Effect of Mirror Therapy on Sitting Balance in Patients with Pusher Syndrome: A Case Study
Introduction
Stroke (Stroke), also known as “stroke” and “cerebrovascular accident”, is an acute cerebrovascular disease, which is a group of brain tissue injuries caused by sudden cerebrovascular rupture or blood failure to flow into the brain, including ischemic and hemorrhagic stroke. Relevant epidemiological experts have studied the relevant situation of stroke in China. The study shows that there are 11 million stroke patients in China, and about 2.4 million new cases every year, of which about 1.1 million people died, and the surviving patients have varying degrees of dysfunction [1]. In addition, other researchers found that the disability rate of stroke exceeded 70%, and the severe disability reached 40% [2], Between 10-16% of stroke patients have tilt syndrome [3](Pusher Syndrome, PS. PS is a particular postural control disorder that occurs after stroke [4], It shows that the patient actively pushes the healthy body away using the healthy arm or leg, turning the center of gravity backwards to the hemiplegic side, and resisting any attempt to passively correct his tilt position. This special clinical manifestation of PS seriously affects the balance of patients under different positions, such as sitting, standing and walking. Balance is directly related to whether they can live independently, social needs, and family care. If the special clinical performance of PS is not correctly understood, the patients will be identified as “not hard work” and “no cooperation”, which will greatly reduce the rehabilitation efficiency, delay the rehabilitation time, increase the medical expenses, and reduce the quality of life of the patients.
At present, the mainstream treatment methods of PS are mainly posture control, trunk muscle reinforcement training, visual feedback training, and attention training. Postural control training can strengthen the trunk tension of PS patients, adjust the coordination between the health and affected torso, promote the upright posture of the muscles and both sides; the attention training is to improve the patient to improve the balance ability [5]; Visual feedback training is an intervention with the motion output and motion feedback process of the balance control system. It is a training way to give intuitive feedback on the training actions through vision. In this study, mirror therapy, MT) is proposed to use the principle of plane mirror imaging to copy the healthy side activity to the affected side limb, induce the affected side activity to eliminate abnormal sensory or recovery function, and provide ideas for the treatment of PS patients. Pusher syndrome (PS) is a special posture control disorder occurring after stroke, where the patient uses a healthy arm or leg to actively push away the home body, reverse the center of gravity to the hemiplegic side, and resist any attempt to passively correct his tilt posture. At present, the domestic treatment plan for PS patients mainly include three categories: posture control, trunk muscle intensive training and visual feedback training. Many studies proposed in this paper have shown that mirror therapy can improve the exercise ability and balance ability of the lower limbs of stroke patients. The study of the balance ability of the particular population of —— PS patients in stroke patients is also proposed. The purpose of this case analysis is to analyze the effect of mirror treatment on lower limb motility and balance, especially sitting balance of such stroke patients, provide more rehabilitation methods for PS patients, and provide more theoretical basis for the treatment effect of mirror therapy for PS patients.
Data and Methods
Subject Investigated
The study object was a hemorrhagic stroke patient from the Rehabilitation Department of Sichuan Provincial People’s Hospital, ① This patient with tilt syndrome met the diagnostic criteria for stroke passed at the Fourth National Cerebral Vascular Conference in 1995, And this patient with PS was diagnosed with unilateral hemorrhagic stroke after cranial CT or MRI; ② This patient had his first onset, The time of illness is within 3 months; The ③ contralateral tilt scale (scale for contraversive pushing, SCP) score more than 0 points in sitting; ④ lower extremity muscle tone modified Ashworth grade 2 Brunstrom stage in stage I-; ⑤ patients were able to understand the instructions for treatment, And cooperate with the treatment of ⑥ patients and their families agreed to conduct the treatment.(2) Excluding standard ① instability, such as severe heart disease or seizures, failure of ② to maintain balance for reasons other than PS, obvious cognitive impairment of ③, and impaired ④ vision. Law X, male, was born in May 1957.Because the left limb weakness accompanied by speech is not conducive to our hospital for treatment on November 4,2019, after evaluation, we were admitted to hospital after meeting the admission criteria of our department.
Patient family describe the patient on November 1,2019 around 12 in the field, sudden left limb numbness, insophical, incontinence, in the local hospital examination, head CT shows the right basal section, internal capsule posterior limb bleeding to different degrees, the PS patient bleeding reached 25ml, the local hospital immediately to the patient “ cranial valve decompression. After the operation, the patient was treated in the local intensive care unit for three days. After three days of treatment, the patient gradually became conscious, and the patient still had dysfunction based on the left limb. In order to seek further recovery of function, he was treated in Sichuan Provincial People’s Hospital. On admission, sane, poor understanding, poor speech, the wheelchair pushed into the ward. Muscle tone (determined by the modified Ashworth rating table) left upper limb grade I+, lower limb grade I; muscle strength (MMT grade) left upper limb grade 2, left lower limb grade 2. No abnormal passive activity in the joint, as assessed by the Brunnstrom level 6 evaluation method, the left upper-handleft lower limbs were grade, grade I and grade, respectively. The second and triceps reflex, radialis reflex and Achilles’ tendon reflex are normal reflex level 2+, and the knee reflex is level 3 +, and the shallow and deep feeling is decreased to varying degrees.
Methods for P S Patient Intervention Studies
Routine Treatment and Rehabilitation: The patient was treated with conventional hemorrhagic stroke, and patients with tilt syndrome required clinical medical medication and routine rehabilitation. Routine rehabilitation treatment mainly includes the following contents of the ① good limb position placement, During the first rehabilitation training of patients with tilt syndrome, The therapist taught the family the various limbs, Let the family members maintain the correct position during the absent training time, To ensure that the joints on the left side of the PS patient are relatively stable, Prevent the dislocation of its left joint, The unique typical spasticity pattern of stroke patients, which is the improvement and maintenance of ② joint activity of upper limb flexor and lower limb extensor muscle, The protocol was formulated based on the relevant training and evaluation of patients with tilt syndrome, Motor choice of passive activity or active power movement, To improve and maintain each joint activity in PS patients. The control of ③ muscle tone, mainly using the passive extension method, to control the patient muscle tone. Generally, passive stretching is carried out before joint activity. Each joint is trained 3-5 times at a time, and each stretching for 30s.For ④ weight-bearing training, the patient’s weight-bearing training was only carried out in the second two weeks.
The patient’s upper limbs were placed on a 40cm high plane, the buttocks were gradually lifted off the bed to gradually train the lower limbs, and the patient with PS was supplemented with center of gravity transfer during weight-bearing training. ⑤ balanced training, mainly sitting balanced training. Let the patient sit on a bench and other bench, the therapist stood in front of the PS patient, the therapist put one hand on the left shoulder blade of the PS patient to prevent the posterior contraction of the shoulder blade, the other hand on the back of the PS patient’s waist, to achieve the purpose of the patient’s spine straighten and bend the hip. Rehabilitation training such as ⑥ body position transfer. At the same time, for the case of the PS patients, stimulate the PS patient side trunk lateral flexion activity: because one of the characteristics of PS side tension is too low and disease, patients side lack of activity, so in order to lengthen the PS patients paralysis related muscle group, improve the PS side trunk shortening, to achieve the purpose of the patients to the side transfer center. And in order to restore the head to the normal position, the guiding training is used, in the sitting of the patient, inclined to side, the patient with the side hand to take the direction of the side items. The training lasts once daily, 30min, rehabilitation on Monday ——, Saturday and Sunday rest for four weeks.
Mirror Treatment and Rehabilitation: A quiet room was selected for treatment, with a glass mirror of about 85* 189 and a physiotherapy bed placed next to the mirror. The patient was sitting in the treatment bed. The mirror was placed directly in front of the patient and in the median sagittal surface of the patient, the healthy upper and lower limb on the mirror side, the affected upper and lower limb on the non-mirror side, and the reflex image of the upper and lower limb movement on the mirror side during training. Before the therapist conducts rehabilitation training on the patient with PS, the therapist first informed the patient and the purpose and methods of the training and relevant precautions during the training process. To ensure that the PS patient should fully understand and actively cooperate with the mirror treatment and rehabilitation, and then demonstrate the patient with the action, so that the patients with tilt syndrome can fully understand the essence of each action. The therapist trained the patient with the same instructions as on both lower limbs of PS patients. In the process of treatment, the therapist should ensure that the patient try to complete the movement of the left lower limb, if the left limb cannot complete, the therapist should be given tilt syndrome patients to a certain degree of assistance, ensure that the PS patients to complete the movement of the lower limbs, at the same time told PS patients in training the lower limb movement as the movement of the lower limb. During training, PS patients need to complete the five movements: flexion extension of hip, adductor extension, flexion extension of knee, dorsal flexion of ankle, and ankle valgus. Each action was repeated 10 times for one group, each with a 30s rest for 30min each, and five training sessions per week for 4 weeks.
Evaluation Indicators
The evaluation by the same five years in neurorehabilitation work of the patient, the PS patient system rehabilitation treatment the day and the day after the end of the evaluation of the therapist, and the evaluation of the patient therapist is unaware of the PS patient system rehabilitation plan
Exercise Ability
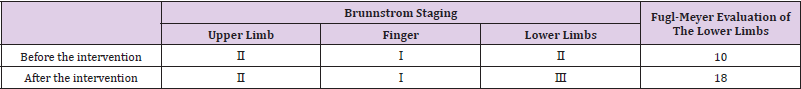
Brunnstrom Staging: Brunnstrom Level 6 evaluation method [6] It is simple and easy to perform, and it is often applied to the general clinical examination of stroke patients. This evaluation method includes the evaluation of the upper limbs, fingers and lower limbs, respectively. In this study, the motor ability of the lower extremities of PS patients is mainly evaluated.
Fugl-Meyer Assessment of Lower Limbs: Fugl-Meyer Assessment Method (Fugl-Meyer assesment, FMA) [7] Based on the Brunnstrom level 6 evaluation method, a quantitative evaluation method for stroke patients is mainly designed, specifically used for the evaluation of stroke hemiplegia. The Fugl-Meyer evaluation method includes five categories: limb movement, balance, sensation, joint activity and pain, including 17 small items in lower limb evaluation, and each item is divided into three grades, 0,1,2 and 17 items. The higher the FMA score, the better the lower limbs.
The Severity of the PS
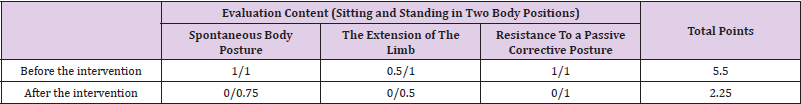
The SCP Scale: The scale for contraversive pushing (SCP) scale first had Karnath, et al. [8].The design proposes that the diagnosis and severity evaluation of PS after stroke are widely used in the evaluation of ① spontaneous body posture (0/0.25/0.75/1 score), ② healthy limb extension / abduction degree (0/0.5/1 score), and ③ resistance to passive correction posture (0 / 1 score).The above three components were assessed in sitting and standing positions, with a maximum score of 2 points for each. The patient was considered to have inclination behavior if they scored 1 for the three components.
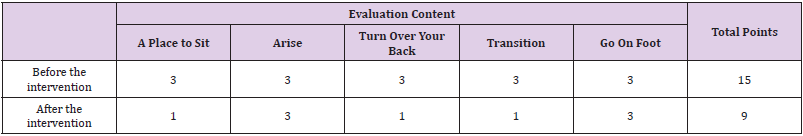
The B L S Scale: Five evaluation items of turnaround, sitting, station position, transfer, and walking constitute the Burke Roll Scale (Burke Lateropulsion Scale, BLS) [9]. The therapist described the symptom severity by assessing the magnitude of resistance that patients present when maintaining or changing body position in these 5 states. The presence of tilt behavior is determined by the results assessed at sitting and position. If the evaluation results indicate a total score of 2, the patient has a tilt behavior. Each score range is 0 to 3 points, 0 is divided into no resistance, 1 is divided into resistance and the patient midline by 5 degrees according to the vertical difference, 2 is divided into resistance began and the angle between the patient’s middle line and the vertical line varied by 10 degrees, 3 is divided into the angle of the midline and the ground vertical line formed by more than 10 degrees. The scores of turnings, metastasis and walking were based on the intensity of pushing felt by the examiner, 0 as no resistance, 1 as mild, 2 as severe, and the three positions were used to evaluate the severity of patients’ tilt behavior.
Balance Function Assessment
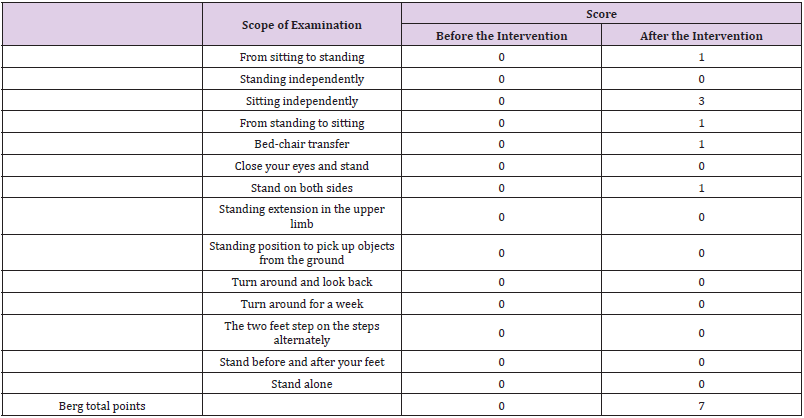
The Berg Balance Scale: The Berg Balance Scale (Berg balance scale, BBS) was used in this study [10] Patients with PS were evaluated.In 1989, the scale was proposed by Katherine Berg and was generally used to assess balance function in stroke patients and children with cerebral palsy. This scale consists of 14 items, including standing up, sitting down, independent standing, eye closed standing, upper arm extension, each rated 0-4 and 14 items total 56 points, the higher the score, the better the patient balance function.
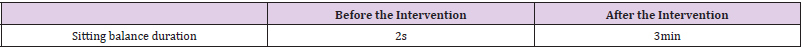
Sit and Position Balance Time: Sitting balance time directly effective should the patient sitting balance ability improved. The patient measures the sitting balance time for the sitting position. The patient sits on the stool, his feet flat on the ground, the back leaves the back of the chair, and his hands naturally on the knee. The therapist used the stopwatch to observe the duration of the patient’s sitting balance.
Results
Kinetism
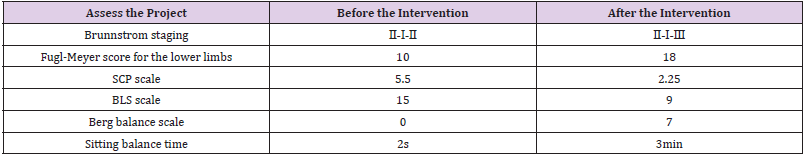
As shown in Tables 1-3, the exercise ability can be seen before and after routine rehabilitation training and mirror treatment. From the perspective of Brunnstrom stage, the upper limbs and fingers are still stuck in stage and stage I, respectively, and the affected side upper limbs of PS patients showed the appearance of spasm, indicating the appearance of the joint response in the PS patient; the fingers showed slow muscle tension without any movement. Results from the Brunnstrom staging indicated no significant changes in the upper limbs and fingers. However, Brunnstrom stage and Fugl-Meyer results showed that the patient’s lower limbs capacity was improved, and the lower limbs entered from the joint reaction period into the stage, causing common movement and small flexion of the hip and knee at sitting and standing.
The Severity of the P S
The SCP Scale: The patient had a significant decrease in the SCP scale score after routine rehabilitation training and mirror treatment, especially with the evaluation score of 0 under sitting, indicating a significant improvement in the severity of PS after treatment.
The BLS Scale: The BLS scale score consistent with the results in Tables 4-6 were significantly reduced following routine rehabilitation training and mirror treatment, indicating a significant improvement in the severity of PS after treatment. In sitting, the patient improved from about 50 degrees to vertical to about 5 degrees vertical; Although the score of the patient did not change before and after the intervention, the therapist observed that the resistance began to about 20 degrees from about 60 degrees; the resistance during supine turning and metastasis also improved from severe to mild resistance.
Balance
The Berg Balance Scale: The preintervention Patient Berg Balance Scale score was zero and 7 points after routine rehabilitation and mirror treatment. After systematic rehabilitation training, the patient is able to complete the transfer from sit to station and from station to sitting with less assistance by the therapist; the patient can complete the bed chair transfer with one person; sit in a back chair, put the feet flat on the ground with the same width as the back of the patient, and cross the bilateral upper limbs on the chest. The patient was able to sit under custody for two minutes; while holding his feet together for 15s with the help of the therapist for 15s.
Sit and Position Balance Time: The patient measures the sitting balance time for sitting. The patient sits on a stool, his feet flat on the ground, his back leaves the back of the chair, and his hands naturally on the knee. Before the intervention, the patient could not maintain the sitting position. The patient had slightly tilted the back, the body shifted to the left during the sitting position and did not adjust his body position to the right by following the therapist’s instructions. After training, the patient was able to maintain the balance under the custody of the therapist for 3min, and after 3min to follow the instructions of the therapist to adjust his position accordingly, and maintain the sitting balance for 5min-10min.
Results Before and After the Intervention: The results showed that patients had improved exercise and balance ability and improved PS severity after routine rehabilitation training and mirror treatment.
Discussion
The results of this study indicate a zero patient Berg balance scale score before the intervention and 7 points after routine rehabilitation and mirror treatment. Among them, the score increased from 0 to 7, combined with the results of the sitting balance duration after the intervention showed that the sitting balance improved effectively after the mirror treatment. And Gao Xiaoyan [11] Puseer syndrome also received intensive balance function in patients with acute stage stroke, and after research, she emphasized the importance of the recovery of seated balance for the rehabilitation of PS patients. The main manifestations of Pusher syndrome are that the center of gravity is biased to the body imbalance state on the paralyzed side, so it is particularly important to strengthen the patient sitting balance training. Only by improving the sitting balance is it possible to stand and walk and improve their other dynamic balance. In the study of increasing mirror treatment on conventional rehabilitation treatment in patients with early stroke, it showed that the improvement of upper limb function was significantly higher than in the control group, and in this study, superficial sensation and unilateral neglect in the experimental group by Dohle, et al. [12]; The results of Hou Hong and other scholars show that stroke patients’ exercise ability, upper limbs can be significantly improved after mirror therapy and exercise training [13].
According to the above and other studies, mirror therapy plays a significant role in improving their upper limb motor function, daily life ability and attention, but there are few studies on their lower limb motor function in stroke patients, and few studies on special groups of PS patients with stroke. And due to the limited mirror device, for the lower limb movement function mirror therapy specific procedures, action, intensity, frequency, length of time not standardized description, directly affect the application of lower limb movement function, is also further study the application of the therapy in PS patients recovery of lower limb movement function one of the important reasons. The case study using the traditional plane mirror between patients’ legs, healthy lower limbs on the mirror side, affected lower limbs in the mirror side, told the patient in the process of treatment in the mirror of the limb movement and imagine the movement, while the patient, under the instructions of the therapist, active or passive affected lower limbs with the same movement as healthy lower limbs. The evaluation results show that the lower limb movement ability and balance ability have been significantly improved. According to Xu Jianyang’s sEMG study to correct sitting balance in patients with stroke tilt syndrome [14], After analysis and discussion of the tested data, the muscle with the most associated with tilt syndrome is the gastrocnemius, which is speculated that the breaking of the common motion pattern of lower limbs in different joints such as hip, knee, and ankle and the emergence of active motion have promoted the gastrocnemius activation.
Moreover, the enhanced stability of the trunk core muscle group benefited from the training of PS patients to exercise both lower limb movements in the sitting position. In addition, the improved stability of the core muscle group promotes the improvement of sitting balance, and the movement of bilateral lower limbs stimulates the active lower limb tendons and proprioceptors in the skin and improves the impaired balance function in patients with tilt syndrome. In addition, while PS patients see intact contralateral limb mirror imaging, a large number of mirror neurons derived from the premotor cortex, lower anterior central gyrus, Broca region, subparietal leaflet mouth side, posterior inferior frontal gyrus, amygdala, insula, and prefrontal cortex are activated [15], Its corresponding cortical neurons are simultaneously activated at the moment when a large number of mirror neurons are also activated. The above view has been demonstrated by EEG, which shows the firing form of the mirror neurons as the same electrical activity of the brain region when the mirror neurons actually complete the corresponding action. Speculation tilt syndrome patients in mirror treatment, bilateral lower limbs in the specified related movements, PS patients in mirror PS patients in bilateral lower limb patients’ healthy lower limbs imaging, PS patients because of visual illusion, the normal activity of the lower limb exercise training as the movement of the affected lower limbs.
Through this principle, visual feedback of motor function recovery in the affected side lower limbs in patients with PS is provided to patients undergoing training. At the same time, the healthy hemisphere of PS patients reduces the inhibitory effect of the focal cerebral hemisphere, the excitability and intercortex primary motor cortex, make the interhemisphere excitationinhibitory balance, and then promote the affected motor pathway activation, making PS patients restore some motor function of the affected lower limbs [16], The improved lower limb motility in PS patients also improved the balance function of PS patients. Besides, the lower limbs of stroke patients were mirror-treated by Sutbeyaz et al. After performing 4 weeks of rehabilitation training, The followup results at 6 months indicated a significant improvement in the lower limb motor function, This result was based on Brunnstrom VI evaluation and functional evaluation of lower limbs (functional independence measure, FMA) RiverMead Visual Traits Assessment (rivermead visual gait assessment, RVGA) score on a statistically significant basis [17]. It was proposed in Mohan et al that after mirror acute stroke treatment, it showed a significant improvement in lower limb motor function in these treated patients [18]. In the study, Cui Wei trained 32 ischemic stroke patients on mirror therapy. Her results showed that the lower limb motor function of the 32 participating stroke patients were significantly improved and their overall motor function after mirror treatment [19].
Other related studies on the impact of mirror therapy in stroke patients combined with other treatment modalities on lower limb function. Some researchers have treated the affected side ankle joint of some stroke patients, who have performed functional electrical stimulation in the affected side limb during the mirror treatment. The evaluation results show that the increased ankle dorsal flexion activity, FMA score and 10m walking experimental score of these stroke patients have been significantly improved. Ji and colleagues studied the impact of lower limb mirror therapy combined with virtual therapy on stroke patients, and finally they proposed that mirror therapy can be used to improve lower limb motility in stroke patients [20]. In the study, Hyun-Gyup conducted stroke patients with task-oriented training, and observed mirror imaging in Hyun- Gyup et al. The results showed improved ability to adjust autonomic posture, hence improved balance function of these trained stroke patients [21]. In conclusion, mirror therapy has been demonstrated by this experiment and research on the recovery of lower limb motor function and balance function in stroke hemiplegia patients.
The results of this study show that the lower limb motor function and balance function of patients with tilt syndrome have been improved to some extent, indicating the good and positive effect of MT in this special group of PS patients. But the study was only one subject, affected by smaller doses. Moreover, there is no unified standard for the application of mirror treatment to stroke PS patients, which may also have some impact on the experimental results. The future utility of mirror treatment for the lower limb motor function and balance function of PS patients and the direction of PS patients and objectives of our standardization.
Conclusion
Mirror therapy combined with conventional rehabilitation treatment has a promoting recovery effect on the motor function, balance function, and metastatic ability of this PS patient, while the severity of PS in this patient is significantly reduced. In summary, this case study suggests that MT may have a positive effect on lower limb motility and balance ability in PS patients, and can be used as an additional treatment for PS patients.



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.