Cognition and Omega-3 Fatty Acids: A Narrative Review of the Literature
Introduction
Today we know quite well that a healthy lifestyle that includes physical activity, healthy eating or moderating toxic habits such as alcohol and tobacco are associated with a lower risk of suffering from some diseases such as cardiovascular diseases, some types of neoplasms, and neurodegenerative diseases in general, and particularly cognitive impairment or dementia. The dietary factor is perhaps the most complex, and much research is aimed at elucidating which foods are associated with this beneficial effect and why. To this respect, one of the most implicated actors in this positive effect has shown to be polyunsaturated fatty acids, especially those belonging to the omega-3 group. Fatty acids are biomolecules consisting of a linear hydrocarbon chain of variable length, with a carboxyl group (-COOH) at one end and a methyl group (-CH3) at the other. The carbon atoms in the chain are joined by single or double covalent bonds. The absence of double bonds defines the acid as saturated, while the presence of one double bond in the chain defines it as monounsaturated acid, and the presence of multiple double bonds as polyunsaturated. Polyunsaturated fatty acids are known by their acronym PUFAs (Poly Unsaturated Fatty Acids). Omega-3 fatty acids (ω-3), together with omega-6 fatty acids (ω-6), make up the group of so-called essential fatty acids, which owe their name to the fact that they are essential for the body since the body is not capable of producing them on its own and must acquire them from foods that contain them. Whether a fatty acid is referred to as omega-3 or omega-6 is established by the location of the first double bond from the methyl-terminal end. In omega-3s, the double bond is at carbon 3 [C3-C4] and can also be identified as n-3. In omega-6, the double bond is at carbon 6 (C6-C7) and is also known as n-6.
Excessive amounts of omega-6 polyunsaturated fatty acids (PUFA), marked by an increased dietary high omega-6/omega-3 ratio, as is increasingly common in current Western diets, are currently speculated to promote the pathogenesis of many diseases, including cardiovascular, cancer, inflammatory and autoimmune diseases [1]. In contrast, omega-3 fatty acids have been shown to play an important role in altering blood lipid profiles and membrane lipid composition and affecting eicosanoid biosynthesis, cell signaling cascades and gene expression, which positively influences health status. This effect seems to have been proven in cardiovascular diseases [atrial fibrillation, atherosclerosis, thrombosis, inflammation, and heart disease, among others], diabetes, cancer, depression, or autoimmune diseases (e.g., rheumatoid arthritis). Its beneficial influence on brain function in the diet of pregnant and lactating women has also been studied [2,3]. The first evidence of this beneficial effect was provided by epidemiological studies which revealed that the traditional Greenlandic diet, rich in marine mammals and fish, reduced the incidence of cardiovascular disease in both the Inuit population and in the Danish people who immigrated to these latitudes, belonging to a different ethnic group [4]. There is currently a tendency in today’s diets to over-consume omega-6 in relation to omega-3 due to the high consumption of vegetable oils by Western society, which means that this ratio can be as high as 20:1, very different from the current recommendations which advise that the omega-6/omega-3 acid ratio should be approximately 4:1, as was the case until the beginning of the 20th century. We could hypothesize that diets rich in omega-3 polyunsaturated fatty acids would be beneficial for the functioning of neural structures, since one out of three fatty acids in the central nervous system are long-chain polyunsaturated fatty acids, and it could be thought that an inadequate balance between these (ω-6/ω-3) would lead to neuropsychological alterations [5].
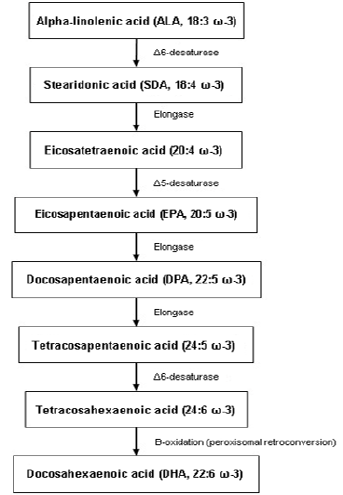
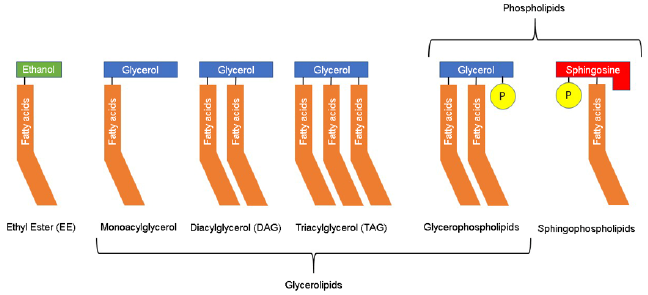
Omega-3 PUFAs originate mainly from the marine environment or the vegetal kingdom and include α-linolenic acid (ALA; 18:3 ω-3), stearidonic acid (SDA; 18: 4 ω-3), eicosapentaenoic acid (EPA; 20:5 ω-3), docosapentaenoic acid (DPA; 22:5 ω-3) and docosahexaenoic acid (DHA; 22:6 ω-3). Some plant seeds, such as flax, chia and canola seeds, are good sources of ALA, which serves as precursor for the synthesis of other long-chain PUFAs (see Figure 1) in the human body such as DHA or EPA. However, the production of longchain ω-3 PUFA from ALA is very limited, with conversion rates of around 5% through this metabolism. Therefore, the best sources of PUFA ω-3 are those of marine origin. Long-chain ω-3s, such as EPA and DHA, are found in the lipids of fatty fish; in the fat tissue of marine mammals; in algae and marine fungi; as well as small crustaceans that are part of krill. The bioavailability of ω-3 PUFAs is also influenced by the organic structure of the ingested form from the diet (see Figure 2), whether ethyl ester (EE), triacylglycerol (TAG) or phospholipids (PL). The most common form of lipids in nature is TAG, which has the best bioavailability compared with EE. PLs are rare in nature and data on their bioavailability are limited and inconclusive [4]. For these reasons, most supplements are made from fish oils or other marine organisms such as krill, as the bioavailability of these products is higher than with vegetal origin products, in addition to the higher proportion of long-chain omega-3 PUFA (DHA or EPA) of higher biological value [6].
The ω-3 PUFAs appear to exert a very important action on neuron membranes, especially in the synaptic regions of neurons (and to a greater extent, in areas of grey matter), where they accumulate in greater proportion and are essential components of the phospholipid membrane, so their importance is vital for the stability of the dynamic structure and functional activity of neurons, as they can alter the fluidity of the lipid membrane (displacing cholesterol from it) and promote synaptic plasticity, which is essential for learning, memory and other cognitive processes. They also act as sources of communication for second messengers between neurons, enhance the coupling of G-proteins involved in many signal transduction pathways and are involved in direct lipid-related transcription functions. DHA, one of the most important and final products of their metabolism (see Figure 1), constitutes more than 90% of the ω-3 and 10% to 20% of the total lipids in the brain. It is mainly incorporated into phosphatidylethanolamine, phosphatidylserine and, in smaller amounts, into phosphatidylcholine in synaptic terminals, mitochondria and endoplasmic reticulum. In fact, DHA is able to modulate cellular properties and physiological processes such as membrane fluidity, neurotransmitter release, gene expression, myelination, neuroinflammation and neuronal growth [6].
The purpose of this review is to examine the current evidence on the relationship between dietary omega-3 supplementation and improved cognition or prevention of cognition-related diseases such as Alzheimer’s disease (AD). To this end, we will discuss the evidence both for and against, in preclinical experiments as well as in clinical studies in humans, including normal ageing, subjective memory or cognitive complaints, mild cognitive impairment, and even AD.
Preclinical Data
The potential effect of omega-3 fatty acids on cognition has been studied in multiple experimental preclinical studies in animals, both in models of normal ageing and in models of AD. The most common model of normal animal ageing is the canine model. Dogs are capable of developing age-related cognitive decline similar to that found in humans and their diet is similar to ours [7]. They can therefore be used to study the potential effects of nutritional supplements in controlled settings. Most studies use nutritional supplements that combine different types of omega-3s, as well as amino acids and antioxidants. The results obtained in these studies support the hypothesis that these supplements would have a beneficial effect on cognition and learning in older animals [7-9], although there are some studies that do not find these benefits [10].
AD models are usually conducted in rodents. These often consist of transgenic strains with mutations that predispose to developing the disease and have been used extensively in AD treatment research. Most studies of omega-3 supplementation in these animal models have shown benefits on delayed cognitive impairment [11], cognitive decline, behavioral symptoms [12], and have even shown to reduce beta-amyloid deposits [12]. An interesting study used transgenic mice for amyloid precursor protein (APP)-animal model for AD-, compared with others that carry the same pathogenic mutation together as well as another mutation that induces the passage of endogenous omega-6 to omega-3, obtaining that the latter showed a lower progression of cognitive and behavioral symptoms compared to the former, displaying the potential protective effect of omega-3 versus omega-6 [13]. This beneficial effect of omega-3s is also observed in other studies in a murine model of epilepsy [14]. In contrast, other studies have not found this beneficial effect in transgenic mice, although they do find it in normal mice [15].
Clinical Evidence
Normal Ageing
We have found and reviewed 13 randomized trials examining the effects of omega-3 dietary supplements in healthy elderly subjects, looking at their cognitive performance. Most used DHA supplements, sometimes combined with EPA, with a daily dose ranging from 350 mg to 3,000 mg of DHA obtained from fish oil in most cases, and in one case from krill [16]. Cognitive performance was measured using a cognitive assessment protocol that typically includes tests of memory, attention, working memory, verbal fluency, and processing speed [17]. The results of most of them showed significant differences when assessing the cognitive effects of omega-3s [16,18-23]. One of the studies used the measurement of P300 evoked potentials as the primary endpoint, resulting in an improvement in the omega-3 treated group [24].
In other studies, on the contrary, no significant differences were found in the parameters evaluated, although most of them used lower daily doses (200-300 mg DHA), compared to the previous studies [25-27], or otherwise the sample size was small [28], which could explain this difference in results. The exception is the study by Danthiir et al. which used high doses (1,720 mg DHA) and only obtained a slight tendency towards improvement in some of the evaluated endpoints [29]. In addition to the above, mention could be made of the Spanish WAHA study, which did not examine the direct effect of omega-3 supplements but studied the effect of a dietary supplement with walnuts in a population-based cohort. Although there were no significant results in cognitive variables after two years of intervention, improvements in functional networks mediated by functional magnetic resonance imaging (fMRI) during working memory tasks were shown [30].
Subjective Memory Complaints
Studies related to subjective cognitive, or memory complaints are scarce, perhaps because the concept is more difficult to categorize or define than normal ageing or the “classic” mild cognitive impairment or dementia. By subjective memory complaints (SMC) we mean individuals who present a subjective perception of poor cognitive performance in general [and memory in particular] but which present a neuropsychological examination within the normal range. It has been established that this altered perception of one’s own cognition could be caused by the onset of a very incipient cognitive impairment which eventually cannot be detected in neuropsychological tests, or by a poor estimation of one’s own abilities (meta-cognition) due to executive dysfunction [31].
The main study in this subgroup of subjects is the MAPT study which randomized French elderly people to multi-domain intervention groups [cognitive stimulation, physical activity, and nutrition], to omega-3 supplementation or both interventions versus placebo. This study found no improvement in patients who underwent intervention [32]. Anyway, a subgroup analysis subsequently found that omega-3 supplementation would be partially beneficial in those subjects who had low baseline omega-3 levels [33]. Another ambitious trial in this population subset is the PONDER study, for which no results have yet been obtained [34]. Otherwise, some studies have found objective improvements on cognitive performance or in regional blood flow measured by fMRI in the posterior cingulum [35-37].
The study by Yurko-Mauro et al. in patients with memory complaints who met criteria for “age-related cognitive decline” has been considered as positive. This is a randomized, doubleblind, placebo-controlled clinical trial in which 900 mg per day of DHA (n=242) or placebo (n=243) was administered to individuals with memory complaints of average age 70 years for a period of 6 months, showing statistically significant differences in favor of DHA administration in validated cognitive tests frequently used for the assessment of memory and learning ability. The authors concluded that DHA supplementation at a dose of 900 mg/day improved memory and learning capacity in individuals with SMC [35]. In addition, there is a meta-analysis evaluating the results of 15 clinical studies, most of them observational, which concluded that DHA/EPA supplementation has a beneficial effect on memory in adult individuals. The review concludes that episodic memory tests of adults with SMC were significantly improved (p<0.004) with DHA/EPA supplementation. Furthermore, and regardless of cognitive status at baseline, DHA/EPA supplementation [at doses >1 g per day] was able to improve episodic memory (p<0.04). Changes in semantic and working memory from baseline were significant with DHA, but no differences between groups were detected [38].
Mild Cognitive Impairment
Mild cognitive impairment [(MCI) is probably the main risk factor for developing dementia, and specifically amnestic MCI (the most prevalent entity) is the most important risk factor for the development of AD. For this reason, preventive treatments have become a relevant source of study in patients with MCI, as they could have a potential role in the prevention of AD. Currently, there is no drug approved for use in MCI, but some strategies such as cognitive stimulation, physical exercise, and dietary recommendations, including omega-3 PUFAs, are under study. Randomized clinical trials that have studied the effect of omega-3 PUFA in patients with MCI have been reviewed. Most studies showed improvements in scores on working memory tests, as well as episodic memory [39- 41], although there are others that evaluated test scores (FSIQ -Full Scale Intelligence Quotient- and WAIS -Wechsler Adult Intelligence Scale), or even depressive symptom scales (GDS -Geriatric Depression Scale) [42,43], which concluded with positive results in favor of omega-3 supplementation. All the mentioned studies above followed patients for 6 months to one year, while studies with shorter follow-up did not seem to obtain statistically significant differences [44].
Additionally, there have been several published meta-analyses and systematic reviews on the effect of omega-3s in patients with MCI. The overall conclusion of all of them points to the beneficial effect of omega-3 PUFA in MCI patients [45,46]. The most recent meta-analysis of 25 studies (n=787) indicated that omega-3s appear to have no effect on overall cognitive function (Hedge’s g= 0.02; 95% confidence interval= -0.12 to 0.154), although it may have a beneficial effect on memory (Hedge’s g=0.31; p=0.003; z=2.945) [46]. Another meta-analysis by Zhang et al. analysed all studies in which the MMSE (Mini Mental State Examination) was used for the assessment of these patients treated with DHA/EPA supplements and concluded that the treatment seems to statistically decrease the rate of cognitive decline in terms of MMSE score (WMD=0.15 (0.05-0.25); p=0.003), so the hypothesis that omega-3 could help to prevent global cognitive decline -in addition to memory- in elderly people with MCI seems to be supported [47].
Neuroimaging research has looked at the effect that omega-3 PUFA may have on the brain in patients with MCI. One of these studies used fMRI to study regional blood flow. It appeared that treatment with omega-3 for 26 weeks is able to increase blood flow in posterior cortical areas, typically affected in MCI [48]. Another study analysed the evolution of brain volume measured by MRI in patients with MCI with results showing that, after treatment with DHA supplementation for one year, the hippocampal volume measured by brain MRI was larger in treated patients than in those receiving placebo [49].
Alzheimer´s Disease
There have been numerous studies on omega-3 PUFA in AD with overall slightly favorable results. In this context, multiple randomized, double-blind, placebo-controlled trials have been conducted, some of which have had great scientific impact. So far, no treatment has been found that is able to significantly improve AD, so most studies are trying to elucidate whether treatments are able to reduce the degree of disease progression. One of the first studies that attempted to address the effect of omega-3s on the progression of AD was the Omega AD study. In this study, patients were treated with high-dose DHA and EPA (1.7 g DHA + 0.6 g EPA) versus placebo, with omega-3 supplementation in both groups continuing for a further period from 6 months to 1 year. The main publication derived from the research showed a tendency for the treatment group to have less disease progression at the cognitive level [measured by MMSE and ADAS-Cog -Alzheimer´s Disease Assessment Scale-Cognitive], although significant differences were only obtained in the mildest AD subgroup [50]. In this trial, a better outcome in patients with higher plasma levels of omega-3 was found [51] and also in those with higher homocysteine levels, which the authors relate to a hypothetical synergistic effect with B vitamins [52]. The same study attempted to assess the efficacy on behavioral symptoms without improvement, with the exception of depressive symptoms, a finding that has been observed in other settings of cognitive impairment [53]. This beneficial effect of omega-3s has been replicated in other clinical trials using similar doses of DHA for 6-12 months with improvements in cognitive scales such as the ADAS-Cog [54–56].
On the other hand, some studies have found no significant differences in terms of cognitive assessment [44]. The most relevant is that of Quinn et al., concluding that treatment with DHA (2 g/day) for 18 months did not produce a relevant cognitive effect as measured by MMSE and subscales of the ADAS-Cog [57]. Studies related to some complex nutrient formulations with high doses of omega-3 PUFA in their composition [1200 mg DHA + 300 mg EPA per 125 ml] are worth mentioning. Some studies with these products have shown beneficial effects of daily treatment. The primary endpoint of the trial was the change in memory as measured by the NTB [Neuropsychological Test Battery] Z-score at 24 weeks of treatment. The study showed statistically significant differences in NTB score in favor of the treated arm [p=0.023; Cohen’s d=0.21; 95% confidence interval (-0.06 - 0.9)) [58,59].
Conclusion
Although evidence is not conclusive, several investigations support that supplementation with omega-3 PUFA, especially DHA, may have beneficial effects on cognition in healthy older adults with SMC and even in patients with MCI or AD. These effects should generally appear at high daily doses [800-900 mg and above] and over long periods of time (6 months or longer). This protective effect has not been shown in all studies, so it is possible that the results may be influenced by other variables; in this sense, it is important to mention that ensuring adequate long-term adherence to treatment [at least 6-12 months] may be important to establish a possible objective benefit. Anyway, more soundly designed interventional clinical trials are needed to ascertain relevant issues concerning dose and supplementation duration. It has been found that plasma omega-3 values or homocysteine levels may be related with these discrepancies among different studies, with subjects with lower plasma omega-3 and homocysteine levels benefiting more from this effect. In any case, these supplements appear to have no relevant adverse effects and may have other added benefits such as reduced cardiovascular risk. Moreover, their indication is not at odds with other recommendations such as cognitive stimulation and physical exercise, so that, altogether, these measures can be medically recommended.



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.