Effects of Two Different Types of Tele-Monitored Physical Training on Cardiac Autonomic Modulation in Healthy Young People
Introduction
In recent decades the importance of physical exercise has become increasingly evident, has been explored in order to help researchers and professionals to develop ways to stimulate people to have an active routine of physical exercises, besides being considered an excellent medicine for various cardiovascular, psychic, neurological and other diseases [1]. Physical exercise is a subcategory of physical activity characterized as a set of body movements that planned and structured in a similar way, maintain or improve some physical capacity [2].
The Ministry of Health of Brazil [3] disclosed measures to prevent the spread of the disease in the country, suggesting social isolation for disease control. Thus, tele monitoring has become a viable way to stimulate the body and mind, as a way to combat sedentary lifestyle and COVID-19 itself [4,5]. Due to the pandemic established by COVID-19, the sedentary habits of the population were evidenced. According to WHO, sedentary lifestyle is considered the fourth risk factor for death in the world, emphasizing the importance of physical exercise, being directly related to the prevention and treatment of chronic diseases in addition to other benefits [5].
After talking about the measure of social isolation, there was a need to seek a practice that could bring the benefits of exercise but that maintained the recommendations of the WHO, so the telemonitored exercises (home based) appear as a feasible and feasible modality. Although there is still no consensus on the best type of training for the prescription of exercise. Cristo, Nascimento e Sachetti [6] conducted a systematic review with 7 clinical studies and concluded that there were better levels of long-term physical activity, improvement in the performance of executive functions, reversal of depression, through telemedicine and home telerehabilitation.
In recent years, high intensity interval training has gained several fans. Gibala e Mcgee [7] characterize High-Intensity Interval Training (HIIT) as intense activities performed with a maximum or submaximal effort with rest intervals or low activity between maximal stimuli. Paz, Fraga e Tenório [8] in a meta-analysis they cite benefits such as increased VO2 max., fat percentage loss and a time-efficient tool to promote cardiometabolic adaptations compared to MCIT.
Some protocols are well known as the Tabata [9], a method created by japanese scientist Izumi Tabata in 1996, which consisted of 8 exercise sessions with stimuli of 20 seconds and 10 seconds of rest. And the Wingate test involves 30s of maximum cycling, repeating 4 to 6 times with an interval 5 minutes of recovery. Fleck e Kraemer [10] define resistance training (RT), with weights or strength, as an exercise requires the body musculature to try or move against a resistance force, and may be imposed by other equipment or free weight. Thus, it becomes a viable alternative for people to seek to improve or maintain physical fitness levels, besides having a cost-benefit in the midst of the COVID-19 pandemic.
According Camm et al., [11] the Autonomic Nervous System (ANS) controls the visceral functions of the body through the sympathetic and parasympathetic pathways, seeking to maintain internal homeostasis. The parasympathetic pathway is responsible for maintaining basic rest activities while the sympathetic route increases the heart rate during physical exercise, seeking to meet energy needs. Heart rate variability is a noninvasive tool that can be used to measure the variation between heart rate and adaptation of the cardiovascular system throughout the day, in order to identify possible heart and systemic diseases.
The research question consists of: What are the effects of two different types of physical exercise on cardiac autonomic modulation in healthy young individuals? With the latest studies, interval training has proposed several benefits to its practitioners, it is believed that Tabata can promote similar results in a short exercise time and in a safe way, based on the variability of heart rate in order to verify the appropriate intensity to be prescribed. Thus, the aim of this study is to evaluate the effects of two different types of physical training on heart rate variability in healthy young people.
Materials and Methods
The methodology of the present study was developed in accordance with the recommendations proposed by the CONSORT Statement. This is a randomized controlled clinical trial developed in the resistance and health training laboratory (LTRS) of the Araguaia University Center in the city of Goiânia.
The sample consisted of 24 participants, of both sexes, according to consecutive order of recruitment. The individuals in the study were selected based on the inclusion/exclusion criteria mentioned below, based on digital media advertising in the city of Goiânia.
The inclusion criteria were the signing of the Free and Informed Consent Form (TCLE), age between 18 and 35 years and being sedentary (last 3 months). As exclusion criteria, being hypertensive, diabetic, recent cardiovascular event (last 3 months), liver disease, orthopedic limitations or any physical or mental limitation that prevents the performance of exercises.
Study Procedures
All patients, after signing the Informed Consent, participants went through three distinct stages in the execution of the study, which are: evaluation, intervention and reassessment.
Evaluation
At this stage, the reading and signing of the TCLE, anamnesis and clinical evaluation, evaluation of body composition, evaluation of localized muscle resistance, recording and capture of R-R intervals for analysis of heart rate variability (HRV) occurred. After evaluation, the subjects will be randomized into the intervention groups.
Intervention
The intervention was performed through a Tele-exercise Program (or tele-monitored exercise): meeting the recommendations necessary in the face of the pandemic by COVID-19 and as a way to evaluate the effectiveness of this model of care for volunteers, participants must have equipment for monitoring (computer or mobile videoconference with installed applications that will be previously delimited with the study participants, and webcam and microphone) that will be held virtually and with the presence of a professional in all sessions to accompany all volunteers (to evaluate exercise execution, perform corrections and offer stimuli to participants), the exercises will be established by the researchers and will be similar to face-to-face programs.
After the evaluation and randomization of the volunteers, these were allocated into 3 distinct groups:
a. Group 1 – Interval Training Group (ITG): Started with 9 minutes per week of aerobic or resistance exercises in the first two weeks, increased to 12 minutes weeks at weeks 3 and 4 and increased to 15 minutes per week at weeks 5 and 6 (Very accelerated breathing, very panting. Modified Borg > 7);
b. Group 2 – Resistance Training Group (RTG): Will perform 45 minutes per week of resistance exercises in the first two weeks, increased to 60 minutes weeks at weeks 3 and 4 and increased to 75 minutes per week at weeks 5 and 6 (Accelerated, panting, but controlled breathing. Can you say a sentence, Borg 4 to 7);
c. Group 3 - Control Group (CG): They did not intervene, they were advised to continue their routine and habits normally, but the evaluations were invited as well as the other groups.
Reassessment
After the intervention period, the volunteers were submitted to reassessment to measure the effects of physical exercise programs: assessment of body composition, evaluation of localized muscle resistance, recording and capture of R-R intervals for analysis of heart rate variability (HRV).
Clinical Evaluation
Protocols
The experiments were carried out in the morning and early hours, in an air-conditioned room with relative humidity between 40 and 60% and temperature between 22 and 24ºC according to recommendations of the ACMS [12]. Participants were instructed not to drink beverages that contained alcohol or caffeine 24 hours before and on the day of the tests, not to perform physical exercises or strenuous activities the day before the application of the protocols, to have a light meal at least 2 hours before the tests and to bring comfortable clothes and sneakers suitable for training.
The participants were familiar with the evaluation and training room, with the researchers, procedures and equipment to be used. Before starting the test they were interviewed and examined to confirm their state of good health and whether they had slept appropriately the night before. The participants were also instructed not to speak unnecessarily during the evaluations in order to avoid interference in the capture of the evaluated signals. However, any change in its general condition before, during or after the application of the protocols should be communicated for the purpose of ensuring safety and well-being of the protocol during testing. Only people related to the experiment were allowed to be present during the data collection process.
Body Composition Assessment
Body mass (BM) was evaluated in a digital scale (2096PP®, Toledo®, São Paulo, Brazil) and height in a portable statometer (Professional Statometer®, Sanny, São Paulo, Brazil). Body mass index (BMI) was calculated by dividing body mass (kg) and height square (mt). Hip circumference (WC) was measured with anthropometric tape (Sanny®, São Paulo, Brazil), positioned at the midpoint between the upper iliac crest and the last costal arch at the end of expiration at rest, and hip circumference will be measured in the region with the highest gluteal bulge [13].
Recording of HR and iR-R for Evaluation of Cardiovascular Autonomic Control
This procedure focused on evaluating cardiac autonomic modulation in resting conditions in the supine position for 10 minutes. The HR and dosiR-R records were collected from the Polar Frequency Meter model® V800 (Electro Oi, Finland). The data were captured from a belt with coded transmitter, placed in the chest region, at the height of the 5th intercostal space and, later, transferred through an interface to a compatible computer.
Two HR evaluations were performed in the two days of evaluation and reassessment. During the collection period, the volunteers were instructed to maintain spontaneous breathing. Volunteers with respiratory rate (RF) lower than 10 or greater than 24 breaths per minute were excluded from the study. For HRV analyses, the most stable signal sections were selected, which will include at least 256 consecutive beats.
The analyses were made from linear models in the time domain: RMSSD indices (square root of the square sum of the differences between the iR-R in the record divided by the number of iR-R at a given time minus one), RMSM (root of the sum of the square and the differences of the individual values in relation to the mean value, divided by the number of iR-R of the selected data series) and pNN50 (percentage in relation to the total of normal iR-R, in relation to the previous iR-R, with a difference greater than 50 ms) and in the frequency domain, through spectral analysis: low frequency components (LF), high frequency (HF) in normalized units (un) by the ratio between low and high frequency LF/HF [11,14,15].
Intervention Protocols
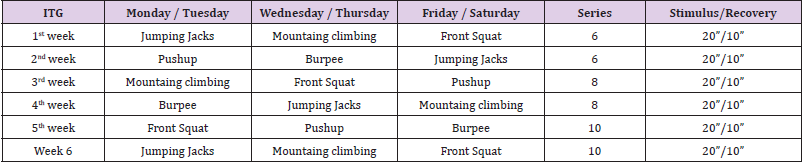
Study participants underwent six weeks of electronically supervised resistance training by GoogleMeet web conferencing platform. The training took place three times a week according to the availability of the participants. The exercises performed by the ITG were: jumping jacks, pushup, mountain climbing, burpee, front squat. Progression occurred every two weeks, increasing two sets every two weeks, as shown in Table 1.
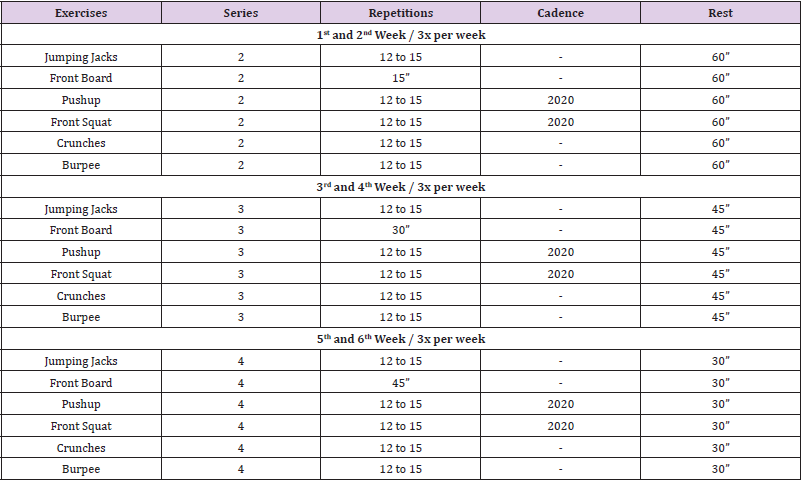
The exercises performed by RTG were: jumping jacks, front board, pushup, front squat, crunches and burpees. The training progression occurred every four sessions (two weeks) and consisted of: first and second week – 2 sets of each exercise with 60’’ interval between each series; third and fourth week - 3 sets of each exercise with 45’’ interval between each series; and finally, fifth and sixth week - 4 sets of each exercise with 30’’ interval between each series, as shown in the tables below, as shown in Table 2.
The Control Group did not perform any exercise, but attended the collection site to perform physiological measurements at the same estimated moments of the experimental protocols. After 3 weeks of protocol it was necessary to make a change only following the exercises performed, starting to be: Polyslipper, Burpee, Squat, Plank, Support and Trunk Flexion. The exchange was performed due to the difficulty of finishing the training protocol.
Statistical Analysis
Data normality was tested using the Shapiro-Wilk test, variance homogeneity was evaluated using the Levene test and boxplot graphs were used to identify significant outliers. Anova oneway was used to confirm homogeneous samples to compare the variables: age, weight, height and BMI.
The variables SDNN, RMSSD, PNN50, VLF%, LF%, LF n.u., HF% and HF n.u. presented a normal distribution, homogeneous variances and absence of significant outliers. The other variables did not present the requirements for parametric tests, which were: RRmedium, HRmedium, HRmin, FRmax, VLF ms², LF ms², HF ms² and the LF/HF ratio. To compare the effects of training in the preand post-intervention moments, the two-way Anova (2x3) was used and when a significant effect of the interventions was identified, Bonferroni’s post hoc was used to identify the differences between means. The Kruskal-Wallis test was used to compare the pre and post values of the nonparametric variables in baseline and after interventions. The Wilcoxon test was used to compare the values of the variables that did not present parametric distribution evaluated in the moments before and after the interventions.
The effect size for the Wilcoxon test was based on the calculation of the rank-biserial correlation (rB). The rB values were classified according to the classification criteria for pearson’s correlation coefficient and, therefore, trivial (rB< 0.10), small (0.10 ≤ rB< 0.30), mean 0.30 ≤ rB<0.50) and wide (rB ≥ 0.50) [16,17]. All analyses were performed in Jeffreys’s Amazing Statistics Program (version 0.12.2, Netherlands). Parametric data were presented as mean (standard deviation) and mean difference (%). Non-parametric data were presented as median (interquartile interval [IIQ]) and median difference). A significance level of 5% was adopted.
Results
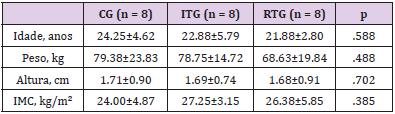
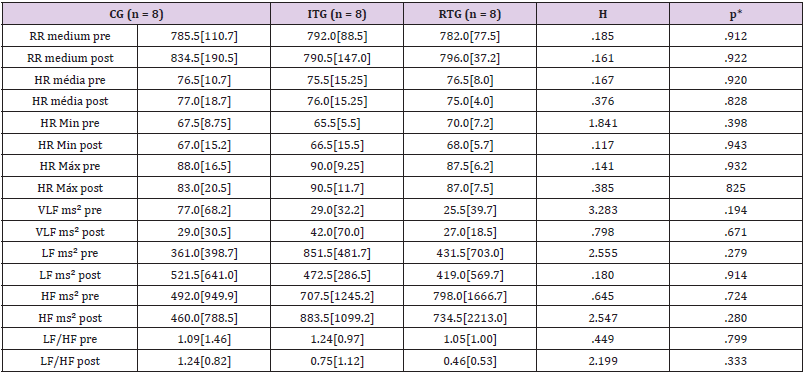
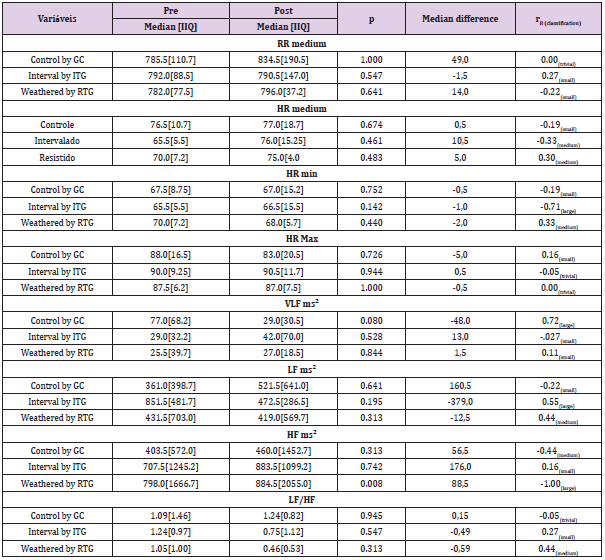
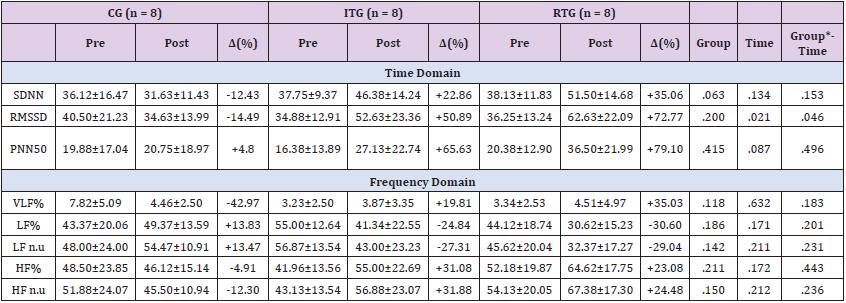
The study included 24 individuals and the sample categorization data are presented in Table 3, with no statistical difference between the variables: age, weight, height, BMI. No significant differences were found (p > 0.05) between CG, ITG and RTG: RRmedium, HRmedia, HRmin, FRmax, VLF ms², LF ms², HF ms² and the LF/HF ratio of the participants both at baseline and after the intervention period, as shown in Table 4. Representing the increase in parasympathetic modulation, the group that performed the intervention with resistance training showed significant improvement in the HF ms² variable (median difference = 88.5; p = 0.008, rB= -1.00 [broad effect], for the other non-parametric variables no statistically significant difference was found, as shown in Table 5. After performing the two-way Anova to compare the parametric variables, a significant effect of time was found for the variable RMSSD [F(1.42) = 5,787; p = 0.021], and for the same variable, group*time interaction was observed [F(2.42) = 3,308; p = 0.046] and after multiple comparisons, the Sidak post-hoc showed that the RTG presented higher values as a function of time (p = 0.006) that showed an increase in parasympathetic modulation with a percentage increase of 72.77% after intervention with resistance training.
Table 3: Characterization of the sample investigated.
Note: CG: Control Group; ITG: Interval Training Group; RTG: Resistance Training Group; n: number of persons; BMI: body mass index.
Table 4: Intergroup comparison of the variables investigated.
Note: CG: Control Group; ITG: Interval Training Group; RTG: Resistance Training Group; n: number of persons; RR: R-R interval; HR: heart rate; VLF: very low-frequency; LF: low frequency; HF: high frequency. H: Kruskal-Wallis h. *P-value from kruskal-wallis test.
Table 5: Comparison between baseline values and after the intervention period for the variables investigated.
Note: CG: Control Group; ITG: Interval Training Group; RTG: Resistance Training Group; n: number of persons; IIQ: interquartile range; rB: rank-biserial correlation ; RR: R-R interval; HR: heart rate; VLF: very low-frequency; LF: low frequency; HF: high frequency. H: Kruskal-Wallis h. *P-value from kruskal-wallis test. *O value from wilcoxon test.
Although the results of the other variables confirm the improvement in cardiac autonomic control, for the groups that performed the two physical exercise protocols, with the increase of the variables representing the parasympathetic modulation PNN50, HF% and HF n.u. (ITG: ↑65.63%, ↑31.08% and ↑31.88%; RTG: ↑79.10%, ↑23.08% and ↑24.48%, respectively) and reduction of indices representing sympathetic modulation LF% and LF n.u. (ITG: ↑24.84% and ↑27.31%; RTG: ↑30.60% and ↑29.04%, respectively) no significant effect of group, time or interaction was observed, as shown in Table 6.
Table 6: Analysis of heart rate variability before and after intervention with tele-monitored exercise.
Note: CG: Control Group; ITG: Interval Training Group; RTG: Resistance Training Group; n: number of persons; SDDN: standard deviation of all normal RR intervals recorded in millisecond, expressed in milliseconds, rMSSD: square root of the mean square differences between normal intervals of adjacent RR, in time interval, expressed in milliseconds; PNN50: percentage of adjacent IRR with duration differences greater than 50 ms; VLF: very low-frequency; LF: low frequency; HF: high frequency.
Discussion
The present study compared and characterized the effects of two different training protocols (Tabata and Resistance Training) on cardiac autonomic modulation of healthy young people. The results indicate that the RTG provided better benefits in relation to the ITG. The recommendation of a minimum of 150 minutes per week of physical activity to avoid sedentary lifestyle and develop healthy habits is predominant throughout the literature [18,19], however, our study demonstrated that 20 to 30 min/day, three times a week, were sufficient to present functional improvements and HRV in healthy young people.
Our findings did not find significant differences in the variables RRmean, HRmedium, HRmin, FRmax, VLF ms², LF ms², HF ms² and the LF/HF ratio in any of the groups, not corroborating the findings of Cardozo et. al., [20] that recorded significant values in the variables LF ms², HF ms² in the groups that performed concentric exercise of the isolated agonist: concentric exercise of the knee extensors, in 3 sets of 10 repetitions, with a velocity of 60°/sec. and recovery interval of 60 seconds and Alternating exercise or superseries: concentric exercise of knee flexors followed, after 10 seconds, of concentric exercise of knee extensors, in 3 sets of 10 repetitions with a speed of 60°/sec. and an interval of 60 seconds between each series, the protocol was performed with an interval of 7 days. It is noteworthy that the intervention time was different in the studies.
Furthermore, the results showed significant improvement in the hf ms² variable (median difference = 88.5; p = 0.008, rB = -1.00 [wide effect] in RTG, impacting on a lower probability of adverse events in sedentary and pathological people, with the practice of exercises performed in domicilium, also pointed out by Lai et. al. [21] that evaluated 32 women aged 55 to 74 years in postmenopausal with coronary artery disease, for 8 weeks, training 3 times a week, were able to obtain similar results with our study.
In a study conducted by Paschoal et.al. [22] that compared cardiac parasympathetic behavior during the recovery phase of an incremental exercise (IE), performed before and after aerobic training program (ED) with 12 sessions, did not provide modification in cardiac parasympathetic modulation in the recovery phase after IE. In our study after the interventions, there was improvement with the increase in the variables that represent parasympathetic modulation, as the main factors that may have interfered in the results, we highlight the total and daily training time and its intensity that were different in the two studies.
Lima [23] analyzed that high values of the variable pNN50 are higher in physically active people, because physical training is able to increase the physiological capacity of the cardiovascular system in varying heart rate and, consequently, better adapt to changes or stimuli of the external environment. Like other studies in the literature, our study improved this variable, confirming the benefit proposed by physical exercise. In our study, we found that the RTG had a significant effect of time for the RMSSD variable and after multiple comparisons, the Sidak post-hoc showed that the RTG presented higher values as a function of time (p = 0.006) which showed an increase in parasympathetic modulation with a percentage increase of 72.77%. Similar to other studies that describe that people with various psychological disorders, anorexia nervosa, hypertensive and other pathologies, have this variable with decreased rates.
Batista et. al., [24] analyzed that the intensity of training and periodized training are predominant factors for changes in autonomic modulation, values such as 80% of VO2 max, were able to increase the parasympathetic activity, associated or not, with decreased sympathetic activity of healthy individuals. In our study, it was possible to verify improvement of parasympathetic activity and decrease in sympathetic activity in ITG and RTG with subjective intensities, taking into account the biological individuality of the groups, in similar intervention periods. Collaborating with our findings in relation to the variables of time and frequency domain of HRV, various authors in their studies, they point out that the higher sympathetic activity and reduced parasympathetic activity, a low HRV, is related to a higher rate of cardiovascular morbidity and mortality and a high HRV reflects on a better health of the cardiovascular system, involving healthy individuals with good function of the autonomic control mechanism.
Due to the current panorama experienced in the world, due to The Covid-19, our study used telemedicine as a strategy to follow the prescribed protocols. Although most studies related to teleexercise are directed to the treatment of pathological groups. Silva et. al., [25] analyzed the Effects of a rehabilitation program on the quality of life of people with Parkinson’s disease, during social isolation in the COVID-19 pandemic, 17 people participated in the program for 3 weeks, the exercise adherence rate remained above 70% throughout the program. It was concluded that people with Parkinson’s disease can obtain improvement in quality of life, even in a period of social isolation.
Despite being a tool focused on pathological groups, recent studies have shown benefits in its use as prevention and guidance of the spread of the disease and way to maintain an exercise routine, which can be aimed at any public. Some limitations of the present study should be recognized. We studied healthy young people and, considering the autonomic modulations presented by people with cardiovascular diseases, their adaptations before, during and after exercise may be different in relation to healthy individuals, so the results of the present study may not be applicable in individuals with pathological conditions, since age is also a variable that influences all parameters.
Further studies should be conducted in larger, healthy and patient populations to analyze new ways of prescribing for different specificities. Another important point is that the study was conducted using only body weight and without any other equipment, therefore, different responses may differ if other forms of exercise were used (running on track, treadmill, bicycles).
Conclusion
The RTG promoted significant improvement in the variables HF ms² and RMSSD, although in the other variables the two protocols were beneficial, the results suggest that Resistance Training may be a viable tool for training programs for healthy young people. The proposal of telemonitoring had a good support of the participants and was able to be effective in the application of training protocols, confirming that it is a viable alternative to combat sedentary lifestyle or assist in the control of pathologies of people who are in isolation due to Covid-19 or lack of resources to go to the places of medical care.
Although few studies include the use of tele monitoring for the prescription of physical exercises for both sedentary and pathological audiences, it was possible to identify advantages in its use in our study, due to zero financial cost, adaptation of participants to technology, flexible schedules for training, besides being crucial for avoiding physical contact, a predominant factor due to the pandemic experienced today.



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.