Management of Penile Fracture with Urethral Injury in Haiti
Background
Penile fracture is a urological emergency requiring operative management [1,2]. Considered a rare and underreported traumatic injury [3-6], it has a reported incidence ranging from 0.29 to 1.36 per 100,000 people [1] and affects 1/175,000 men in the USA [6]. It is defined as a rupture of the tunica albuginea of the corpus cavernosum and occurs when the penis is erect [1,2,7] Erection causes thinning of the tunica, with its thickens reduced from 2 mm to 0.25-0.5 mm, and it becomes vulnerable to trauma [6]. The main cause of penile fracture is coital trauma, which represents 1/3 of all trauma to the penis. In very rare cases it is accompanied by rupture of the urethra which occurs in 1% to 38% of cases of penile fracture reported globally [1,2,8,9]. Some African studies revealed the main cause is masturbation [10]. Management of penile trauma has evolved over time. Initially, penile fractures were managed conservatively and non-operatively. However, due to the high complication rate observed, emergency surgical management has been the standard of care since 1980, which considerably reduces rates of long-term complications as erectile dysfunction [1,9,11-16]. To our knowledge this is the first described case from Haiti, we present a case of traumatic penile fracture and an associated urethral injury which presented to the emergency department at the State University Hospital of Haiti and managed operatively by the urology service.
Case Presentation
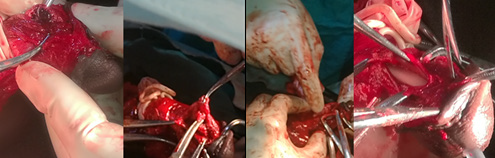
Our patient was a 49-year-old man with no known medical history. He presented to the emergency department with a six hours history of urethrorrhagia and difficulty of retracting the glans. He reported taking sexual stimulants and subsequently engaging in vigorous sexual intercourse during which he heard a sudden cracking noise at the penis after bumping the perineum of his female partner. He reported engaging in vigorous vaginal penetrative sex from the posterior position (i.e., doggy style). After the sound, he passed blood from the meatus, followed by pain and edema in the body of the penis. Given the increasing intensity of the pain and the persistent hemorrhage, the patient decided to come to the Urology Emergency Department. Initial clinical examination was remarkable for a leftward deformity of the penis, most markedly in the distal 1/3 of the organ, edema without apparent ecchymosis (Figure 1), and passage of blood via the urinary meatus. There was difficulty in retracting the glans and pain was most severe at the point of swelling. Examination of the scrotum and perineum was unremarkable. The diagnosis of penile corpora cavernosa fracture was made and the patient was consented and prepared for operative repair. The operation was initiated by the in ligature and section of frenulum artery followed by a circular incision was made through the balanopreputial groove to strip it down to the root (Figure 2). A tourniquet was placed for less than 30 minutes and exploration of the penis was initiated where clots were identified, hematoma was drained and wound was washed with 0.9% serum saline.
Figure 1: Description of the fractured penis with leftward deformation and edema of the penile shaft.
Exploration of the penis revealed an injury in the corpora cavernosa on the right distal to the urethral meatus approximately 2.5 cm away. This was repaired with Vicryl 0, followed by a sealing test using 0.9% serum saline and removal of the tourniquet (Figure 3). After exploring the corpus cavernosum, we started the exploration of the urethra using a Nelaton catheter 16, which allowed us to identify and evaluate the anterior urethral injury which was approximately 3 cm in length and located at 5 cm from the urinary meatus. We proceeded to dissect the urethra circumferentially, then we proceeded to repair the urethral mucosal injury with (interrupted) Vicryl 4.0 suture over a 16 Fr. Foley catheter. A reassuring erection test with Nacl 0.9% was performed, and then we repaired the albuginea with (interrupted) Vicryl 2.0. Next, a second circular incision 5 cm (distal) from the first one was made, and we proceeded to repair the skin to the mucosa with a (interrupted) chromic 2.0, followed by the repair of the frenulum. At the conclusion of the procedure a sterile dressing was placed and the Foley catheter remained in place. The procedure which lasted approximately 2hr 45 min.
Discussion
Penile fracture is the traumatic rupture of the albuginea attached to the corpus spongiosum [1,3,17]. This structure has a bi-layer of collagen, which provides a significant tensile force resisting the intracavernous pressure which can rise to1500 mm Hg. This tensile strength is essentially provided by the outer layer of the albuginea, the thickness of which decreases considerably during erection (2 mm to 0.2-1.5 mm) and thus weakens the corpora cavernosa [6,9]. Any situations or evens which elevate the intra-cavernous pressure above 1500 mm Hg are a risk factor for penile fracture due to the rupture of the albuginea and the corpus spongiosum [18]. These situations include the use of oral sexual stimulants and sex under psychological pressure, like extra-marital sex [2,6]. Our patient admitted to having used oral sexual stimulants prior sexual act. Diagnosis of penile fracture is essentially clinical [5,15,16]. The majority of cases involve a history of trauma, especially and more than a third of cases report coitus [1,2,19]. Other causes of trauma can lead to penile fractures, such as a fall from the top of the bed during sleep, direct blunt impact, and penetrating injuries such as that made by projectiles [1,2]. It is uncommon to see penile fracture with concurrent urethral rupture. The prevalence reported varies by region of the world. It is 3% in Asian and African countries, while it is around 38% in Western countries [6,8]. Furthermore, certain sexual positions favor the occurrence of penile fractures with or without rupture of the urethra.
Among these positions, the doggy style position and the position where the woman is on top are the most often described cases [14,20-22]. However, other positions can result in penile fractures as well. The most consistent clinical sign of penile fracture with urethral rupture is hematuria, followed by urethrorrhagia, dysuria, and urinary retention [5,18,23,24]. However, the absence of these signs does not exclude a penile fracture with urethral injury [13,18]. Furthermore, there are the classic signs of penile fracture such as pain, edema, ecchymosis, and the classic “eggplant” deformity [4,5,16,18]. Our patient presented with a similar picture; he had urethrorrhagia, edema, pain and an eggplant deformity. Imaging studies can be used in certain well-determined circumstances, among them sonography and cavernosography, retrograde urethrography, MRI, and cystourethroscopy [15]. These are not recommended in emergencies where the clinical exam is usually sufficient to make the diagnosis and to expedite emergent surgical management [12]. This was the case for our patient who had almost all the clinical signs, and thus we expedited his penile anesthetic block and operative repair. Since 1980, emergency surgery is recommended in all cases of penile fractures. The British Association of Urological Surgeons recommends surgery within the first 24 hours [14] in order to reduce the risk of longterm complications. Bozzini et al. observed a complication rate of 7.6% in patients operated before 24 hours and 68.7% in patients operated 24 hours after injury [12,14].
Our patient underwent the procedure approximately 12 hours after admission. The wound was approached by a coronal suture (Figure 2), the most commonly technique used, which gives better exposure, improved post-operative aesthetics, and facilitates dressing changes [2,9,18]. However, some studies have shown that this approach is associated with risks of infection and necrosis [9]. The rupture of the corpus cavernosum was partial as is the case in the majority of penile fractures [9,12] and measured 2.5 cm, while the urethral wound was mostly anterior and 3 cm in length. Studies have shown that urethral rupture is most common in bilateral fractures [12,14,19] and is often ventrolateral where the tunica albuginea is thinner [14]. Reports recommend the use of urethrography or retrograde cystography in cases of fracture with signs of urethral rupture [12,14,19]. In our case this was not available, so we have used a 16 Fr catheter a very common practice and highly recommended by some researchers and we proceeded to operative exploration with ultimate repair of the albuginea as recommended [4,19] with Vicryl 2.0. . Our patient has had a good clinical outcome. Post-operatively, he was followed for 2 days in the inpatient surgical ward. He received antibiotic coverage with ceftriaxone. After discharge on post-operative day, he was evaluated regularly at 3-day intervals with changes of the petroleum-based dressing and re-application of topical neomycin for the first 15 postoperative days. The patient was instructed not to wet the wound and to continue the neomycin application until complete healing. The foley was removed one month post-operatively, and the patient had satisfactory urinary function. Return to sexual intercourse was advised at 2 months post-operatively.
Conclusion
Any patients presenting with hematuria and/or urethrorrhagia in whom clinical history suggests penile fracture, an evaluation of urethral injury must be performed. The diagnosis is essentially clinical and requires surgical intervention within the first 24 hours after injury. After operative repair, return to sexual activity is recommended after 6-8 weeks. In developing country like Haiti, with limited resources like cystogram or retrograde urethrogram, clinical evaluation and surgical emergency is key to avoid long term complications.
For more Articles on: https://biomedres01.blogspot.com/





No comments:
Post a Comment
Note: Only a member of this blog may post a comment.