The Relationship of Chronic Rhinosinusitis with Nasal Polyps and PDL-1
Introduction
Chronic rhinosinusitis with nasal polyps (CRSwNP) are benign inflammatory and hyperplastic outgrowths of the sinonasal mucosa [1]. It is a disease that seriously affects the quality of life of patients by causing nasal congestion, snoring, postnasal discharge, nasal discharge, loss of sense of smell/taste. The prevalence of CRSwNP is 1% to 4% in the general population [2]. CRSwNP is observed more frequently in male patients between the 4th and 6th decades [3]. İn histologically, nasal polyposis is characterized by respiratory epithelium covering oedematous stroma infiltrated by inflammatory cells [2]. Eosinophilic infiltration is the most common finding in polyp histopathology. In addition, there is an infiltration of inflammatory cells such as lymphocytes, basophils and macrophages.
Mucosal changes, including squamous metaplasia, secretory hyperplasia and epithelial cell proliferation, are observed in polyp tissues with the effect of chemical mediators secreted from these cells. T-helper 2 (Th2) cell-directed eosinophilia develops as a result of elevated immunoglobulin-E (IgE) and interleukin-5 (IL-5) [4]. In Asians, the majority of patients with CRSwNP show features of neutrophilic inflammation in addition to eosinophilia [5,6]. PD-1 (B7-H1,CD 274) is a protein-structured receptor belonging to the immunoglobulin superfamily found on the surface of activated T cells and antigen presenting cells. By binding to the PDL-1 ligand, T cell inhibition occurs and escape from the immune system occurs. PD-L1 works like a stop sign, inactivating the immune system’s T cells. One of the ways in which sick cells escape from the immune system is to densely host the proteins called PD-L1 on the cell surface. Studies have shown that PD-1 plays an important role in immune tolerance and in the regulation of T cell function [7].
Genetic studies have found that PD-1 gene polymorphism is associated with autoimmune diseases such as systemic erythematosus and rheumatoid arthritis [8,9]. PD-1 and PDL-1 are expressed in many different tumors such as lung carcinoma, lymphoma, pancreatic carcinoma, and renal cell carcinoma. It has been reported that PD-1 expression is increased in T cells in patients with CRSwNP with using flow cytometry [10]. This checkpoint led to the development of immune checkpoint inhibitors, which are the next generation immunotherapy drugs. These drugs prevent the interaction of molecules such as PD-L1 and PD-1, thereby activating the immune system against diseased cells. Among the immune checkpoint inhibitors nivolumab and pembrolizumab act by inhibiting PD-1 receptors, while atezolizumab and durvalumab act by inhibiting PD-L1 receptors [11].
If the importance of pdl1 in nasal polyp becomes clear, these immune checkpoint inhibitors drugs can be used in the treatment. There are not enough studies in the literature regarding the presence of PDL-1 in nasal polyps. In our study, our aim is to explain the presence of pdl1 in nasal polyp by immunohistochemical method. Detecting of the PDL-1 changes in nasal polyp tissue may explain the development of chronic rhinosinusitis with nasal polyps and may help develop new methods in the treatment of nasal polyps.
Materials and Methods
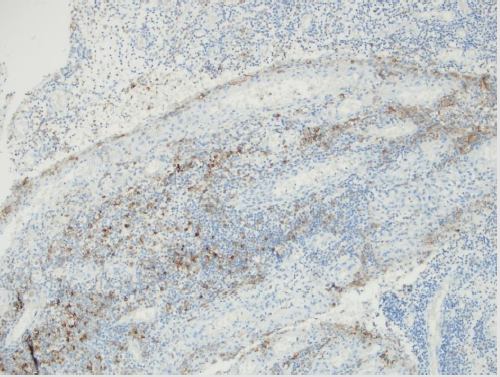
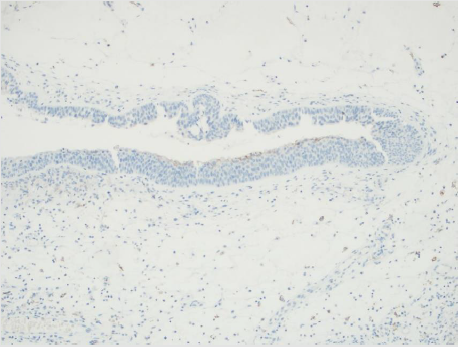
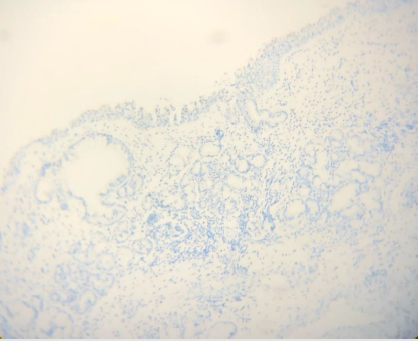
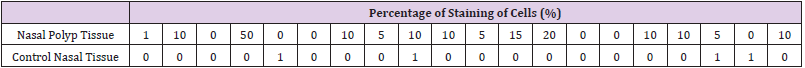
In our study, 20 patients who underwent endoscopic sinus surgery due to nasal polyps and 20 patients who underwent surgery for functional and/or aesthetic reasons and whose septum and turbinate mucosa were removed were included retrospectively, in Alanya Alaaddin Keykubat University Medical Faculty Hospital between 2010-2020. Previous sinus surgery, age is under 18 and nasal malignancies were exclusion criteria. 4 micron thick sections were taken from paraffin blocks for applying immunohistochemical PDL-1 antibodies. These sections were processed with Ventana PDL-1 (SP 263) monoclonal antibody on the fully automated Ventana Ultra Benchmark XT instrument. In the evaluation of PDL- 1 antibody applied immunohistochemically, the percentage of cells showing membranous staining with PDL-1 antibody was calculated among 100 tumor cells under light microscope. IHC staining results in groups were evaluated with Mann Whitney test using SPSS software version 22 (SPSS Inc., Chicago, IL, USA). P <0.001 was considered significant. Ethics committee approval was obtained from Alanya Alaaddin Keykubat University (no:2021/09-06).
Results
There were 2 female and 18 male patients in the study group, and 4 female and 16 male patients in the control group. The mean age was 37.4±8.6 years in the study group and 35.4±8.8 years in the control group. PDL-1 positivity in nasal polyp tissues was significantly higher than normal nasal mucosa epithelium. (P=0.000) (Table 1) (Figures 1-3) The recurrence rate was higher in PDL-1 positive cases with nasal polyps, and the recurrence rate increased as the staining rate increased, and it was statistically significant. (P=0.003).
Discussion
There are some hypotheses exist for how CRSwNP develops but the aetiopathologenetic mechanism of it is still unclear [2,12]. The pathogenesis of it is thought to involve persistent inflammation of the nasal mucosa due to infiltration by eosinophils, basophils, lymphocytes, neutrophils and mast cells [2]. T lymphocytes act as the main actor in this inflammation process. PDL1 İs a member of the B7 family that regulate the T-cell response and a predictive biomarker. It is a cell-surface glycoprotein primarily expressed by antigen-presenting cells. Studies on PDL 1 in the literature are mostly about tumor cells. Different cut-off values have been reported in these studies [13-16]. However, variable cut-off levels create difficulties for researchers in making decisions during evaluation. Determining a standard cut-off value for researchers is important for the correct interpretation of the results and for the consistency between the results of the studies. In our study, we considered the presence of PDL-1 positive in staining of 1% or more. Different companies have antibodies and subclones for PDL- 1. In the literature, there are studies reporting different results with antibodies and clones of different companies in the same cell group [17,18].
We used the SP263 clone of Ventana, which is frequently used in studies in the literature, to increase the staining quality and the reliability of the results. There are studies explaining that the infectious process plays a role in the pathogenesis of CRSwNP [19,20]. İt is reported that IFN-γ secretion increases after incubation of lymphocytes with bacterial and fungal extracts [21,22]. IFN-γ is an important cytokine thas is a strong inducer of PDL-1 expression [23]. Before studies showed IFN-γ have been identified in nasal polyposis [24,25]. PDL-1 levels in other cell membranes increases by the IFN-γ charged by T-cells. Thus, it causes a negative feedback in nasal polyposis by causing down-regulation of T-cell responses. İn a study about mRNA expression of PDL-1 in patients with CRSwNP, resarchers found mRNA levels of PDL-1 was increased in nasal polypies epitel compared to healty nasal tissue epitel [26].
Although there are studies in the literature that measure PDL1 level in nasal polyp tissue and blood cells by PCR and flow cytometry, but there is not enough study in which the pDL1 level in nasal polyp tissue is analyzed immunohistochemically. In a small study in the literature using only 3 nasal polyp tissues and 3 nasal tissues as control, immunohistochemical evaluation was made and PD-1+ cells were indeed increased in the submucosa of NP tissue compared to control tissue [27]. İn our study we found that the pdl1 level in CRSwNP tissue was significantly higher than the pdl1 level in the control healthy nasal tissue, and it was was statistically significant. (p:0.01). For this reason, the use of monoclonal antibodies developed against PDL-1 as a target drug as a non-surgical drug therapy in nasal polyps is a matter of debate. Recurrence in surgical procedures is an undesirable situation for the patient and the surgeon. Different researchers used several markers for predicting nasal polyp recurrence.
Recurrence is frequently observed in nasal polyposis, and recurrence is higher in eosinophilic polyps than in noneosynphilic polyps [28]. Zhong et al. in their study, the relationship between peripheral eosinophil count and recurrence was examined and they found a significant correlation between high peripheral blood eosinophil count and recurrence [29]. In another study showed researchers that a tissue eosinophil proportion of >27% of total cells was a marker for recurrence within 2 years after endocopic sinus surgery in patients with CRSwNP [30]. In our study, recurrence rate was high, and it was found in 10 (50%) patients. The recurrence rate was higher in PDL-1 positive cases with nasal polyps, and the recurrence rate increased as the staining rate increased, and it was statistically significant. (P=0.003) These findings suggest that the presence of PDL-1 may be a predictive factor for recurrence.
Limitations
The most important limitation of our study is that it was a retrospective study, and we could not reach sufficient patient material, since the operated patients took the operation materials to an external center for histopathological consultation. It will be possible to make a clearer comment on the fact that it is a determining factor in the development of recurrence.
Conclusion
PDL-1 was significantly increased in our patients with CRSwNP compared to normal nasal mucosa tissue. Presence of PDl-1 is a predictive factor for recurrence in nasal polyposis. Since there are not many studies explaining the presence of CRSwNP and PDL- 1 in the literature, we think that our study will contribute to the literature. New studies with a larger number of patients are needed to determine the presence and importance of PDL-1 in nasal polyps.



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.