Outcome of Fetoscopic Laser Coagulation in 61 Pregnancies with Twin-Twin Transfusion Syndrome in Viet Nam
Introduction
Given the increasing implementation of assisted reproductive technologies in the reproductive medicine, the incidence of twin pregnancies has been continuing to rise [1]. Thirty percent of twin gestations have monochorionic placentas which are susceptible to complications because of their unique placental architecture [2,3]. Twin-to-twin transfusion syndrome (TTTS) is one of the most severe complications of monochorionic twin pregnancies, accounting for 15% of twin pregnancies [3,4]. When transfusion syndrome occurs, the two fetuses share different portions of the same placenta and connect with each other through placental superficial vascular anastomoses [2], leading to the poor prognosis for both two pregnancies. Approximately 90% of twins acquired TTTS result in intrauterine demise of one or both fetus or perinatal death without any intervention [5]. About 50% of surviving twins are likely to leave irreversible neurological sequelae such as brain white matter necrosis, ventricular hemorrhage, cerebral dilation, cerebral palsy, neurocognitive impairment, etc [6-8]. The donor twin experiences the reduction of circulatory volume, anemia, decreased diuresis, oligohydramnios, hypotrophy. Meanwhile the recipient twin is characterized by circulatory hypervolemia, cardiomegaly, heart failure, fetal edema. Consequently, twins are at high risk of intrauterine demise or irreversible nerve damage after birth.
Treatment for TTTS includes methods such as amniocentesis, opening the amniotic septum between the two fetuses, fetoscopic laser coagulation (FLC) of the blood vessels connecting the two fetuses, or clamping the umbilical cord. Until now, the FLC and umbilical cord clamp are the only solutions to solve the pathogenesis of the TTTS. FLC was firstly conducted by De Lia at al. in 1990 under laparotomy and general anesthesia [9]. Subsequently, FLC has been improved and implemented in TTTS treatment worldwide [10]. It is demonstrated to be a beneficial therapy over serial aminoreduction in numerous population-based study as well as randomized controlled trial [4,10,11]. FLC has been also presented to reduce the long-term neurocognitive impairment in twins [12,13]. In Vietnam, Tam Anh Hanoi General Hospital is currently the only hospital that can perform FLC. However, there is no any study discussing the outcome of FLC in TTTS in Vietnam. Therefore, we conducted this study to evaluate the safety and therapeutic efficacy of FLC and other related factors in the outcomes of TTTS.
Methods
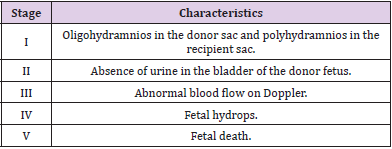
This is a prospective analysis study of pregnancies diagnosed with TTTS at the 16-26 week of gestation treated by FLC at Tam Anh Ha Noi General hospital, Vietnam. We included 61 consecutive pregnancies with moderate to severe mid trimester TTTS treated in our hospital of FLC between August 2018 and August 2019. This study protocol was approved by the Ethical Committee of Tam Anh Ha Noi General hospital on 1 August 1998. During the research period, all participants having TTTS confirmed by ultrasound and classified as the stage of II-IV (Quintero criteria) were extensively explained detailed risks and benefits of FLC. We only included participants accepting conducting the FLC and signing informed consent [14] [Box 1].
All procedures were performed under local anesthesia and ultrasound guidance. Firstly, the physician identified the position of fetoscope which is the most feasible position to approach the boundary line between the 2 amniotic chambers on the placenta surface from the amniotic fluid of the recipient fetus (Figure 1). In detail, this position has to allow the fetoscope parallel with the vertical axis of the donor fetus. Moreover, the attach positions of umbilical cords to placentas have to be observed clearly so that the conjunctive vessel will be detected more easily. Later then, the fetoscope (0°telescope, STORTZ) was introduced into the amniotic cavity of the recipient fetus and all the detected conjunctive vessels were coagulated along the whole vascular equator with a 0.4-0.6 mm fiber and laser system (20-40 watt of laser diot or laser YAGYttrium luminum Garnet).
The primary outcome was survival rate after 2 weeks of surgery and the live birth rate of one or both two fetuses. We also identified gestational age at delivery, the birth weight of neonate, the APGAR score and the weight of neonates seven day after birth as the secondary outcome variables. Gestational age in weeks was calculated based on the mother’s registration of her experienced due date. We divided gestation age at birth into very preterm (28- 31 weeks), moderate preterm (32-33 weeks), late preterm (34-36 weeks), early preterm (37-38 weeks), and full term (39-41 weeks). There was no post-term infants in the present prospective study. The birthplace at the Tam Anh hospital was only 21 pregnant women the remaining 40 pregnant women at the other 15 health facilities located in 14 provinces/cities nationwide.
Continuous variables are reported as mean and standard deviation (SD), categorical variables as absolute numbers and percentages. The differences in weight (percentage, %) was calculated by the following formulation ((weight of blood receiverweight of blood donor) *100/weight of blood receiver)) at the intervention time and the giving birth time, the end of gestation. Two-sided p<.05 were considered as significant using a t-test and odds ratio and 95% confidence interval. All statistical analyses were conducted with STATA Version 10.0.
Results
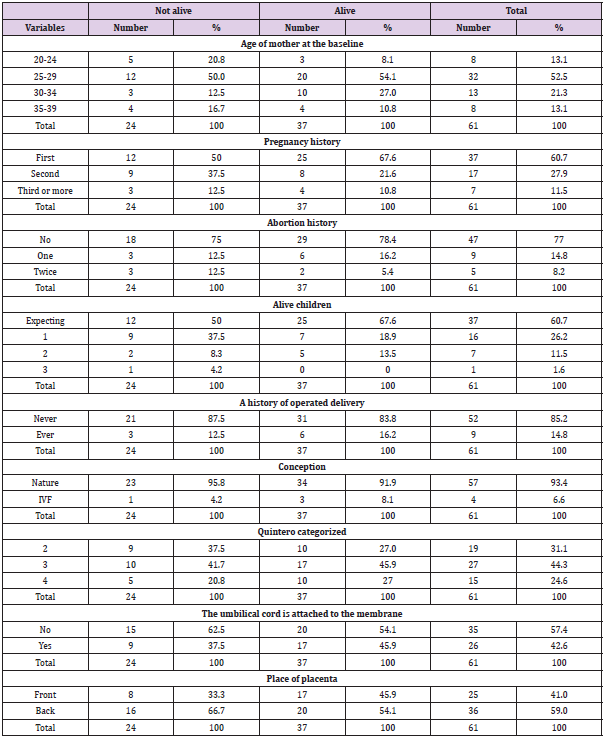
We recruited successfully 61 pregnant aged from 20 to 39, of which over 50% aged 25-29. Among them, 37 (60.7%) cases have reported having the first pregnancy, 17 (27.9%) cases having second pregnancy; 47 cases have no history of abortion and remaining 14 cases reported having abortion at least one time; 24 women have alive children and 37 other women with the first pregnancy. There was 52 women (85.2%) having history of caesarean section; 57 women (93.4%) have natural conception. 40.1% of case had anterior placenta, whereas 59.9% ones had posterior placenta. In included pregnancies, there were 26 cases having velamentous cord insertion. According to the Quintero staging classification, there was 19, 27, and 15 of pregnancies categorized to be stage II, III, and IV, respectively (Table 1).
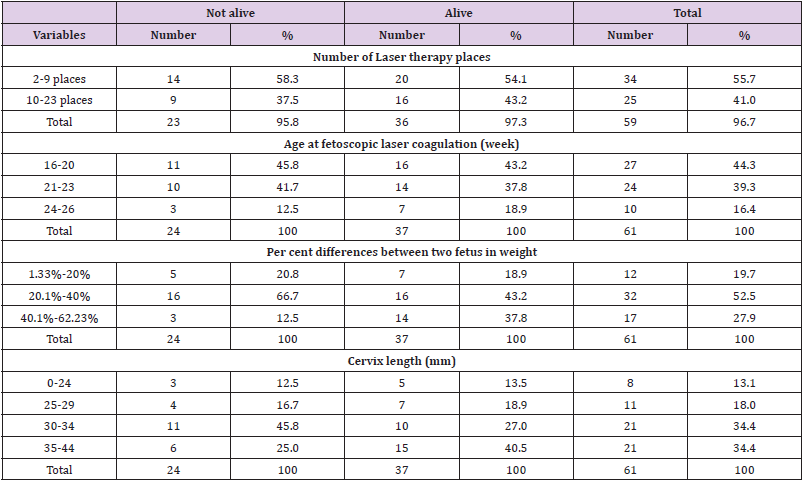
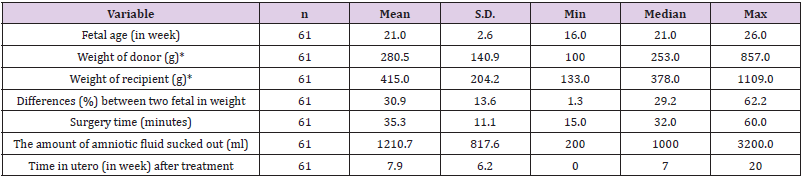
Cervix length (mm) was 0-24 (eight cases), 25-29 (11 cases), 30-34 (21 cases), and 35-44 (21 cases). The difference (percentage) in weight (g) between two gestations was 1.33%-20% (12 cases), 20.1%-40% (32 cases), and 40.1%-62.23% (17 cases). The age at FLC (in week) was 16-20 (27 cases), 21-23 (24 cases), and 24-26 (10 cases). The number coagulated vascular anastomoses was 2-9 places in 34 cases and 10-23 places in 25 cases (Table 2). The estimated average (mean +/- standard deviation (SD)) of surgery time (minutes) was 35.3+/-11.1; of the volume (ml) of drained amniotic fluid was 1,210.7+/-817.6; of the percent (%) of differences between two fetal in weight was 30.9+/-13.6. At the intervention time, the estimated weight (g) of donor was significantly lower (280.5g+/-140.9g) than recipient (415.0g+/- 204.2g), (Appendix Table 1).
Among 61 women, 15 cases were miscarriage after the intervention within 14 days after performed FLC, remaining 46 cases being followed up. Nine cases reported having neonatal mortality before or after delivery. There were 37 cases having babies survived for 7 days, at the last study follow-up, Figure 2. Among 37 cases having successful live birth, Quintero II, III, and IV was 10 cases, 17, and 10, respectively. The proportion of participants who have no survivors was gradually decreased by increased Quintero staging, 47.4% (9/19), 37.0% (10/27), and 33.3% (5/15) for the Quintero II, III, and IV, respectively, non-statistically significant, p=0.394. The gestation age (in weeks) at delivery was full term of 39-41 (3 cases), earlier preterm of 37-38 (4 cases), late preterm of 34-36 (9 cases), moderate preterm of 32-33 (8) and severe preterm of 28-31 (13 cases), Table 3.
All 61 pregnant were healthy by the last follow-up time and 37 of them (60.7%) having at least one liveborn neonate, of which six cases gave the single birth of the donor fetus, eleven cases gave the single birth of the recipient fetus, and 20 cases had successful birth of both twins. Newborn survived for 7 days was 57 (46.7% of 122 gestation). There were not significant differences in birth weight between 6 single survived donors (mean 1,858.3g) and 11 single survived recipients (mean 1,954.5g), but significant differences in birth weight, among 20 survived twins, between donor twin (mean 1,410.0g) and recipient twin (mean 1,782.5g) in 20 cases of twins’ delivery, Table 4. The average weight (g) of the neonate was significantly lower in both the group of the gestation donors (1,918.8g versus 1,333.3g, p=0.012) and recipients (2,260.0g versus 1,763.5g, p=0.041) when compared the categorized Quintero II to the categorized Quintero III-IV, Table 5.
When compared the indicators of the first ten performed cases to the last-ten cases, from the first to the last 61 participants consecutively recruited, the average surgery time was longer (41.4 versus 33.0 minutes) but the average number of coagulated vascular anastomoses vascular anastomoses was lower (6.3 versus 10.7). Among 20 surviving twins, the estimated differences (in percentage) in weight between donor and receiver gestations have continuously getting worse and increased in two cases, from 25.09% and 6.83% (at the treated time) to 43.75% and 21.74% (at the end of gestation), respectively. This difference in weight between donors and recipients has decreased in the remaining 18 cases.
Discussion
The successful FLC in our study was over 60% after seven days of birth with severe TTTS. The performed intervention was the first time successfully treated in Viet Nam and the achievements and main findings are significantly contributing to the develop the treatment technique of FLC for further better managements of TTTS in Viet Nam and at low- and medium economy countries. The proportion of Quintero stage IV in our study population was two time higher than the previous four studies combined (24.6% (15/61) versus 12.3% (46/373)) [15-18], indicating big challenges to manage maternal and neonatal health in the present project. The higher proportion of the late stage of Quintero might be due to lack of established health facilities and trained physicians in the rural province in managing TTTS in the country. Therefore, the pregnant came to our hospital at the advanced stage of TTTS. Moreover, due to limited participants’ resources and poor quality of transportation from other regions in the South and Central areas to the Hanoi city, only one third (21/61) participants have completed the recommended monitoring and following-up at our hospital that might cause a poor outcome of the present pilot intervention project. Therefore, social-determinant factors of maternal and child health were possibly related to the present intervention study.
The average age at the intervention time (week) in the present study was similarly to the other five previous studies [15-18], from 20 to 22 week. The estimated average surgery time in the present study (35 minutes) was longer than the other recent studies in Germany and France (27-29 minutes) [18,19]. Due to local limited quality of disinfection, some pregnant women were suffering from infection after completed intervention (2/61) resulting the premature ended of the gestation. This unwanted outcome was not seen in the other studies [20]. The average gestation age of newborn of 37 cases in the present study was approximately 4 weeks lower when compared to the previous 953 cases of nine studies combined (29 versus 33 weeks) [15,16,20-26]. After the intervention, these pregnant often came back to follow their pregnancies at the local hospitals at disadvantage areas that might be related to the shorter period of gestation age. The deficiency of well-trained physicians in managing of TTTS could contribute to the high rate of preterm birth in our study. Furthermore, as in the low economic status, the hard labor, the malnutrition in these pregnant could be also the explanation for this. The overall survival of at least one surviving gestation in the present study (60.7%) was lower than previous four studies (69.2%-84.0%) [11,21,27-29].
Because there was not significant difference in weight (g) between single surviving donors and single surviving recipients but it was observed among 20 surviving twins, the possible explanation is that the nature of limited amount of blood due to unknown related factors in the donors or the velamentous cord insertion involvement. Fifteen participants have no survivor (all had miscarriage within 2 weeks of treatment) and most of them among the first half time of recruited participants due to our limited experiences. The other 9 cases had neonatal death might be due to poor taking care by other local health facilities outside of our hospital in Hanoi city. In our study, the mean estimated surgery time in the first 10 cases is shorter than the last 10 cases. After some first cases, our team gradually got more experience and spent shorter time to find the vascular anastomoses positions and do the coagulation. Treatment technique in TTTS would be transferred from the established health facilities of developed countries to the other in the low- and middle economy countries and this work would be coordinated by an international association and institution in taking care better maternal and child health. We assume that there is an estimated 3.4% of pregnancy is twin, of which about 33% is monochorionic; about 66% of monochorionic has the blood vessels connecting the two fetuses and about 15% of them developing TTTS [30], among about 140 million pregnancy in 2020 worldwide, there was about 155,509 TTTS globally.
In order to improve maternal and child health, global project to manage TTTS is highly needed. With about million newborn per year, Viet Nam will have about 1,111 pregnancy that will be suffering from TTTS and the findings of the present project is timely and that will contribute greatly to manage TTTS in the country. The present study certainly has limitations including a lack of followup for about two-third of participants due to social-economy difficulties, limited local health facilities. Another limitation is the lack of neurodevelopment follow-up of delivered babies. In spite of these limitations, during 13 months running of the project, we just managed for only about 5.5% of the estimated 1,111 pregnancy with severe TTTS and the work would be improved for further better management and outcome of TTTS in Viet Nam in particular and in other low- and median economy countries.
Acknowledgement
We deeply appreciate study participants and their family members with their cooperation in taking care maternal and child health to manage TTTS in the present study.
Conflict of Interest
There are no conflicts to disclose.
Appendix Table 1: Estimated indicators of twin-twin transfusion syndrome when treatment was performed.



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.