Novel Use of GnRH agonist as Neoadjuvant Treatment for Giant Endometrial Polyps
Introduction
Endometrial polyp is one of the most common structural causes of abnormal uterine bleeding in the reproductive age group. It arises from endometrial overgrowth brought about by a hyper-estrogenic state. Polyps are usually around 2cm in size, and those greater than 4cm are labeled as giant polyps. The cases presented are women in the reproductive age group with fertility problems, having endometrial polyps as large as 10cm occupying the whole uterine cavity, even prolapsing out of the endocervical canal. Conservative management was recommended but due to their size, immediate hysteroscopic removal may not be attainable due to expected difficulty in distending the uterine cavity and possible morbidities like fluid overload and uterine perforation. Although with limited studies, GnRH agonists have been proposed as a neoadjuvant treatment prior to hysteroscopic removal of giant polyps. Given the same mechanism applied with GnRH agonist’s use with myomas, it induces a hypoestrogenic environment at the same time decreasing the vascularity of the endometrial lining that will help significantly decrease the size of the giant polyps, making hysteroscopic removal feasible
Case Report
Case 1
This is a case of Abnormal Uterine Bleeding (AUB) in a 29-yearold, single, nulligravid from Laguna. The patient has unremarkable past medical and family history. She is living in with her 3-year partner and is desirous of pregnancy. Ever since menarche, patient has been experiencing heavy menstrual bleeding soaking 2-3 baby diapers per day, lasting 7-14 days, with no associated symptoms. She was hospitalized at the age of 16 for blood transfusion due to chronic blood loss brought about by heavy menstrual bleeding. Blood dyscrasia was ruled out. At the age of 20, she consulted a government hospital still for persistent heavy menstrual bleeding now associated with dyspareunia and post-coital vaginal bleeding. She was assessed with a cervical mass probably polyp and underwent fractional curettage and polypectomy, which on biopsy revealed polyp. Patient continue to have occasional heavy menstrual bleeding however few months prior to consult in our institution, she had continuous profuse vaginal bleeding, this time associated with an enlarging abdomino-pelvic mass. She was assessed with cervical cancer due to a finding of irregularly shaped cervical mass. A cervical punch biopsy was done which only revealed granulation tissue. She was then referred to our institution for further work up and management.
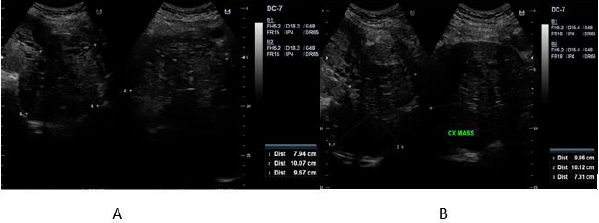
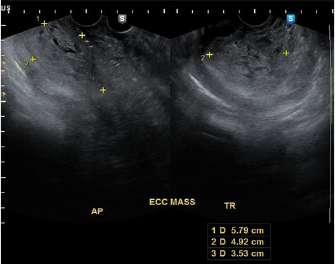
When we first saw the patient, she was pale but with stable vital signs. Speculum examination revealed a polypoid fleshy mass occupying the upper half of the vaginal canal. On internal examination, patient had a polypoid fleshy mass measuring 8cm x 10cm x 10cm occupying the upper vaginal canal and the cervix was difficult to palpate. The corpus was enlarged to 18-20 weeks size. She was initially diagnosed as a case of to consider cervical cancer and was admitted for blood transfusion and work up. Cervical punch biopsy was repeated and it revealed necrotic and hemorrhagic polypoid lesion. Transvaginal ultrasound done noted an aggregate of polyps at the cervix that arise from the endometrial cavity with attachment at the fundus. Impression was endometrial mass, to consider endometrial pathology with extension to less than 50% of the myometrium, endocervical canal, and lower third of vagina (See Appendix 1, Figure 1). Current working diagnosis was changed to AUB secondary to endometrial mass probably endometrial polyp. Patient was referred to our section for possible hysteroscopic polypectomy. But due to the size of the mass and expected technical difficulty for hysteroscopic removal, we advised pre-treatment with Gonadotropin-Releasing Hormone (GnRH) agonist to be given for 3 to 6 doses every 28 days prior to surgery.
Apendix 1 Figure 1: Endometrial mass and prolapsing cervical mass arising from the endometrium prior to GnRH agonist.
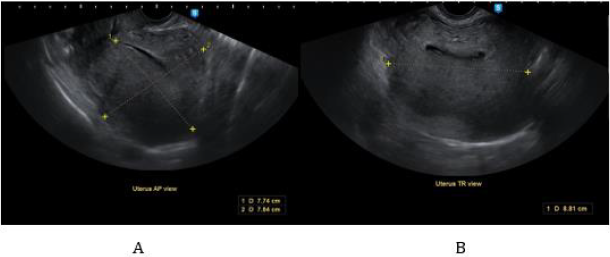
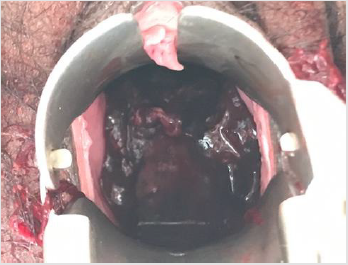
After three doses of GnRH, repeat internal examination showed that the polypoid mass within the vaginal canal disintegrated and was easily removed from its attachment. Patient noted minimal vaginal bleeding with passage of meat like material, probably fragments of the polyp. The corpus size also decreased to 14 to 16 weeks size, from the initial 18-20 weeks size. Additional 3 doses of GnRH agonist were suggested to further decrease the size of the mass and make the hysteroscopy easier. After 6 doses of GnRH agonists with a corpus size of 10-12 weeks, the patient then underwent hysteroscopic polypectomy. Intraoperatively, the polypoid mass was soft and hemorrhagic, but was not friable and non-necrotic, with an aggregate diameter of 17 cm (See Appendix 1, Figures 2 & 3). Cut section revealed multiple cystic spaces all throughout the mass. Final biopsy report showed mixed endocervical-endometrial polyp. Three months post-surgery, there was no recurrence of heavy menstrual bleeding and repeat ultrasound revealed normal uterus with thin endometrium (See Appendix 1, Figure 4). Currently, the patient is already 1 year post op with no recurrence of the heavy menstrual bleeding and is currently for infertility management.
Apendix 1 Figure 2: Endometrial mass and prolapsing cervical mass arising from the endometrium prior to GnRH agonist.
Apendix 1 Figure 3: Endometrial mass and prolapsing cervical mass arising from the endometrium prior to GnRH agonist.
Case 2
This is another case of AUB in a 30-year-old, Gravida 2 Para 0 (0020), married, from Mindoro. She has no co-morbids and had 2 previous spontaneous abortions at 12 weeks AOG. She is currently living with her husband of 10 years and is desirous of a successful pregnancy. Four years prior to consult in our institution, patient experienced heavy menstrual bleeding for 7 days, soaking 3 baby diapers per day with blood clots. She was assessed with AUB secondary to thickened endometrium and was admitted for blood transfusion. After 2 years, patient again had recurrence of heavy menstrual bleeding, this time associated with abdominal enlargement. Ultrasound was done and showed myoma uteri. She was again transfused with blood products and advised hysterectomy but patient refused due to financial constraints and desire of future fertility. 3 months prior to consult in our institution, patient again experienced continuous vaginal bleeding and pain with pallor and fatigue. She was rushed again to the local hospital and on assessment, there was a polypoid mass occupying the vaginal canal and was sampled for biopsy. The histopathology result revealed atypical polypoid adenomyoma so the patient was referred to our institution.
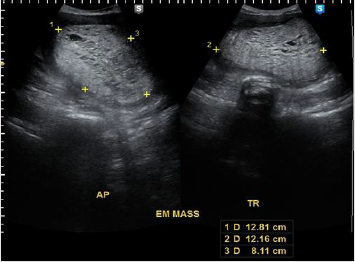
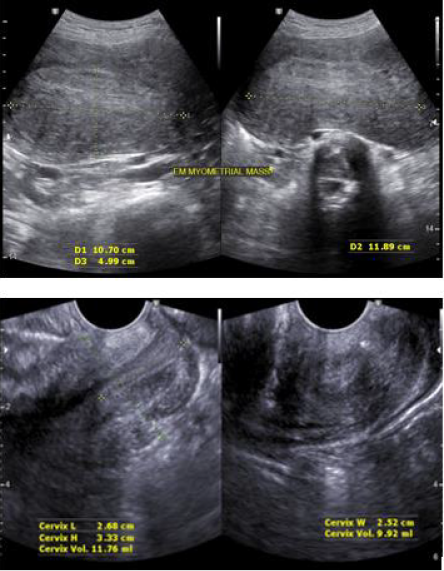
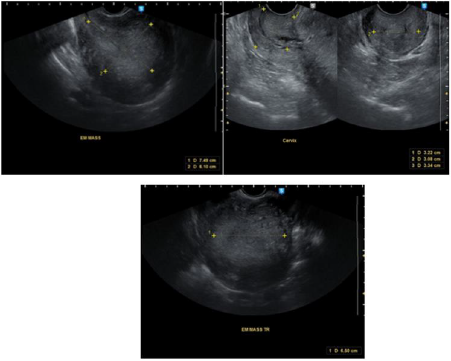
On our initial examination, the patient was pale but with stable vital signs. Pelvic examination revealed a hemorrhagic polypoid fleshy mass occupying the whole vaginal canal that easily bleeds in manipulation measuring 6cm x 6cm (See Appendix 2, Figure 1). The cervix was difficult to assess and the corpus was enlarged to 20-22 weeks size. Rectovaginal examination was unremarkable. Transvaginal ultrasound was done which showed an echogenic mass within the endometrial, endocervical and vaginal canal measuring 12.8 x 12.2 x 8.1 cm with multiple irregular cystic spaces, invading >50% of the posterior myometrium (See Appendix 2, Figure 2). The impression was endocervical and endometrial masses consider atypical polyp with >50% myometrial invasion. Repeat biopsy of the prolapsed endometrial mass was done which revealed endometrial polyp. Patient was also referred to our section for possible hysteroscopic polypectomy. But again, due to the size of the mass and expected technical difficulty for hysteroscopic removal, pre-treatment with GnRH agonist prior to surgery was advised. After 2 doses of GnRH, there was significant improvement of patient’s symptoms, but with minimal vaginal bleeding, and passage of meat-like materials. On internal examination, the prolapsing endometrial mass decreased to 2x2cm (See Appendix 2, Figure 3) and the corpus size decreased to 16-18 weeks from the initial 20-22 weeks size. Repeat ultrasound also noted a decrease in the size of the endometrial mass to 10.7 x 11.8 x 5.0 cm (See Appendix 2, Figure 4). After the 3rd dose of the GnRH, the patient will be re-assessed if additional GnRH is needed or if already amenable to hysteroscopic polypectomy.
Case 3
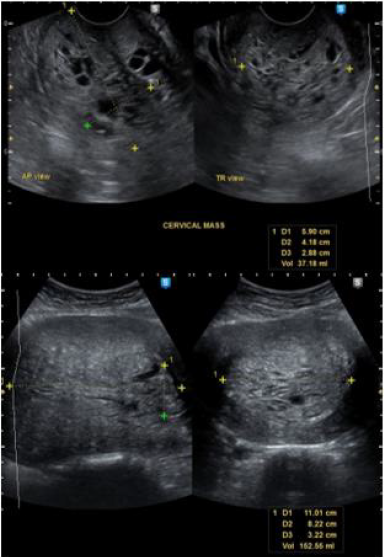
The last case is a 36-year-old, nulligravid who came in due to abdominal enlargement and inter-menstrual bleeding. Patient has no comorbid but is unable to conceive for 9 years with her husband. 1 year prior to consult, she began to develop intermenstrual bleeding, soaking 3 pads per day lasting 1-2 days associated with abdominal enlargement. On pelvic examination, there is a 3x3cm polypoid mass protruding out the endocervical canal, which seems to be coming from the endometrial cavity and the corpus is enlarged to 18-20 weeks size. Ultrasound showed an endometrial mass measuring 11.0 x 8.2 x 3.2cm with irregular cystic spaces and seems to be contiguous with the endocervical mass (See Appendix 3, Figure 1). Endometrial biopsy was done to rule out malignancy, and the result was endometrial polyp, hyperplastic type. Management was again GnRH for 3 doses and reasses if amenable for hysteroscopy. After her 1st dose of GnRH, the size of the corpus significantly decreased to 14 to 16 weeks size. Patient also reported fragments passage of meat-like material with minimal vaginal bleeding. Repeat ultrasound was done and the size also significantly decreased to 7.5 x 6.5 x 6.1cm (See Appendix 3, Figure 2). Patient is still for completion of 2 more doses of GnRH prior to re-assessment.
Discussion
Endometrial polyp is one of the most common structural causes of AUB among the reproductive age group. It could present as intermenstrual or heavy menstrual bleeding and the amount of bleeding is usually proportional to the size of the endometrial polyp: the larger the size, the more debilitating the symptoms. Aside from bleeding, it is also associated with infertility just as the cases presented. Endometrial polyps are formed from localized overgrowths of endometrial tissue composed of variable amount of glands, stroma, and blood vessels covered by epithelium. The stroma of a polyp is composed of fibroblast like spindle cells and large blood vessels with thick walls. Commonly, the size of a polyp is less than 2cm, however, polyps greater than 4 cm are called giant polyps, as shown in the cases above, whose sizes range from 10 to 12 cm. The development of endometrial polyps has been explained by a number of molecular mechanisms such as monoclonal endometrial hyperplasia, over-expression of endometrial aromatase and gene mutations [1]. It usually arises because of estrogen hypersensitivity in some areas of the endometrium, probably caused by hyperactivation of the beta or the alpha estrogen receptor during the first phase of the cycle. Furthermore, they do not shed with menstruation because the estrogen related inflammation block the apoptosis via bcl-2 gene expression. Giant polyps, on the other hand are known to occur due to unbalanced estrogen levels. This estrogen related polyp growth occurs due to angiogenic growth factors’ deregulation, produced under hormone control inside the polyp, within a short time and few cycles [2].
Histopathological examination must be performed on all resected polyps to rule out endometrial polyps (0.5%–3%) with malignant foci. Lasmar BP reported that endometrial polyps larger than 15 mm are associated with hyperplasia and Wang J et al. identified that polyps measuring more than 10 mm are associated with malignancy [3]. The 3 cases of giant polyps presented all underwent endometrial biopsy to rule out the possibility of malignancy prior to choosing conservative treatment, which was advocated since all 3 cases have issues with infertility. For the management of endometrial polyps, hysteroscopic resection is the preferred method [4]. However, in some instances like in giant polyps, immediate hysteroscopic removal may not be feasible. This could be due that giant polyps occupy the entire uterine cavity that distending the cavity during hysteroscopy for visualization of the polyp’s attachment may not be done. Aside from failed removal of the polyp, morbidities like fluid overload and uterine perforation can be encountered. Although there is limited evidence with the use of GnRH agonist in endometrial polyps, it’s use was suggested as it may significantly decrease the size of the polyps to make the hysteroscopic resection achievable.
GnRH agonists has revolutionized the management of many conditions in gynecology based on the discovery that when administered in a non-pulsatile fashion, they down regulate pituitary GnRH receptors, and therefore decrease the production of FSH and LH. It has been widely used for submucus myomas to decrease its size and make its hysteroscopic removal manageable with less morbidity. It used as a neo-adjuvant therapy prior to hysteroscopy to decrease bulk of the myoma and induce a state of hypoestrogenism. Pretreatment with GnRH agonists improves the hemoglobin level, reduces blood loss during surgery, and reduces uterine and leiomyoma volumes in as much as 40-50%, with most of the reduction occurs in the first 12 weeks [5]. This is especially helpful in infertile patients because this prevents destruction of the surrounding endometrial tissue [6]. Given the same concept for myomas, GnRH can then be used as pre-treatment for giant polyps since they have characteristic cytogenetic rearrangements similar to uterine leiomyoma [2]. As said previously, polyps contain estrogen as well as progesterone receptors, and the concentrations of these receptors are significantly higher in the glandular epithelium of endometrial polyps than those in the normal endometrium [7].
Hormonal inhibition of the endometrium can induce mucosal thinning and decreased bleeding. The effect of GnRH agonist can extend up to 1 month from the last dose and this could be due to persistent hypoestrogenism and consequent inhibition of regeneration of viable endometrial cells [5]. In the cases presented, GnRH agonist has significantly decreased the size of giant polyps even after 1 dose. All of the patients have reported vaginal bleeding along with passage of meat-like materials, which were believed to be fragments of the polyp spontaneously sloughing off from its attachment due to devascularizing effect of the GnRH agonist. None of the cases developed anemia or needed blood transfusion despite the said vaginal bleeding. The 1st case even successfully underwent hysteroscopic polypectomy after 6 doses of GnRH with no morbidity encountered and no residuals after, given the initial size of her polyp. With this in mind, there is room for GnRH agonists in treating endometrial polyps, specifically the giant polyps, where immediate hysteroscopic removal may tend to be difficult or may lead to failure, more so, morbidity. The cases have shown the effect of GnRh agonists in significantly decreasing the size of the polyps probably by inducing a hypoestrogenic state and at the same time deceasing the vascularization of the polyps causing it to spontaneusly slough off from its base. This will facilitate complete hysteroscopic removal of the giant polyp at the same time decreasing chances of morbidity. Although further studies are needed to strengthen its use in endometrial polyps, this may open an area for more research work.
Conclusion
Endometrial polyps, specifically the giant polyps, can be an incapacitating cause of abnormal uterine bleeding, which are often associated with infertility. In such cases, conservative management in the form of hysteroscopic removal is encouraged. However, given the size of a giant polyp, there will be technical difficulty in doing its resection. Use of GnRH agonist as neoadjuvant treatment for giant polyps can be advised. Using the same concept of GnRH agonist in shrinking myomas, it can induce a hypoestrogenic state causing devascularization of the endometrial lining. This will help significantly decrease the size of polyp, allowing complete hysteroscopic removal. However, further research studies are still suggested to strengthen its neoadjuvant use with giant endometrial polyps.





No comments:
Post a Comment
Note: Only a member of this blog may post a comment.