Evidence-Based Medicine: Era of Big Data
Introduction
More than 25 years have passed since the term evidence-based medicine (EBM) was introduced into the medical literature [5]. EBM is a concept that has evolved over time, initially clinicians considered that the decisions were made based on evidence, a more systematic approach was created to identify the most appropriate evidence an individual patient. This new approach was defined as patient-oriented evidence, meaning that the decisions are based on the clinical judgment of a capable expert, resulting from relevant medical literature witch follows a set of defined steps [1-6]. The most well established clinical guidelines are developed using methods that incorporate the EBM principles [1]. The successful implementation of EBM allowed a departure from the classic empirical practice that dominated medical history, however, the EBM approach provides only partly adequate solutions. The reason being that it is based on the premise “one size fits all”, this means that the solution found for the patient derives from information from a similar population. Consequently, medicine deals essentially with fragmented data, so the experts cannot master all the required knowledge [3]. This era of groundbreaking scientific developments in high-resolution, high-throughput data generating technologies is allowing the cost-effective collection and analysis of huge datasets on individual health, commonly refer as Big Data. This knowledge, makes it possible to achieve a data-driven approach centering on the individual, also known as personalized medicine, however, its implementation presents several challenges [3]. The most critical difference between EBM and MP lays on the fact that computational tradition, Big Data, is driven by data rather than hypothesis testing. This method works with raw observations and does not incorporate context knowledge into evidence production [7]. The long-term goals of MP are focused on: providing better-adapted, personalized surveillance measures and therapies and to significantly delay disease onset and, whenever possible, to prevent it. To achieve these goals, it is necessary to create a connection between MP and EBM [3].
Evidence-Based Medicine (EBM)
EBM is not only the application of knowledge acquired through literature, it is also the use of a series of steps to obtain relevant information for the patient in question and the incorporation of system of values related to the patient, that is, the wishes and preferences of the patient [1,4]. The EBM stages are typically [1,8,9]: 1) Formulation of the EBM question; The questions must be specific to a population, the more specific the easier it will be found in the literature. In addition, it must be well designed.
2) Gathering Evidence to answer the clinical question; The selection of relevant studies to gather all evidence necessary must be performed through a literature review. It is important to identify and use high-quality sources, such as MEDLINE, Cochrane Collaboration, among others;
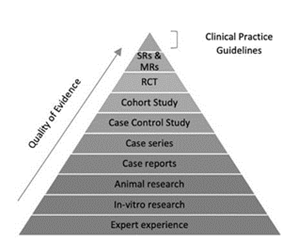
3) Evaluation of the quality and validity of the evidence: Not all scientific studies have the same value, they differ in terms of scientific strength and legitimacy, as defined in Figure 1. In addition to any type of study, individual examples vary in internal validity (quality of the methodology) and external validity (generalization of results). The levels of evidence are defined from 1 to 5 in decreasing order of quality. The types of study at each level vary in relation to the clinical issue but typically consist of:
• Level 1: Systematic reviews or meta-analyzes of randomized controlled trials and single high-quality, randomized and controlled trials
• Level 2: Well-designed cohort studies.
• Level 3: Case control studies with systematic review.
• Level 4: Low quality cohorts and case control studies.
• Level 5: Expert opinion without critical evaluation, based on reasoning about physiology, bench research or its underlying principles [10].
4) Decision to apply the evidence to the patient’s treatment; Since the best available evidence can be derived from a population of patients with different characteristics from the patient in question, it is necessary to make a detailed analysis about the applicability of the evidence to the specific patient [1,8].
Big Data EMB
The explosion of big data has made the traditional research methodology obsolete [4]. Big data methods offer expanded research power. Classification algorithms can act as diagnostic tests, classifying a patient as having or as not having a disease [7]. Evidence - based personalized medicine is based on three pillars: responsible inter-institutional sharing of large clinical harmonized data sets; data on vital signs and behavior collected by empowered citizens; and clinical bioinformatics required to convert this complex information into clinically useful knowledge, which will be then returned by the medical practitioners to the individuals concerned [3]. For the clinicians today, the technology is already available but new concepts and ways of thinking are still lacking. Future clinicians will not be responsible for the storage of knowledge but rather, they will be responsible for knowledge administration. They will apply the knowledge acquired from a complete set of data to their daily clinical practice and serve the patients even better [4,11]. Some of the stages of Big Data EBM can be: [4,9,11]
1) Formulating Questions; Determining the research area: disease, treatment, tests, principle, group, characteristics, among others.
2) Research of data from real cases: hospitals, operators, etc. (preferably in a defined period of time )
3) Evidence analysis, advanced analytics tools are used to transform the data collected from the heterogeneous sources into the consumable units;
4) Evidence Grading and Calculation of Statistical Significance;
5) Analysis of the results with the objectives defined for the research, in order to support the best evidence;
6) Evidence Presentation, presentation of medical evidence;
While EBM continues to be the guiding principle, clinicians should be aware of potential tainted results. In the future, big data is likely going to offer us a new aspect of EBM and arm us with more comprehensive data when we make our clinical decisions [4].
EBM Big Data: An Example
Genomic and other related big data are leading a new era of precision medicine. Genomic medicine attempts to construct customized strategies for diagnostic or therapeutic decision making by using patients’ genomic information. The way this will impact population health depends on its ability to affect large segments of the population [6,12]. Next-generation sequencing (NGS) technologies, targeted sequencing, and other associated technologies, are increasingly applied to biomedical research and medical practice to identify diseases, drug- associated genetic variants, diagnostic markers. Genomic data generated by NGS technologies is a vital component support genomic medicine and therefor to advance precision medicine [13]. Nonevidence-based use of BGD may be harmful and result in major waste of healthcare resources [6]. Cancer is a complex genetic disease that results from the accumulation of genetic alterations and depends on the individual predisposition to cancer and the somatic alterations that initiate and trigger the progression of cancer. Genetic alterations could serve as effective biomarkers for early detection, monitoring and prognosis of cancer. Big Data EBM makes it possible to magnify screening from a single gene to the whole genome by using genomewide genotyping for genome wide association studies (GWAS) or next-generation sequencing (NGS) for cancer genome profiling studies. With the use of this technologies it is possible to provide the right dose of the right drug for the right patient at the right time, based on the genetic profiles of cancer and the individual [14].
Evidence-based Medicine and Precision Medicine: How to?
This combination will require worldwide and responsible data sharing, as well as regularly updated training programs responsible for the interpretation of the increasing amount and complexity of data, analyses and sharing of standardized medically relevant data globally, data for modeling disease and for issuing reports to support the decisions of clinical staff. Big data EMB will shift progressively from therapy to prevention, thus leading eventually to improved, clinician-to-patient communication, citizen-centered healthcare and sustained well-being [3]. EBM practitioners would benefit from seeking data science partners to exploit the availability of new, largescale, diverse data and to enlarge their tool kit with machine learning methods that may offer less expensive, quicker, and more powerful approaches to generating evidence in some circumstances. Big data scientists, who often come from outside the health field, would also benefit from partnering with clinical researchers who have the disease knowledge to adjust for sources of bias and to recognize spurious signals. Evidence-based medicine needs the computational power of big data, and big data needs the epistemological rigor of EBM. Combining these 2 types of knowledge offers the best path for enlarging and strengthening the knowledge base of clinical medicine [15].
Big Data EMB: Barriers and Solutions
One of Big Data EBM’s barriers is connected to the guidelines related to electronic health records and other clinical tools, that are overly restrictive [6]. Clinical tools are often built on representative patient population and may not reflect the individual patient. To overcome this barrier the guidelines can be adapted to the patient and use a shared decision making to help patients chose the most effective option [5]. Aggregation of heterogeneous data sets into electronic health records is important to achieve de goals of MP. The data is of multiple heterogeneous types, furthermore, storage and analysis of large data sets is not easily obtained by using current EHRs. There is a clear necessity for robust standardized procedures to ensure reliability, efficiency and an higher-level management of EBM. However, EHRs are not only heterogeneous but they can have incomplete, inconsistent, or inaccurate data, as well as additional limitations that further hinder their applicability, scalability, and semantic and technical interoperability [3,5]. Efforts to simplify the application of precision medicine into clinicians’ practice are improbable to be successful except if the EBM system became integrated into their Workflows [11]. Big Data EBM must be taught in an interactive and clinically based way, in order to fill the lack of knowledge of this practice. Even with the evolution of this concept, for many conditions, there is still no relevant evidence. In addition there is still incomplete evidence and conflicting evidence, so a set of guidelines with a low level of bias should be used in order to strengthen the clinical judgment. The clinician himself must keep abreast of the literature and be prepared for changes in practice due to changing evidence [5,6].
Conclusion
The paradigms of evidence-based medicine and personalized medicine both have strengths and weaknesses. The field of personalized medicine should advance with caution, avoiding overselling [3]. EBM´s success in providing a framework for fully integrating research evidence into the delivery of health care and raising awareness of the need for consideration of individual patient values and preferences. This framework has evolved over time in order to bridge the advances in medicine, so it may come to incorporate the era of big data that we live in and remain enduring contributions to clinical medicine and related fields [15].
For more Articles on: https://biomedres01.blogspot.com/



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.