Frequency of Blood Glucose Monitoring in Relation to Glycemic Control in Patients with Type-2 Diabetes
Introduction
Diabetes is among the principal sources of morbidity and mortality around the World. Diabetes prevalence has been increased from 108 million cases in 1980 to 422 million cases of diabetes in 2014, and this trend of increasing burden has been speculated to raise from 425 to 629 million diabetic people from 2017 to 2045 [1]. Diabetes is among the major health problems facing the human population around the world today. It also poses economic problem because it is estimated that 10% of National Health Service (NHS) expenditure is spent on diabetes which is equal to £1 million per hour. Presently, 2.3 million people have been reported with diabetes and above 500,000 people with type-2 diabetes are not aware of their diabetic status. It is expected that more than 4 million people will have diabetic till 2025 and probably a large number those will have type-2 diabetes, leading to an increase in aged, overweight and obese individuals. It is alarming that growing unhealthy lifestyle has been a key reason of type-2 diabetes, once observed only in the over-40s, being diagnosed in a increasing number of younger people and even children [2]. Diabetes is manifested when blood glucose concentration reaches the higher level than normal blood sugar level. Blood sugar is a main source of energy found in foods which we eat. Insulin is hormone which is made by the pancreas which facilitates glucose from food get into cells for its use as energy. At times body doesn’t make sufficient or any insulin or doesn’t use insulin properly, then glucose remains unused in blood and doesn’t enter cells.
Three types of diabetes are commonly found as type-1, type-2 and gestational diabetes. In type-1 diabetes the body doesn’t make insulin and the patient immune system attacks and damages those cells in pancreas which are responsible for making insulin. Type-1 diabetes is typically detected in children and young adults, though it can appear in every age. Individuals in type-1 diabetes need to take insulin every day for his/her survival. In type-2 diabetes, which is most common type of diabetes the body doesn’t produce or use insulin properly. Type-2 diabetes can start at any age, even during childhood. However, this type of diabetes takes place mostly in middle-aged and older people. Gestational diabetes is caused in certain women when they are pregnant. Most of the times, this form of diabetes goes away after the birth of baby. There are some other less common types of diabetes including monogenic diabetes, which is an inherited form of diabetes, and type of diabetes associated with cystic fibrosis [3]. Type-2 diabetes has a number of causes but most important are known as genetics and lifestyle, but the combination of both factors can create insulin resistance, when body doesn’t use insulin as it should. Insulin resistance mostly causes type-2 diabetes. Genes do play important role in type-2 diabetes, but lifestyle also play important role. Lifestyle choices that affect the development of type-2 diabetes includes lack of exercise, unhealthy meal planning choices, overweight or obesity [4]. Some risk factors of diabetes include being overweight or obese, hypertension (high blood pressure), and low level of “good” cholesterol (HDL), elevated level of triglycerides in blood, sedentary lifestyle and family history of diabetes. Symptoms of diabetes include increase urination, excessive thirst, weight loss or gain, hunger, fatigue, skin problem, blurred vision, nausea, vomiting etc. Diabetes can cause microvascular (damaged to small vessels) and macrovascular (damaged to large vessels) diseases [5].
Self-monitoring of blood glucose (SMBG) refers to check blood glucose of diabetic patient at home. SMBG is an important modern therapy of diabetic patients. It is used to attain a specific level of glycemic control and to avoid hypoglycemia. The aim of SMBG is to gather detailed information about blood glucose concentration at various times. SMBG can be used to help in the fixing of a therapeutic regimen in response to blood glucose values and to assist individuals in adjusting their dietary intake, physical activity, and insulin dosages to improve glycemic control on a daily basis [6]. SMBG can be measured by strips or by glucometer before meal (fasting blood sugar, FBS) or anytime (random plasma sugar, RBS). Hba1c refers to glycated hemoglobin is actually the protein in the RBCs carrying oxygen all over the body joins with glucose and become glycated. Through measuring hba1c we are able to get the whole status of average blood glucose level over a period of weeks/ months. The normal Hba1c is below 42mmol/mol or below 6.0%. Prediabetics have 42-47mmol/mol or 6.0%-6.4% and diabetic have 48mmol/mol or over and/or 6.5% or over. There is a difference between hba1c and blood glucose level. In hba1c we know about the how high sugar level has been over a period of time, it provides a longer-term trend. While blood glucose, is the concentration of glucose in blood at a single point in time. It is measured as FBS and RBS [7]. Study reported that that SMBG concentration is linked with improved glycaemic control in patients and rise in rate of SMBG with growing HbA1c value was proportional to the higher ratio of insulin- treated patients in higher HbA1c categories [8,9]. Also, the better quality of metabolic control demonstrating self-monitoring of blood glucose improved glycemic control in the majority of non– insulin-treated and also insulin treated type-2 diabetic patients [10-12]. Studies have reported that substantial numbers of diabetic patients have poor glycaemic control and older age, duration of diabetes, poor dietary habits, rural lifestyle, poor medication and low education are the eliciting elements of poor glycaemic control [13-15]. Inadequate glycaemic control prevailed in the majority of aged Pakistani diabetic subjects. SMBG levels have been reported to be associated with clinically and statistically improved glycaemic control irrespective of diabetes types or therapies. Eliciting factors of poor glycaemic control and increase awareness on the significance of SMBG and strongly promote this practice among diabetic patients should be taken seriously by the healthcare authorities in targeting multidimensional interventions to accomplish good glycaemic control [8,9]. In the year 2017, about 6.9% (7,474,000 individuals) of the Pakistani population were suffering from diabetes and the country was on 10th position (projected to be on 8th position in 2045) among high burden diabetes countries all over the world [1]. Numerous studies on SMBG have been done in different countries and also in Pakistan but there is no such study conducted in Mardan district of Khyber Pakhtunkhwa province (KP) in Pakistan [8,9]. Therefore, the present study is aimed at investigating the association between blood glucose, measured as Hba1c and frequency of SMBG in diabetic patients from Mardan Pakistan [16].
Materials and Methods
Study area: This study was conducted in District Mardan of Khyber Pakhtunkhwa. Data were obtained from patients with diabetes from District Mardan. The Mardan city is on 23rd position in the list of big cities of Pakistan and the second largest city of Khyber Pakhtunkhwa with human population size of 331,837. Mardan is located in the southwest of the district at 34°12’0N 72°1’60E and at altitude of 283 metres (928 ft). An economic zone is planned as a part of the multi-billion-dollar China-Pakistan Economic Corridor (CPEC) near Rashakai. Mardan features a hot semi-arid climate. The average temperature in Mardan is 22.2°C, while the annual rainfall averages 559 mm. (https://en.wikipedia.org/wiki/Mardan).
Study Population
The data were collected from 100 diabetic patients of Mardan including male, female and children related to different age groups. These patients were suffering from type-2 diabetes. Data collection: Data were collected from the patients of diabetes diagnosed in Mardan Medical Complex, private clinics and private hospitals in District Mardan. during January 2019 to March 2019 through convenience survey. Information was obtained by structured questionnaires on diabetes therapy and blood glucose self-monitoring. All the participants were briefed about the study and then their written consent was obtained. All the subjects were subjected to interview for filling the questionnaire proforma regarding the study. Data regarding glycemic values, socio demographic and clinical characteristics of the patients were recorded. All those subjects with severe illness, having accidental physical disabilities, unable to comprehend this study, those having life threatening diseases and those suffering from cholera, dengue or malaria.
The Questionnaire Proforma Encompassed the Following Parameters
General Information: Patient name, age, gender, weight, ethnicity, type of diabetes, duration of diabetes, diabetes therapy, fasting plasma glucose, random plasma glucose, Hba1c.
Additional Information: Family history, additional disease with diabetes, allergies, hypoglycemic episodes, education, income and employment.
Study Variables: These variables included glycemic control parameters including FPG, RPG and HbA1c. Socio-demographic and clinical features, depression, cognitive status, physical status, weakness, nutritional status, pain and level of self-care were independent variables. The target value for HbA1c was <7%, FPG was 80–130 mg/dL and RPG was <180 mg/dL [17]. Subjects having HbA1c, FPG, and RPG levels above the upper threshold of the target levels were declared as having poor glycemic control.
Statistical Analysis: SPSS version 21.0 was used for statistical analyses of collected data. Descriptive statistics and bivariate correlation were applied. Mean and standard deviation were computed for quantitative variables. Qualitative variables were subjected to frequencies and percentage analyses.
Results and Discussion
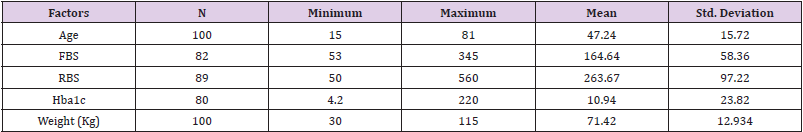
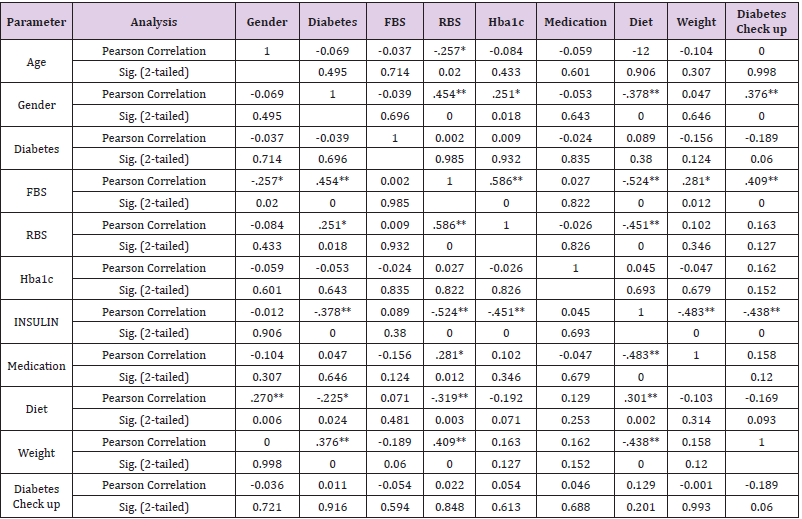
Descriptive analysis showed that age of subjects was between 15-81 years with mean ± SD as 47.2±15.7. almost equal number of subjects belonged to urban (52%) and rural (48%) areas. Most were females (60%) subjects, and 82% subjects were suffering from years. Overall, 44% of the patients used to check their diabetes less than twice a week and 22% check their diabetes once daily. Stratification for frequency and percent of patients who test their FBS and RBS was 82% and 89% among which some people couldn’t test either FBS or RBS. The recorded FBS value was 53-345mg/dl with mean ± SD of 164.6±58.4 and of RBS was 50-560mg/dl with mean ± SD of 263.7±97.2. The frequency of hba1c was 80 with recorded value of 4.20-16.90% and mean ± SD was 10.9±23.8. Most of the people (67%) used medications along with insulin from years. Maximum of the (52%) people were not following diet to control it. Majority of the patients (78%) had high blood sugar. Weight of the patients was between 30-115kg with average between 60-70kg. Most (67%) subjects were not doing regular exercise. Maximum of the patients (73%) were consuming tea 42% showed no family history of diabetes while 40% subjects had one parent affected and 18% had both parents affected. Most of the patients (98%) had other problems like vision problem, nausea, numbness etc. Sixty percent subjects were literate with majority of unemployed, and 55% were middle class (Table 1). By using bivariate correlation, we performed Pearson correlation coefficient. The values p˃0.05 and p˃0.01 show significant linear relationship. From this correlation analysis a linear relationship between age and weight was determined as well as between gender and SMBG, insulin, diet and weight. There was no correlation between SMBG and Hba1c (Table 2).
In past few decades, huge rises in diabetes prevalence have been confirmed in almost all areas of the world, with 415 million people worldwide now living with diabetes [17]. Diabetes is among the metabolic disorders characterized by elevated blood sugar levels for a long time period. Diabetes afflicts various complications like diabetic ketoacidosis, hyperosmolar hyperglycemic state, or death. Other severe complications can be cardiovascular disease, stroke, chronic kidney disease, foot ulcers, and eyes damage. (https:// en.wikipedia.org/wiki/Diabete). In 2000 the global prevalence of diabetes was estimated to be 151 million by International Diabetes Federation (IDF). In 2003 the number reached to 194 million, in 2006 the number increase to 246 million, in 2009 it reached to 285 million, in 2011 it increased to 366 million, in 2013 it reached to 382 million, in 2015 it reached to 415 million. In recent study it was estimated that in 2017 about 425 million cases of Diabetes in age group 20-79 years throughout the globe, If the age range is increased to 18-99 the estimated case of diabetes rises to 451 million, the number of diabetes cases are increased day by day and reached to 629 million people for age range 20-79 years [17].
According to a recent study in Pakistan, 11.77% prevalence of type-2 diabetes mellitus has been recorded. Males were more affected (11.20%) than females (9.19%). Likewise, this trend was reported in 3 provinces of Pakistan as well reporting 16.2%, 12.14% and 13.3% prevalence in males as compared to females as 11.70 %, 9.83% and 8.9% respectively in Sindh, Punjab and Baluchistan province respectively. While in Khyber Pakhtunkhwa (KP) Province, females (11.60%) were more affected than males (9.2%). This prevalence was higher in urban areas (14.81%) as compared to that reported from rural areas of Pakistan (10.34%) [18]. In our study we focused on the frequency of blood glucose monitoring in relation to glycemic control in patients with type- 2 Diabetes. This kind of study was first reported from Scotland by Evans et al. [10] to investigate patterns of self-monitoring of blood glucose concentration in diabetic patients and to determine whether frequency of self-monitoring is related to glycaemic control. Further studies are conducted in different countries. In Pakistan similar study has been reported from Agha Khan University Karachi by Khowaja, et al. [8], to explore the association between selfmonitoring of blood glucose (SMBG) levels and improved glycaemic control (HbA1c level) among type-2 diabetic patients.
Our study revealed that 89% subjects were suffering from type- 2 diabetes, 5% from type 1 diabetes, 1% from gestational and 5 from other types of diabetes. Out of 100 cases 40% were male and 60% were female. Stratification for frequency of normal blood glucose in patients suffering with diabetes mellitus with regards to duration of diabetes mellitus was recorded which shows that out of 100 cases 82 subjects have diabetes from years, 15 have from months and 3 subjects have diabetes from days. Overall, 52% belonged to urban areas and 48% from rural. Frequency of Hba1c was 80%. Seventy nine percent did not develop any types of allergies. The normal blood glucose in patients suffering with diabetes with regards to financial status shows that out of 100 cases 10% were of lower class (10,000-20,000), 60% were of middle class (20,000- 40,000) and 30% were from upper class (> 40,000). Frequency of control of blood glucose in patients suffering with diabetes mellitus with regards to educational status showed that 60% patients were literate, and 43% were employed. By using bivariate correlation, we performed Pearson correlation coefficient. Basically, this was performed the extent to which two variables are linearly related. The value p˃0.05 and p˃0.01 show significance. From this correlation we found that there is significance association between age and weight. There is also significance link between gender and SMBG, insulin, diet and weight. According to frequency of and time of doing SMBG, the results of the participants who did SMBG were above or below the target for glycemic control. This means that doing SMBG is not currently associated with better glycemic control. There is no liner relationship between self-monitoring blood glucose and Hba1c.
Evans et al. [10], have reported a direct relationship of haemoglobin A1c level with the number of strips collected during previous 6 months in diabetic patients. They have not found any association of HbA1c level and SMBG in diabetic patients using insulin. It may be due to the fact that SMBG is more effective in true insulin deficiency unlike the insulin resistant state. Or diabetic patients might have no aware of insulin use, more worried about the risks of hypoglycaemia, and hence less likely to act on the results of tests. Our study is similar to Harris [11] who evaluated the association of SMBG and HbA1c. They reported no such association between the frequency of SMBG and HbA1c level of those diabetic patients treated with insulin, oral agents, or diet alone. More educated, having a diabetes patient education class, and frequent visitor to physician were found frequently practicing self-monitoring. However, SMBG was not associated with higher economic status or to having health insurance. Our study was quite contradictory to the study of Khowaja and Waheed [9] because they examined that self-monitoring of blood glucose concentration is associated with improved glycaemic control, which prevents complications resulting from diabetes. Their study indicated that there was a significant association of self-monitoring of blood with glycaemic control. It was contradictory may be because their sample size was 5 times higher in number than our study samples. Davis, et al. [15] also determined, like our study that both cross-sectional and longitudinal Fremantle Diabetes Study (FDS) data revealed that Hba1C was not statistically different between SMBG users and nonusers. This study is also similar to Alzahrani, et al. [18] establishing that the results of the patients who followed SMBG were beyond the target for glycemic control which reveals that SMBG is not linked with improved glycemic control. In our study we do not support the association of SMBG to glycemic control. The results of our study reveal that SMBG is important, but it also indicates that majority of subjects were checking their blood sugar occasionally. It was also observed that participants doing SMBG, were managing their diabetes well and self-monitoring may be recommended particularly in those patients who are the most difficult to control.
It is established that education and economic status are also the possible effect modifiers for controlling the blood glucose levels. Besides regular checking of blood glucose, lifestyle reform also needed to be done in diabetic patients including diet and regular exercise. The results of this study may be handy for creating awareness of blood glucose control during diabetes ultimately reducing the morbidity level in due to diabetes [19].
Conclusion
According to the result of our study, regular self-monitoring in patients with diabetes is uncommon and the self-monitoring of blood glucose is not associated to glycemic control among type- 2 diabetes. There is a lack of knowledge about SMBG and Hba1c testing and control in public.



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.