Recovery of a Vietnamese Child from Impaired Fasting Glucose and Hyperinsulinemia After one Year of Implementation of an Appropriate Diet Plan: A Case Report
Introduction
Global increase in T2D in children and aldolesents has raised
a serious concern on the health condition of the future generation.
Combination of multiple risk factors such as genetics, the mother’s
gestational diabetes, poor diet and lifestyle are considered as the
cause of this rise (Castorani, et al. [1]). While there are no possible
actions can be done to change the genetics of the person, adopting
an appropriate personalized diet and lifestyle represents the
sole option for the prevention of the disease pathogenesis and
management. High fat low carb diet has demonstrated health
benefits in restoring metabolic syndroms and other diseases
(Walton, et al. [2]) (Dowis, et al. [3]). Recent data shows a significant
increase in T2D mellitus as well as in prevalence of non-diagnosed
T2D in children worldwide (Spurr, et al. [4]). In Vietnam, it was
reported in a recently published study that the prevalence of T2D
in children from 11-14 years old is lower than in most countries
and the impaired fasting glucose prevalence is up to 6.5% (Phan,
et al. [5]). T2D mellitus in children is often diagnosed only when
grave complications have already occurred because of the poor
risk management and the lack of surveillance programs and tools.
Consequently, pediatric patients risk being put on medicaments
including insulin injection at a very young age. We report here a
case of a 9-year-old Vietnamese male diagnosed with IFG and
hyperinsulinemia in December 2019 following cortisol treatment
(from August 2018) for severe hair loss (Alopecia areata). One year
after changing his diet, the patient has restored his IFG, insulin,
complete blood count and re-started to grow taller after more than
one year staying at the same height.
Case Report
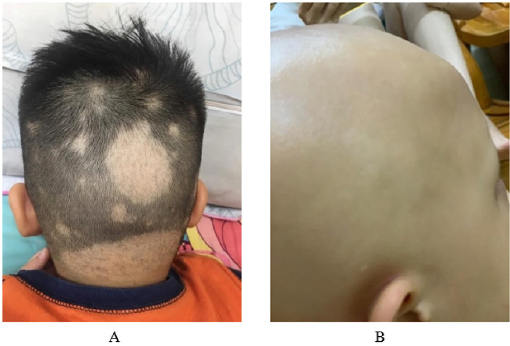
A 9-year-old male presented at the hospital in August 2018 with alopecia areata symptoms. He was put on a treatment of 4mg of Methylprednisolone and 0.1% Mometasone furoate, daily. His severe hair loss was advancing rapidly to complete hair loss within one year (Figures 1A & 1B). The patient was with a normal BMI of 23.3 kg/m2 and none of the blood tests for diagnosis of T2D was performed upon his first visit to the hospital. On another visit to the hospital on December 2019, he gained 5kg and was diagnosed with T2D with fasting glucose of 6.6 mmol/L, HbA1C of 5.1%, a very high fasting insulin of 123.048 μU/mL and C-peptide of 4.7 nmol/L. He was then put on metformin while continuing the cortisol treatment.
Figure 1: Hair loss progression of the patient
A) Photo taken at the beginning of the hair loss in August 2018.
B) photo taken in May 2020.
Results
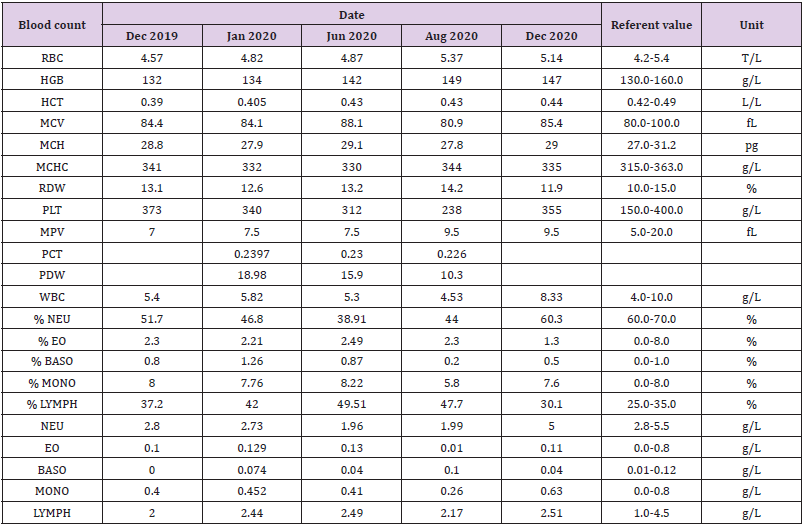
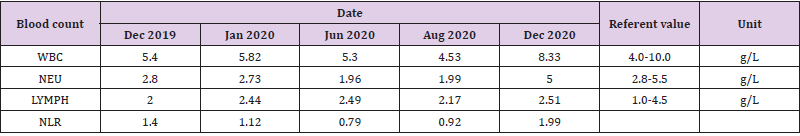
His mother was seeking help outside of the conventional medical approach, reaching to her research scientist friends in Vietnam and oversea. As provided by the mother, the patient was born lightly overweight (4.1 kg) and has itchy skin at birth. He got his first dent only at one year old and his nail grew slowly and has remained weak. No intensive treatment of neither antibiotic or anti-inflammatory drug was used prior to the appearance of alopecia areata. Eczema had appeared shortly before the hair loss. The patient’s blood test showed an IFG associated with hyperinsulinemia (Table 1, Dec 2019) and a severe inflammation in the white blood count panel (Table 2, Dec 2019 and Jan 2020). A reduction in Neutrophils and an increase in Lymphocyte count reflects a decrease in Neutrophils Lymphocytes Ratio (NLR) which is implicated in prognosis of systemic inflammation, infection and even cancer survivor rate (Bowen, et al. [6,7]). Since the naissance, the patient had had a conventional Vietnamese diet with high carb low fat meals consisting mainly of rice and vegetables. A part from 3 main meals, he had small snacks from 3 to 4 times a day which are formulated milk, soda, tropical fruits, potato chips, sweets and cookies. He pooped only every 3 days. From May 2020 we suggested his family to adopt an anti-inflammatory diet to first reduce the severe inflammation condition. The diet aims to eliminate the intake of all potential inflammatory elements such as lectin and omega 6.
In summary, the first diet plan excluded: All seed oils, all legumes, night shade vegetables, egg, coconut, nuts, rice, rice noodle, sticky rice, wheat flour, bread and all refined sugar food and drinks including soft drink, juices, sweet, cookies, ice cream, etc. Glutamate which is casually used in cooking in Vietnam as well as all prepared sauces which often contain high amounts of sugar were both removed from the diet. Soy and dairy products were also eliminated. Alternatively, all cooking and meal preparation used a generous amount of olive oil, butter and animal fat. Table salt was replaced by sea and Himalaya salt. Fruits were limited to avocado, berries and cucumber. Whole food consumption were mainly cruciferous and green leafy vegetables, aromatic herbs, grass fed meat and/or wild caught small size fishes. Bone broth and lemon juice were consumed daily. Red meat, organ meat, shellfish, fermented vegetables and prebiotic drinks (kombucha) were added regularly to his diet. He started with three meals per day with no snacks in between and eventually reduced to 2 meals per day for 3 or 4 day per week. By August 2020 (Table 1), his blood test showed a significant reduction in fasting insulin level (from above 123 to 7.4 μU/mL) while he was off of all his medications. He restored his blood Fe to normal level and slightly improved his white blood count panel (Table 2) showing promising recovery from both T2D and inflammation. Pooping frequency was also gradually improved, from once every three days to every 18-24h. The patient has stayed active and full of energy. He started regain height (from 139 cm to 141 cm).
In Dec 2020, his blood test showed an improvement in HbA1C (Table 1) and more importantly a significant improvement in white blood count (Table 2) and the NLR (Table 3) which shows no more inflammation. Nevertheless, his thyroid panel shows a tendency of hypothyroidism with the TSH closed to the upper limit (Table 2). From Dec 2020, the diet protocol was extended to a classical low carb high fat moderate protein diet. We re-introduced, with a moderate quantity of certain fruits and vegetables such as tomato without the skin and seed, pomelo, papaya and pomegranate; pumpkin seed and almond; heavy cream and high fat chesses; coconut milk and egg yolk. He continued to skip his breakfast 3 to 4 times per week with no snacks in between. He was supplemented with vitamin D3, vitamin K2, nutritional yeast for group B vitamin, zin, selenium, sea kelp, potassium citrate and magnesium citrate. In April 2021, his blood test showed that he is no longer IFG with a normal level of fasting insulin and C-peptide. He has recovered from the risk of hypothyroidism (Table 1) and continue to grow taller. All his antibody tests (ANA, ICA, GDA and TPO) for autoimmune disorders were negative (Data is not shown). His hair lost unfortunately has not shown any recovery.
Discussion
The rise of T2D mellitus in children in developing countries like Vietnam is regarded to be caused by the westernization of their conventional diet or the combination of both. Impact of the introduction of a number of snacks and high sugar beverages to the routine consumption upon three conventional meals filled with rice and starchy vegetables must be taken into account for T2D epidemics in Vietnam and Asia, especially in children of young age. Prior to the arrival of alopecia areata, the patient did not show any symptoms of T2D or autoimmune disorders. He was not overweight and didn’t endured any intensive treatment of antibiotic or/and anti-inflammation prior to the severe and rapid hair loss. As there were no blood tests for fasting glucose and insulin before starting the cortisol treatment, we cannot know if the treatment had contributed to graver his IFG and hyperinsulinemia condition. As alopecia areata is often associated with insulin-dependent diabetes (Wang, et al. [8]) and taking into account his previous diet, it is likely that he possessed a pre-existing hyperinsulinemia condition long before the appearance of the severe hair loss.
Routine screening for IFG and hyperinsulinemia in children is highly recommended for T2D prevention which will help to avoid such serious consequences to the physical, physiological and psychological conditions and the development of the child. Treatment of T2D mellitus in children by medication can be avoided by better management of diet and life style. However, it is challenging as successful employment of such changes in diet and lifestyle requires a strong willingness and collaboration of both the child and his family. Notwithstanding the social influences on the implementation of the diet as consumption of refined sugary foods, snacks and drinks are widely used and accepted at all social events. Despite all these difficulties and social inconveniences, the patient and his family have made a huge step forward, helping the child to recover from his diseases and to continue his growing curve right before entering puberty. His recovery encourages many others to take actions as showing that adopting an appropriate diet may not be an easy option but is the one that works.
Conclusion
Implementation of an anti-inflammatory diet followed by
an extension to low carb high fat diet has rescued the 9-year-old child,
now is 10 years old, not only from the development of T2D
mellitus but also the severe inflammation. Routine screening for
IFG and hyperinsulinemia in children is highly recommended
for the prevention of the T2D and therefore reduction of serious
complications and consequences.
For more Articles on : https://biomedres01.blogspot.com/




No comments:
Post a Comment
Note: Only a member of this blog may post a comment.