Jaundice Clinical Manifestation and Pathophysiology: A Review Article
Introduction
Jaundice is when clinically there is an increase in the amount of bilirubin in the serum rising above 85mmol/l (5mg/dl). When in utero, unconjugated bilirubin is cleared in the placenta to produce cord serum bilirubin of approximately 35mmol/L (2mg/ dl). After birth, jaundice is a reflection of the bilirubin present in the liver, the rate of hepatic excretion and the ability to bind to serum proteins to retain the bilirubin present in the plasma. Many variations in individual responses to bilirubin load prevent specific levels of psychological jaundice [1]. Therapy has proven that the benefits outweigh the harm. The physiological pattern of jaundice also varies with other factors such as prematurity and ethnicity. In hemolytic jaundice, serum bilirubin exceeds physiologic levels and can be caused by sepsis and inherited hemolytic diseases such as glucose 6-phosphate dehyrogenase (G6PD) deficiency, ABO and Rh isoimmunization [2]. Prolonged jaundice refers to jaundice that persists beyond the first two weeks of long neonatal life, and is caused by other diseases, including lateonset jaundice of the breast, congenital hypothyroidism and rare inherited disease conditions. Infants with breast milk jaundice have prolonged levels of unconjugated bilirubin in other healthy infants, and glucuronidase b in breast milk appears to be an important factor in this condition. There are two types of neonatal jaundice associated with breastfeeding, the first known as lactational jaundice associated with treatment of the breast which results in dehydration and causes the jaundice to become more intense [3]. The second is breast milk jaundice which is associated with prolonged jaundice in infants with the first two weeks of life. One or more substances such as enzymes (glucoronidase), 3 alpha, beta and 20 pregnanediol in breast milk although to be possible cause of breast milk jaundice. Jaundice is influenced by several factors, namely dehydration, weight loss after birth, bleeding, cephalohaematoma, contusions, babies in mothers with diabetes, acidosis, apixia, and gastrointestinal obstruction [4].
Discussion
Clinical Manifestation and Etiology
Patients with jaundice may not experience any symptoms, although some present with a life-threatening condition. Patients who present with acute illness, which is usually due to infection, may present with fever, chills, abdominal pain, and flu-like symptoms. In these patients, skin discoloration may not be their chief complaint. Patients with non-infectious jaundice may complain of weight loss or pruritus. Abdominal pain is a symptom that usually appears in pancreatic or biliary tract carcinomas. Occasionally patients present with jaundice and accompanying extrahepatic manifestations of liver disease
Jaundice can be caused by a number of things, including [4,5]:
a. Haemolysis due to ABO or Rh isoimmunisation, resulting in G6PD. deficiency
b. Hereditary spherocytosis, drugs
c. Sepsis - septicaemia, meningitis, UTI and intra-uterine infections
d. Polycythaemia
e. Psychological and idiopathic jaundice f. Breastfeeding and Breastmilk jaundice.
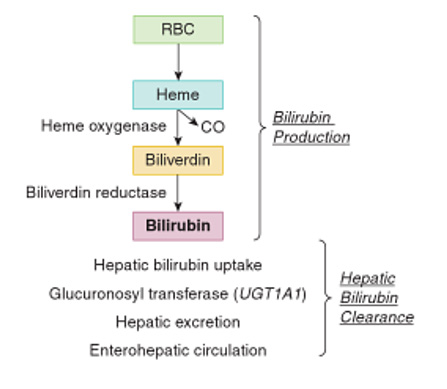
There is a reduction in the erythrocyte cycle in normal newborns (70 to 80 days in infants and 120 days in adults) increasing the amount of bilirubin in neonates. Hereditary hemolytic changes lead to increased RBC turnover and increased risk of hyperbilirubinemia. This causes hemolysis in newborns which is divided into several causes, namely first, damage to RBC metabolism resulting in G6PD and pyruvate kinase deficiency. The second is RBC membrane damage, of which congenital sporocytosis is an important factor. The third is impaired hemoglobin production where alpha thalassemia syndrome is the main cause in newborns. Fourth is an inherited immune hemolytic disease called medelian trait [6] (Figure 1). Schematic drawing of bilirubin production in neonates [7]. Bilirubin metabolism occurs in three phases, including the prehepatic, intrahepatic and posthepatic phases. Dysfunction in one or more of these phases can lead to jaundice [8].
a. Prehepatic jaundice
The human body produces approximately 4 mg/kg of bilirubin per day from heme metabolism. Approximately 80% of heme is the result of erythrocyte catabolism, with the remaining 20% resulting from ineffective erythropoiesis and the breakdown of muscle myoglobin and cytochromes. Bilirub that is formed will be transported from the plasma to the liver to be conjugated and excreted.
b. Intrahepatic jaundice
Unconjugated bilirubin is both fat soluble and water insoluble, and therefore can easily cross the blood-brain barrier or cross the placenta. In hepatocytes, unconjugated bilirubin will be conjugated with sugar catalyzed by the glucuronosyltransferase enzyme and finally dissolved in bile.
In the intrahepatic phase, disorders associated with bilirubin can be divided into three subgroups [5,9]:
1. Excessive production of bilirubin
2. Disturbance in the conjugation process
3. Impaired excretory function
c. Posthepatic Jaundice
After dissolving in bile, bilirubin is transported through the bile duct and cystic duct for temporary storage in the gallbladder, or through the ampulla of Vater and into the duodenum. In the intestine, some bilirubin will be excreted in the feces, while the rest is metabolized by the normal intestinal flora into urobilinogen and will then be reabsorbed. Most of the urobilinogen will be filtered from the blood by the kidneys and excreted in the urine. A small amount of urobilinogen is absorbed in the intestine and excreted into the bile [8,9].
Jaundice can be classified into three main groups. This division is based on the presence of bilirubin found in serum [10]:
a. Unconjugated (indirect)
Albumin is insoluble in blood, therefore albumin is bound to blood. The free bilirubin is then combined with albumin and transported to the liver. In the liver there is an uptake mechanism, so that bilirubin is bound by liver cell membrane receptors and enters the liver. As soon as it is present in the liver cells, ligandin (Y protein), Z protein and other hepatic glutathione compounds occur which carry it to the hepatic endoplasmic reticulum, where conjugation occurs 4.
b. Conjugated (direct)
Conjugated bilirubin is formed in the rough and smooth ER, where it is conjugated with glucuronic acid. The result is water-soluble bilirubin (monoglucuronide and diglucuronide) a process that catalyzes glucoridation by uridine diphosphateglucuronosyltransferase, which occurs with the help of two isoenzymes. Excretion of bilirubin into bile is actively carried out by ATP-dependent transporters. Billirubin is transported into the stomach by the help of cells. Apolar glycuronide bacteria produce water-soluble unconjugated bilirubin, which can be converted to urobilinogen by reducing bacteria.
c. Albumin and bilirubin binding (indirect) [11,12].
Conclusion
Delta bilirubin is a small amount of conjugated illirubin. In serum irreversibly bound to albumin by covalent bonds. In laboratory tests to determine albumin levels, directly conjugated delta albumin is usually referred to as jaundice and is protracted, in which delta bilirubin levels rise proportionally and results jaundice.
For more Articles on: https://biomedres01.blogspot.com/



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.