Comorbidity Resolution and Quality of Life after Bariatric Surgery
Introduction
Recently, obesity has become one of the most important health
problems in our society. In 2008 and according to the World Health
Organization (WHO) 1.4 billion people in the world suffer from
overweight and 500 million from obesity [1]. The prevalence of
obesity in Spain is 21.6%, being higher in men and older people [2].
The high prevalence of metabolic syndrome among obese patients
suggests that both entities share the lipotoxicity as etiological
mechanism. In overweight patients, cardiovascular pathologies
are more frequent as well as invalidating knee and waist arthritis.
Obesity also accounts for 44% of diabetes type 2 (DM2) and nonalcoholic
steatohepatitis (NASH) affects practically every obese
patient. This excess weight is the main risk factor for obstructive
sleep apnea (OSA). Obesity is a preventable cause of diverse
cancer types: colon, rectum, breast, uterus, kidney, esophagus and
pancreas [3]. It also impacts the personal sphere with a reduced
functionality in the everyday life activities and a worse quality of
life
(QoL). Clinical studies show that this QoL is not only a consequence
of their worse physical condition, but it is also due to their lack of
self-esteem, personal and social acceptation [4]. Stress, anxiety
and depression are very frequent symptoms. The prevalence of the
latter ranges from 23 to 69% much higher than the in the general
population (17%). It has also been suggested that the incidence of
psychopathologies and severe psychiatric affections is higher, being
this partly responsible for the lack of adherence to the dietetic
treatment and lifestyle changes. Weight loss has been related to a
significative decrease in psychological symptoms [5].
Bariatric surgery (BS) was developed in the 50s as a promising treatment for those patients in whom the classic approach with diet modifications, exercise and drugs was not effective, allowing a maintained weight loss in the long term. It is performed worldwide with restrictive, malabsorptive or mix techniques, being the gastric by-pass (GBP), a mix technique, the gold standard. Other procedures are the sleeve (GS) and biliopancreatic derivation [6]. Surgery has shown a reduction in the associated comorbidities as well as a reduction in global mortality [7]. DM2 remission rate is over 50% in different studies [8-10]. Therefore, BS is recommended in those diabetic patients with a BMI ≥ 35 kg/m2 and poor glycemic control in spite of dietetic and adequate medical treatment. Most recent guidelines recommend that metabolic surgery could be considered in DM2 patients with a BMI ≥ 30 kg/m2 [11]. After surgery HBP prevalence is halved and dyslipidemia is reduced or disappears in 70% of cases, especially in BPG and biliopancreatic derivation. As far as OSA is concerned, its remission is around 35- 40% [12]. Other comorbidities such as the arthropathy haven’t been so thoroughly studied.
Given that BS is not exempt from risks, is crucial to carefully select the patients undergoing this surgery. It is indicated in the following criteria cases [1,6]: Age between 18 and 65; BMI ≥ 40 kg/ m2 without comorbidities or BMI ≥ 35 kg/m2 with comorbidities (Drug resistant DM2 or HBP, OSA, infertility, severe arthropathy). To evaluate the three fundamental aspects after surgery (i.e. weight loss, comorbidity resolution and QoL) The Bariatric Analysis and Reporting Outcome System (BAROS) was developed. This score system is considered a helpful tool to evaluate both objective and subjective outcomes. To address the subjective part it includes the Moorehead-Ardelt II QoL questionnaire, specifically validated in BS [13]. BAROS score was conceived by Oria in 1990 [14] and has been used in most countries since then. In 2009, Oria introduced minor changes which resulted in the questionnaire used nowadays [15]. The objective of our study is to evaluate the results in patients undergoing BS in the HURS, using BAROS scoring method to evaluate the outcomes after surgery.
Material and Methods
We performed a descriptive, observational, cross-sectional study which evaluated patients undergoing BS in the HURS. All patients attending a follow-up between January and December 2018 were included. Verbal informed consent was requested and those who accepted were handled the BAROS scoring method [16]. This questionnaire evaluates the clinical improvement in two parts: The first one evaluated by the investigator and the other one answered by the patient. The part evaluating the postoperative evolution is divided into two sections: weight loss evaluated as the percent excess weight loss (%EWL) and the resolution of comorbidities.
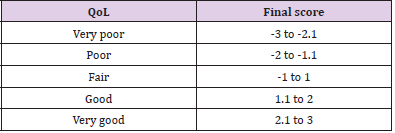
Each one of these sections receives a score from -1 to +3, according to the %EWL and the evolution of the comorbidities. In case the patient didn’t suffer from any comorbidity this part is obviated. It is also taken into account the appearance of complications and the need of a reoperation. The second part takes into account the QoL, assessed by the Moorehead-Ardelt II questionnaire which evaluates self-esteem, physical activity, social life, work conditions and sexual activity. The score in each of these items is added up in order to obtain a final result which ranges from -3 to +3 (Table 1).
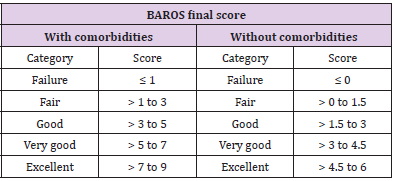
The addition of the two parts, after subtracting points corresponding to complications or reoperations, gives a final score which values the global result of the surgery. The highest score depends on the existence of presurgical comorbidities (Table 2). On the other hand, the researcher collects the age, gender, type of surgery and time since the BS (in months). The comorbidities we studied were DM2, HBP, dyslipidemia, OSA, arthropathy and cardiovascular illnesses. Information to assess the evolution of comorbidities is obtained from the interview with the patient, their medical records and the list of their active medications in the computer system. To define DM2 remission we followed ADA (American Diabetes Association) criteria [17].
Statistical Study
In the descriptive study, continuous variables are expressed with the mean and standard deviation (SD) and categorical variables as frequencies and percentages. To compare the independent means between two groups whose quantitative variables follow a normal distribution, we used the Student’s t-test. To compare independent means among more than two groups in quantitative variables which follow a normal distribution, we used the ANOVA test. Levene’s test was performed to assess the equality of variances and Scheffé’s test to the post-hoc comparison. To evaluate the statistical correlation between two quantitative variables, Pearson correlation coefficient was employed. Chi’s squared was used to compare the qualitative variables between independent groups. Normality distribution of variables was assessed with the Saphiro-Wilk test. The relationship between QoL and the different independent variables was analysed with a logistic regression. Statistical significance was considered with a p-value < 0.05.
Results
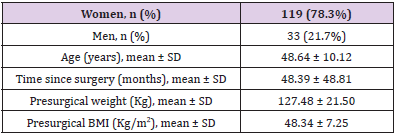
152 patients were recruited (Table 3). 78.3% (n= 119) women and 21.7% (n=33) men. Mean age was 48.64 ± 10.12 years. The mean time after surgery was 48.39 months. Mean BMI just before surgery was 48.34 ± 7.25 kg/m2. Prior to surgery 31.6% of patients suffered from DM2 (n=48); 40.8% from HBP (n=62); 35.5% from dyslipidemia (n= 54); 19.7% from OSA (n=30); 11,8% from arthropathy (n= 18) and 4.6% patients (n=7) had suffered a cardiovascular event. The types of surgical techniques performed were gastric bypass in 65.1% of patients (n=99), gastric sleeve in 31.6% (n=48) and gastric banding in 3.3% (n=5). 17.8% patients (n=27) presented with minor complications and 9.2% (n=14) with mayor ones. 17.8% (n=27) had to be reoperated.
Surgical Outcomes
Weight Loss: BMI after surgery was 32.75 ± 6.16 kg/m2, being this reduction statistically significant. %EWL was 60.46 ± 18.8%. The difference in weight loss was not statistically significant among the surgical techniques performed.
QoL: QoL after surgery was reported as fair in 20.4% of patients (n=31), good in 23% (n=35) and very good in 54.6% (n=83). 2% (n=3) had poor or very poor QoL. There were no statistically significant differences between QoL and type of surgery performed. When exploring the relationship between QoL and %EWL it is remarkable that patients with very good QoL had a statistically significant higher %EWL (64.29%) than patients with fair (57.39%) and good QoL (54.14%).
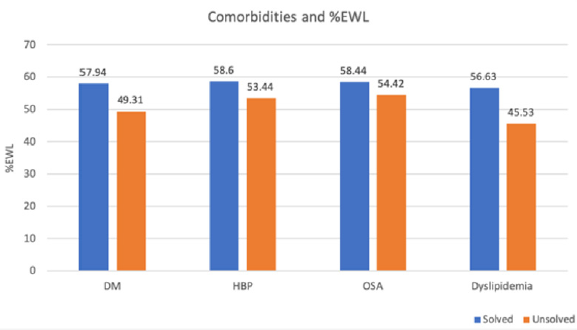
Resolution of Comorbidities: 60.5% of the patients in our study suffered from comorbidities prior to the BS. These were aggravated in 3.3% of them (n=5), in 10.5% (n=16) didn’t change and improved in 7.2% (n=11). They were solved in 39.4% patients: In 16.4% (n=25) one comorbidity was resolved and in 23% (n=35) all of them disappeared. 39.5% (n=60) didn’t have previous comorbidities. DM2 remitted in 75% of patients (n=36); HTA in 38.7% (n=24), dyslipidemia in 51.9% (n=28), OSA in 33.3% (n=3) and vasculopathy in 57.1% (n=4) of cases (Figure 1). Arthropathy wasn’t resolved in any patient. There are no statistically significant differences according to the surgical technique. %EWL was higher in those patients whose comorbidities disappeared. However, these differences were not statistically significant, except from the dyslipidemia (Figure 2). Patients without DM2, HBP or dyslipidemia before surgery achieve a higher %EWL than patients with these comorbidities, being this difference statistically significant (p<0.001). The relationship between resolution of the two most important comorbidities (DM2, HBP) and QoL didn’t achieve statistical significance.
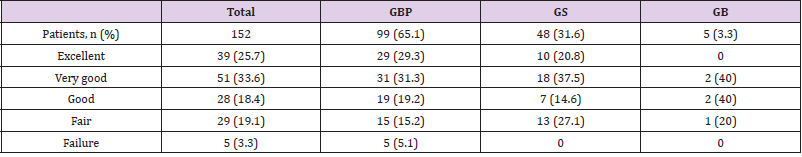
Global Evaluation: BAROS Questionnaire: 3.3% of patients (n=5) are classified as failure; 19.1% (n=29) as fair; 18.4% (n=28) as good evolution; 33.6% (n=51%) as very good and 25.7% (n=39) as excellent. BAROS questionnaire results according to the surgical technique are shown in Table 4. There were no statistically significant difference when comparing QoL results with the surgical technique, although the percentage of patients with excellent results is higher in those who underwent a BPG. Patients with a fair result according to the BAROS questionnaire had a statistically significant longer follow-up than those classified as very good or excellent result. The variables associated with the QoL were included in a multivariate logistic regression analysis but these results were not statistically significant.
Discussion
Nowadays, BS is considered the only effective treatment for obesity in the long term. With conventional treatment, patients may lose around 5 to 10% of their initial weight; with BS, though, patients may achieve losses around 25 to 30%, which can be maintained up to 20 years, according to research by O’Brien [18]. In our study, we identified a mean weight loss, expressed as %EWL, of 60.46% and a post-surgical BMI of 32.65 kg/m2, which stayed stable since the surgery. According to success criteria in BS by SEEDO-SECO, these results can be considered as good [19]. We found similar results in numerous studies. O’Brien’s metanalysis described a %EWL of 71% in biliopancreatic derivation, 60% in GBP and 49% in gastric sleeve. In our research, results didn’t differ among the different types of surgery. Comorbidities resolution has been excellent given that in 23% of patients all of their comorbidities disappeared and in 16.4% one of them was solved, with an improvement in the rest. These results agree with prior ones. Queiroz follows up 120 patients who underwent GBP for two years, checking that out of 71 patients with one or more comorbidities, there is a complete remission in 86% of cases and a partial remission in 14% [20]. In accordance with most previously published research up to the moment, DM is the comorbidity that benefits the most of BS with a 75% resolution rate in our series. Ribeiro’s group quantified DM and dyslipidemia resolution in a 100% of the patients and HBP resolution in 77% of the cases [21]. Surgery has been proven safe with 9.2% of major complications and a 17.8% rate of reoperation. These results coincide with Queiroz work [20]. BS advantages go further beyond than just a simple weight loss, though, and that is the reason why we used BAROS questionnaire which focuses on the QoL of patients, a very often neglected aspect in published research. In our work we checked that most patients considered their postsurgical QoL as good or very good, similarly as what is found in literature. In Ribeiro’s work, QoL patients referred was better (8%) or much better (92.5%) after GBP [21]. Alcaraz-García evaluates the impact of BS in QoL of obese patients after surgery. It finds a decrease in BMI, improvement or disappearance of comorbidities and improvement in QoL variables, which translates into a raise in self-esteem, physical activity, social life, work conditions and sexual activity [22]. We analysed the three more frequent techniques and found no statistically significant differences in QoL among them. BAROS results confirm previous results are far as efficacy and safety of BS are concerned. The longer the follow-up period is, the worse BAROS final score is, given that those patients with a fair score have a statistically significant longer follow-up time than those with very good and excellent score. One limitation in our study is lacking presurgical QoL data, which makes it impossible to quantify the improvement. At the same time, had the sample been larger, we might have found statistically significant differences among surgical techniques.
Conclusion
1. Results of bariatric surgery according to the BAROS
system were good, very good or excellent in 81.73% of patients,
after a mean follow-up of 4 years and without statistically
significant differences among techniques.
2. %EWL was 60.46%, with an average post-surgical BMI of
32.65 kg/m2 which is considered as a good result.
3. In 46.6% of the patients, bariatric surgery has improved
and/or resolved all pre-surgical comorbidities being diabetes
the pathology that benefits the most.
4. In our experience, QoL of patients after bariatric surgery
is good or very good in 77.6% of cases, without statistically
significant differences between QoL and type of surgery
performed.
5. QoL is influenced by loss weight so that patients with a
very good QoL showed statistically significant higher WLP than
patients with fair and good QoL.
For more Articles on : https://biomedres01.blogspot.com/




No comments:
Post a Comment
Note: Only a member of this blog may post a comment.