Efficacy of Particulate Versus Non-Particulate Transforaminal Epidural Steroid Injections in Relation to their Complication Risk
Introduction
Transforaminal epidural steroid injections (TFESI) are widely used interventional procedures for diagnosis and treatment of spinal nerve pain and pathologies. Two broad categories of corticosteroids exist: those that contain particles and those without. The most well-known non-particulate steroid (NPS) is dexamethasone and the most popular particulate steroids (PS) are betamethasone, triamcinolone and methylprednisolone [1]. Steroid categorization is based on solubility properties in water as well as the propensity to aggregate in various solutes. PS range in size from 0.5-100um, though aggregates can reach sizes of 1000um [2]. In contrast, the average red blood cell is 7um [3]. Interestingly, betamethasone can fall into both categories based on preparation. The acetate version is considered a PS whereas the sodium phosphate version is considered NPS [2]. The significance of these particles and aggregates lies within the embolic risk if inadvertently injected intravascularly, leading to spinal or brain ischemia. In 2014, the FDA investigated multiple case reports of catastrophic post-injection complications including paralysis, spinal infarct, ischemic stroke and death [4]. The FDA’s Adverse Event Reporting System (FAERS) database and the medical literature between 1997 and 2014 were reviewed. A total of 90 serious complications after epidural steroid injections were identified. Type of corticosteroids used were generalized and never specifically identified by the FDA. However, subsequent review of the literature revealed that these complications occurred with particulate steroids. In 2014, the FDA required relabeling of PS products to include reports of serious medical events [4-6]. Despite the new FDA warnings, most practitioners still utilize PS for TFESIs likely due to availability, training, physician preference and a persistent belief that PS are superior in efficacy. Proponents of PS point to the theoretical benefit of a local depot effect where larger particles absorb slower due to their local accumulative nature. These slower diffusion rates would then result in longer lasting effects [7]. Proponents of PS also suggest that intrinsic risks are associated with all spinal injections including vasospasm, vertebral artery dissection and air embolization. Vasospasm can occur after arterial irritation due to alpha-1 adrenergic activation and resultant vasoconstriction. If prolonged enough, this vasoconstriction can cause ischemia. Dissection can occur with any needle trauma separating the tunica intima from the media. This can then shunt blood into the false lumen causing distal arterial ischemia.
Air embolization can occur with any interventional procedure that involves injections. If the syringe is not correctly prepared, air particles can be injected into the artery causing embolization of the artery [8-10]. There are few reports in the literature of these types of adverse events [11-13]. Though there has been a longstanding divide between those who advocate for PS vs NPS for transforaminal epidural steroid injections, the issue has come to the forefront with the introduction of new Spine Intervention Society (SIS) guidelines [14]. The purpose of this study is to review current evidence regarding efficacy and potential complications of PS versus NPS.
Methods
A literature review of available evidence was conducted utilizing Google Scholar and PubMed databases. Key search terms included: transforaminal epidural steroid injections, complications, efficacy, particulate steroids, non-particulate steroids, dexamethasone, methylprednisolone, betamethasone and triamcinolone. Studies that involved exclusively interlaminar epidural steroid injections were excluded. No limitations for publication date were implemented. The snowball method was then employed by reviewing reference lists of included articles for any additional relevant primary articles.
Results
Complications
TFESI are very low risk procedures; however, rare but serious side effects can occur. Since the FDA investigation into neurological complications, several studies have retrospectively investigated complications arising from TFESI. One such retrospective cohort study used HIRA claims to find patients who underwent TFESI from 2009 to 2014 and subsequently presented to the emergency department within 24 hours of the procedure. 830,000 cases were found and the incidence of neurological complications, including infections, hypotension, seizure, stroke, spinal cord injury, and death, for PS versus NPS was 1.73 and 0.9 per 100,000, respectively. Interestingly, neurological complication rates did not differ between NPS and non-steroid injections [6]. A larger study by Scanlon, et al. [13] aimed to determine the prevalence of neurological injuries within the current population. A survey was sent to all physician members of the American Pain Society. Respondents were asked about awareness of complications, year, practice setting, use of imaging, contrast, type of steroid, doses administered, and advanced imaging findings. 287 respondents reported 78 complications including 16 vertebrobasilar brain infarcts and 12 cervical spinal infarcts. 13 of the 78 cases were fatal. Methylprednisolone was used in 79% (22 of 28) of cases, betamethasone in 11% (3 of 28), and triamcinolone in 11% (3 of 28). Dexamethasone use was not reported in any of the complications. The majority of serious complications were due to infarcts; however, there was 1 case of both air emboli and vascular dissection [13].
In addition to these retrospective studies, there are multiple case reports of neurological events after TFESI [12,15,16]. To date, there are only 2 case reports of complications associated with NPS. The first was reported by Boudier-Revéret [11], where a 39-year-old man presented with involuntary movements of the bilateral upper trapezius muscles after a right C6/7 TFESI with 5 mg dexamethasone. MRI of the brain and cervical spine revealed no specific lesion and electroencephalography showed no abnormal findings. The myoclonus gradually improved and resolved completely within two weeks. It was difficult to discern the root cause of the myoclonus; however, it was thought to be from trauma leading to subacute spinal neuritis during neuraxial anesthesia. The second case reported acute right lower extremity weakness accompanied by a right-sided foot drop and sphincter dysfunction after a dexamethasone right L5 TFESI [12]. MRI showed significant disc herniations at the L4-5 and L5-S1 levels, contributing to moderate central/foraminal stenosis but no acute findings. EMG demonstrated acute denervation potentials in L5-S1 distributions. Emergent L4-5, L5-S1 laminectomy with discectomies at the L4-5 and L5-S1 levels was performed. Immediately after surgery, the patient’s weakness and sensory deficits improved. The authors attributed this patient’s neurological deficit to an acute increase in mass effect from the volume of injectate, resulting in ischemia.
Efficacy
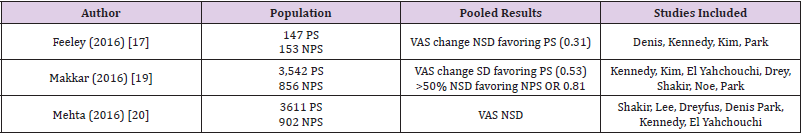
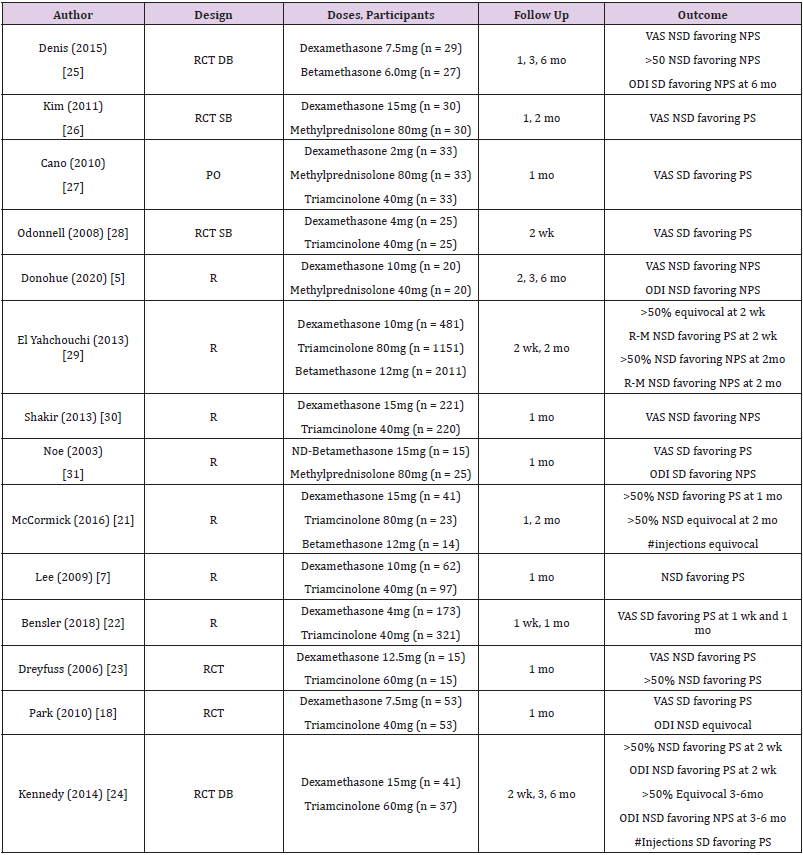
The efficacy of NPS versus PS for TFESI continues to be an area of controversy. An extensive evaluation of the literature shows multiple studies comparing the two. One large literature review conducted by Feeley and colleagues found four compatible studies comprising 300 participants undergoing 147 PS injections and 153 NPS injections [17]. Analysis showed no statistically significant difference in VAS data between the PS and NPS groups (0.31). There was however, a slight non-significant VAS improvement in those receiving PS injections. This review did include one study, Park, et al. [18], that showed a significant difference in VAS favoring PS over NPS injections. A larger systematic review and meta-analysis by Makkar et al. included studies that compared the efficacy of PS with NPS in TFESI [19]. Seven studies met criteria and included 3,542 PS and 856 NPS injections. Pooled average VAS scores were significantly different with 0.53-point greater VAS change for those receiving PS compared to NPS injections. However, the NPS group had a larger proportion of patients with more than 50% pain relief (OR 0.81). Once again, Park, et al. [18] was included in this review as the only study that reported a statistically significant difference in VAS scores between PS and NPS injections. A third meta-analysis by Mehta et al. also reviewed studies comparing 3611 PS and 902 NPS in TFESI [20]. Here, TFESI results were evaluated in 7 separate studies and again showed no significant difference in VAS scores between the two groups. Table 1 shows a summary of the 3 large systematic review studies and their results. While each review analyzed a different pool of studies, there was a fair amount of overlap. There were a few studies that were not included in any of the above analyses. These included McCormick et al., which studied 78 patients with three separate steroids and found no significant difference in the number of repeat injections required for pain relief, but slightly favored particulates for short-term pain relief [21].
Table 1: Systematic reviews comparing particulate and non-particulate steroids.
Note: NSD = No significant difference, SD = Significant difference
Greater than 50% relief was seen in 35% of those receiving PS and 28% of those receiving NPS injections less than one month after injections (<1 mo). Greater than 50% pain relief was seen in 40% of those receiving PS versus 39% receiving NPS injections greater than one month following the injections (>1mo) [21]. A second retrospective self-controlled study completed by Donohue et al. included 40 patients receiving 20 PS and 20 NPS injections. Non-particulates were favored when looking at both VAS score and function outcomes [5]. Additionally, Lee et al. included 159 patients (97 receiving PS, 62 receiving NPS) who underwent cervical TFESI and evaluated pain scores at 1 month. Outcomes were similar to other studies, showing relief with PS in 80.4% of patients versus 69.4% with NPS, although this difference was not statistically significant [7]. There have been a limited number of studies that have demonstrated a significant benefit of particulate over non-particulate steroids for TFESI. These include Bensler, et al. [22-24,18]. Bensler et al. performed a retrospective comparative review on two cohorts in which one group (N=321) was treated with 40mg triamcinolone and the other group (N=173) received 4 mg dexamethasone. PGIC scoring showed a significantly higher proportion of patients improved at 1 week (43.2% versus 27.7%) and one month (44.3% versus 33.1%) with PS over NPS [22]. Dreyfuss et al. completed a study involving 30 patients (15 PS, 15 NPS) and found the effectiveness of dexamethasone 12.5mg to be non-significantly less than that of triamcinolone 60mg at 1 month. However, a greater proportion of the dexamethasone group (27%) obtained complete relief of their pain than in the triamcinolone group (7%), but this difference was not statistically significant [23]. Another RCT that favored PS over NPS was completed by Park and colleagues in which 106 patients underwent TFESI (53 NPS 7.5mg dexamethasone, 53 PS 40mg triamcinolone) and showed significant improvement in the particulate group at 1 month [18]. For the dexamethasone group, the reduction of pain score was 40% whereas that of the triamcinolone group was 71%.
A final multicenter double-blind RCT of 78 consecutive subjects was completed by Kennedy, et al [24]. Looking at those receiving triamcinolone (n=37) and dexamethasone (n=41), this study found a greater percentage of PS subjects achieved ≥50% pain relief at 2 weeks than those receiving NPS (43.2 vs 31.7%); however, this did not reach statistical significance and this difference disappeared by the 3-month and 6-month follow-up. There was, however, a statistically significant difference in the number of injections received, with 17.1% of the dexamethasone group receiving three injections vs only 2.7% of the triamcinolone group [24]. Table 2 shows a summary of all the available studies comparing the efficacy of PS and NPS.
Table 2: Trials comparing efficacy of particulate and non-particulate steroids.
Note: RCT = Randomized control trial
DB = Double blind
SB = Single blind
PO = Prospective observational
R = Retrospective
ND = Non-depot
NSD = No significant difference
SD = Significant difference
Discussion
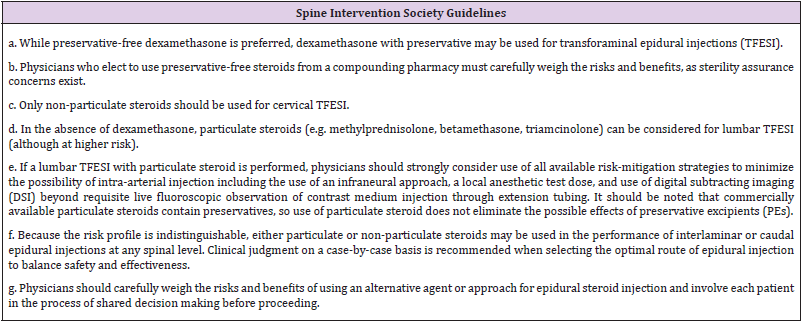
Intrinsically, there are risks and complications associated with any procedure. However, the focus of this article is to determine if there is added risk dependent on the type of steroid medication utilized in TFESI. Specifically, there is the generalized potential for air emboli, vasospasm and dissections, though these are very rare. The incidence of particulate emboli is rare but devastating when it occurs. There are numerous reports of PS-related emboli resulting in complications from paralysis to stroke or death. Catastrophic complications associated with NPS have not been reported. This catastrophic neurological risk associated with PS comes with the potential for a slight non-statistically significant pain reduction in the short term. Most studies that favor PS only followed patients for 1 month from injection. Studies that followed for a longer duration found that the difference between PS and NPS VAS scores disappeared. Bensler, et al. [22] showed a significant difference in favor of particulates, but the dosing used was not comparable given that 40mg triamcinolone was compared to 4mg dexamethasone (rough equivalent of 20mg triamcinolone). Given the body of evidence indicating increased risk and lack of compelling evidence of superior efficacy with PS, combined with the absence of any reported devastating complications attributed to NPS, it seems logical to advocate for the use of NPS for transforaminal epidural steroid injections. This is reiterated by the SIS guidelines posted in 2019 advising the use of NPS over PS whenever possible and directing physicians to advise patients of the increased risk with PS (Table 3) [25-31].
Conclusion
Though there is a strong preference among interventional pain physicians to utilize PS for TFESI, evidence strongly indicates that catastrophic complications, though rare, are exclusively associated with PS with no such reports with NPS. Furthermore, there is no compelling evidence of superior efficacy of PS over NPS other than minor, non-statistically significant early differences in VAS score that disappear with longer follow up periods. With the addition of the 2019 SIS Position Statement regarding the use of NPS for TFESI, it will be a growing challenge to justify the use of PS for TFESI given the increased risk. A shift to NPS for TFESI eliminates the likelihood of catastrophic neurological outcomes and is in line with the growing body of evidence and professional society guidelines. While position statements are non-binding, it is certainly possible that these types of documents may be relied upon for medicolegal purposes, thus creating the potential for liability for non-adherence.



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.