.5% for bilateral PTMC and bilateral PTC). And even 100% in the presence of 6 foci. Ayham et al reported a similar result in the presence of 3 or more foci, except that no appreciable difference in level VI lymph node metastasis in patients with one and two foci [11]. These findings identify multifocality in PTC as an indicator of tumor aggressiveness, manifesting in a higher propensity for locoregional metastasis.
Both univariate and multivariate analysis identified male gender, tumor size larger than 1cm, multifocality, diffuse calcification as significant predictors of level VI lymph node metastasis in the study population. These findings are consistent with previously published studies identifying risk factors for level VI metastasis in PTC [12-14]. Of note, our data indicated a rare phenomenon diffuse calcification as significant predictors of level VI lymph node metastasis. Diffuse calcification has been implicated with thyroid malignancy [15,16]. In our study, the LNM rate for the PTC with diffuse calcification is 3/3 (100%), although the case number is small, it still strongly indicates that PTC patients with diffuse calcification under ultrasonography has a higher propensity for locoregional metastasis. Another interesting finding is that, when we compare the LNM rate between multiple PTMCs (6mm≤largest diameter≤10mm) and unifocal PTC which diameter is larger than 1cm, there is no significant difference between these two groups. This finding indicates that multifocal PTMCs with 6mm≤largest diameter≤10mm has the same propensity for LNM in central compartment, compared with unifocal PTC with largest diameter ≥10mm. Other studies have shown concordant result that multifocal PTMC with relative bigger foci is at higher risk of LNM although it might not be clinically evident. Zhao et al. has proposed the concept of aggregate diameter (AD) to better assess the tumor burden [17,18]. Abbas et al. also pointed out that the sum up of the diameter of each tumor foci >10 mm confers a similar risk of aggressive histopathological behavior with unifocal PTC greater than 10 mm [19].
In conclusion, this study provides evidence that multifocal PTCs are at higher risk of LNM, which tendency might increase in the presence of over 4 foci when compared with unifocal and bifocal disease. In addition, multifocal PTMCs with largest foci between 6mm to 10mm might have the same tendency to PTC which diameter is >10 mm. Thus, multifocal thyroid PTMCs should not be managed as conventional PTMCs at low risk, thereby prompting more aggressive treatments.
| For more Articles on : https://biomedres01.blogspot.com/ |



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.