ABO Blood Group Profile Frequencies and Relationship in COVID-19 Disease Susceptibility and Severity in Lagos, Nigeria
Introduction
COVID-19 caused by the Severe Acute Respiratory Syndrome Coronavirus-2 [SARS-CoV-2] was first described as a serious infection leading to significant morbidity and mortality in Wuhan, China in January 2020 Zhou, et al. [1]. The number of deaths was increasing due to the catastrophic effect of the emerging new strains. Research has shown that there are predicting factors of COVID-19 severity such as demographic, clinical, immunologic, haematological, biochemical, and radiographic factors Benjamin, et al. [2]. According to Samra, et al. [3] ABO groups can play a role in COVID-19 severity and susceptibility. The rapid global spread of the novel coronavirus SARS-CoV-2 has strained existing healthcare and testing resources, and it is causing COVID-19 severe cases in some people than in others. While some people experience only mild symptoms, others are being hospitalized Samra, et al. [3]. The pathogenesis of severe COVID-19 and the associated respiratory failure are still unclear, but the higher mortality rate is consistently associated with older age and being male Samra, et al. [3]. Many studies have shown that the ABO blood type is a potential risk for various diseases such as cancer, myocardial infarction, acute kidney injury, and venous thromboembolism Dentali, et al. [4,5]
Apart from comorbidities and other predicting factors, findings have shown that the ABO blood group has a correlation with COVID-19 susceptibility and severity. Biological factors that determine susceptibility to SARS-CoV-2 and severity of COVID-19 are yet to be fully understood Samra, et al. [3]. The ABO blood grouping may influence the susceptibility of COVID-19 and severity of the disease Zhao, et al. [6]. As reported by Nagla, et al [7], patients from three hospitals in Wuhan, Shenzhen, and China showed the likelihood of association between ABO blood groups and the susceptibility to COVID-19 exposure after the outbreak of the COVID-19 infection. The study results showed that individuals with blood group A had a markedly greater risk of COVID-19 exposure, while those with blood group O had a significantly reduced risk of COVID-19 infection. In a meta-analysis of two different case-control cohorts, blood group A was reported to confer a greater risk of aggravated COVID-19, while blood group O offer protection against COVID-19 infection WU, et al. [8].
However, A, B and O blood group are antigenic complex oligosaccharide molecules located on the extracellular surface of the red blood cell membrane Storry JR, et al. [9]. ABO blood group are also expressed on the surface of other human cells and tissues, including the epithelium, sensory neurons, platelets, and the vascular endothelium Eastlund [10]. The ABO blood group have been reported to play a key role in various human diseases such as diabetes, cardiovascular, neoplastic, carcinoma and other infectious disorders Cheng et al. [11-13]. ABO and Rh blood groups polymorphism are valuable and indispensable tools in contemporary medicine, population genetics and anthropology. The distribution of these two blood groups has been reported different populations of the world and they showed considerable variation in different geographic locations, reflecting the underlying genetic and ethnic diversity of human populations Garratty ,et al. [14,15] reported the distribution and gene frequencies of ABO and Rh [D] blood group systems in six geopolitical zones of Nigeria. Their data revealed that the ABO blood group frequencies were found in the order O [52.93%] A [22.77%] B [20.64%] and AB [3.66%] respectively among Nigeria population. This was in agreement with other studies from other parts of the world from different race and ethnic groups in USA having [O; 46.6%, A; 37.1%, B; 12.2% and AB; 4.1%] Garratty, et al [14]. Another report from a study done in Mauritania, Morocco, Cameroun, Tunisia, Ethiopia and Iran is also consistent with the Nigerian study showing [O > A > B > AB] Hamed, et al. [16-21]. The report from Madagascar and Guinea showed slightly different result [O > B > A > AB]. However, Nigerian ABO blood group results are slightly different from the study in Madagascar and Guinea that reported this trend [O > B > A > AB] Randriamanantany, et al. [22,23]. Reports from studies in India and Bangladesh showed blood group B having highest prevalence followed by O and the least was AB [B > O > A > AB] Dewan, et al. [24,25]. In Nigeria, there is a limited information of association between ABO blood groups and the susceptibility to COVID-19 in Nigeria. This study therefore, evaluated the role of ABO blood group in SARS-CoV- 2 infection susceptibility and disease severity in Lagos, Nigeria.
Methods
Study Design and Participants
This study is a case series that includes patients that are evaluated between June and August 30, 2020, and diagnosed with COVID-19.With ethical approval obtained from the Institutional Review Board [IRB] at the Nigerian Institute of Medical Research [NIMR], Yaba, Lagos, Nigeria, patient data were obtained and reviewed at the Mainland Infectious Disease Hospital and the Nigerian Institute of Medical Research, Yaba. Informed consent was also obtained from the study participants before their health records were obtained. They were confirmed to have been infected with SARS-CoV-2 by a positive reverse transcriptase polymerase chain reaction test [Qpcr] of nasopharyngeal, throat and blood samples. Clinical outcomes were also monitored and recorded.
Data Collection and Statistical Analysis: Clinicians and trained research assistants retrospectively reviewed and copied patients’ health records out to a standardized data collection form. Health records copied out include demographic information, signs and symptoms presented with, co-morbidities, and patient outcome. A formal sample size was not calculated for this study because the objective of the study was to describe the clinical characteristics of the patients and their Blood group profile of participants who had enough information in their health records for analysis. Records were double entered into the forms before merging to reduce errors during data entry. Descriptive analyses were performed using Statistical Package for the Social Science [SPSS] version 25 [IBM, USA].
Results
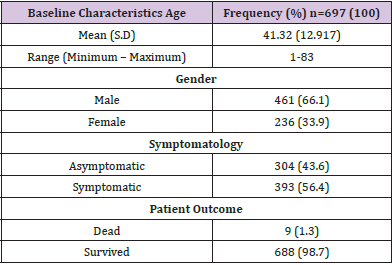
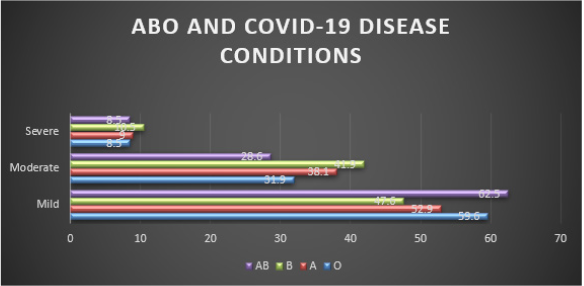
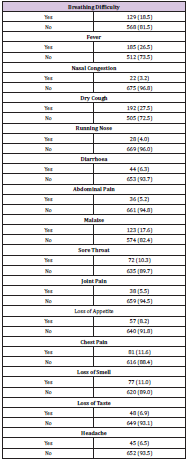
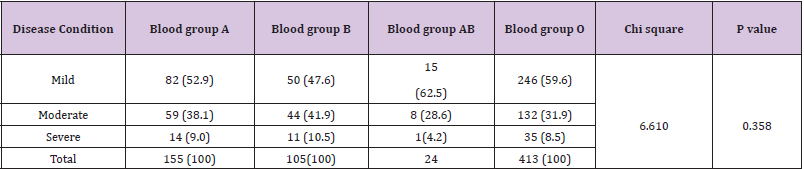
A total of 697 COVID-19 patients were included in this study. The mean age [S.D] of the study participants is 41.32 [12.917]. COVID-19 was common in males [66.1%] than in females [33.9%]. Out of the 697 participants, 43.6% were asymptomatic while 56.4% were symptomatic showing symptoms like breathing difficulty, fever, dry cough, running nose, sore throat and others as shown on Tables 1 & 2. The most frequently detected blood group in the population was O accounting for [59.2%], followed by A 155[22.2%], B 105[15.10%] and the least is AB 24[3.4%]. Figure 1 showed the blood groups that accounted for COVID-19 severity: blood group B 11 [10.5%] followed by A 14 [9.0%], O 35 [8.5%] and AB 1 [4.2%]. There was no significant statistical difference between the blood groups in relation to COVID-19 severity [p=0.358].
Table 2: Symptomatic patients (56.4%). The most common symptoms were: dry cough (27.5%), Fever 185 (26.5) and breathing difficulty (18.5%).
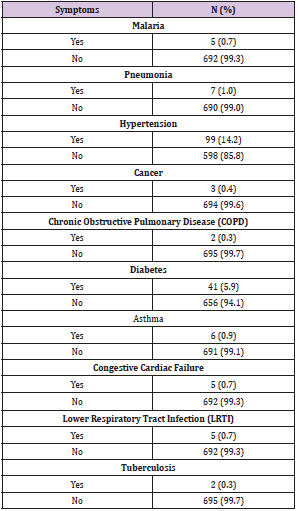
Tables 3 & 4 showed five [5] persons having blood group O were among the deceased [55.6%]. Four out of the 5 deceased had severe COVID-19 and were males. Their age, ranged from 53 to 65 years. The youngest being 53years was a woman who had a mild symptom of COVID-19. Three [3] women having blood group A were among the deceased [33.3%]. Aged ranged 66-75 years. Two out of these three women had mild cases and one severe COVID-19 case. This is a proof to show that old age and co morbidities are risk factors to COVID-19 disease complications and death. Five [5/ 55.6%] persons having blood group O were among the deceased four out of the 5 deceased had severe COVID-19 and were males and aged 53 to 65 years. The youngest being 53 years was a woman who had a mild symptom of COVID-19. Three [3/ 33.3%] women having blood group A were among the deceased. Their age ranged from 66 to 75.
Discussion
A person’s blood group [A, B, AB and O] is determined by the presence or absence of specific antigens on red blood cells which trigger an immune response. Reports from some recent studies, suggests that ABO blood group may play a role in the immunopathogenesis of COVID-19 disease with group A conferring a higher susceptibility to infection and or severe disease and group O individuals less likely to test positive (Geol, et al. [26]) and Fan, et al. [27]. However, reports are in contrast to our current study which shows no statistical ssignificant evidence [p = 0.358] that individuals with the blood group profile A were associated with increased risk to severe cases of COVID-19. Furthermore, in moderate cases of Covid-19 infection, group B [41.9%] individuals were more represented and may have increased risk to COVID -19 susceptibility when compared to other blood groups. We also observed that most of the deceased persons [5/ 55.6%] had blood group O, were males and age 53 to 65 years. Three [3/ 33.3%] women having blood group A were equally among the deceased aged 66 to 75 years with co-morbidities which include Pneumonia, Diabetes, LRTI , Hypertension in both severe and mild cases confirming that both age and comorbidities can lead to death with COVID-19 disease.
A recent study that supported our data reported that a significantly increased risk was associated with blood group B Almadhi, et al. [28], which is also comparable to findings by Latz, et al. [29] and meta-analysis by Liu, et al. [30]. In Nigeria and other parts of the globe, blood group O Rhesus positive has consistently been the most common, followed by A, then B, and AB being the least [Anifoweshe et al 2016]. According to [Geol et al 2021], group O originated in Africa before early human migration, and has anti‐A and/or anti‐B antibodies present in group O individuals which binds to the corresponding antigens on the viral envelope and contribute to viral neutralization, thereby conferring some protection by preventing target cell infection. However, our data proposed that group B and or O individuals may be more likely to be infected with COVID-19 disease suggesting that COVID -19 in Nigeria and few other studies from other parts of the world may not be affected by the anti A or B that has been proposed to confer protection to these that have it. Furthermore, ABO blood group is determined by inheritance, natural selection, showing underlying genetic and ethnic diversity which may have influenced the current frequencies of ABO types among Nigerian populations based on susceptibility to particular diseases or disorders. Hospitalization, higher infection chances, and death were found among those with blood group A and O, and ethnicity was also a factor considered to weigh COVID-19 risks in this study.
Conclusion
The ABO blood group was not associated with the presentation and recovery period of COVID-19 disease during the period of this study. However, the patients of blood group B profile seem to have higher risk of COVID-19 disease susceptibility. To further detect the susceptibility and severity of COVID-19 infection, more samples of individuals with confirmed exposure to COVID-19 infection should be conducted.
For more Articles on: https://biomedres01.blogspot.com/



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.