My Therapy Concept from 25 Years of Experience in Dental Sleep Medicine
Introduction
My therapy concept is based on the idea of using three highly precise aids, that exhibit very little redundancies. The combination of these aids yields a significant increase in quality, effectiveness, and efficiency of the entire treatment process. The aids I am referencing here can be split into three separate solutions: first the vector diagram as a framework, secondly the JS-Gauge® as an instrument and thirdly the F-UPS® as MAD (mandibular advancement device). In our clinic, the combination of these aids has significantly reduced laboratory and treatment times and increased our patients’ satisfaction.
Risk Profiling (Vector Diagram)
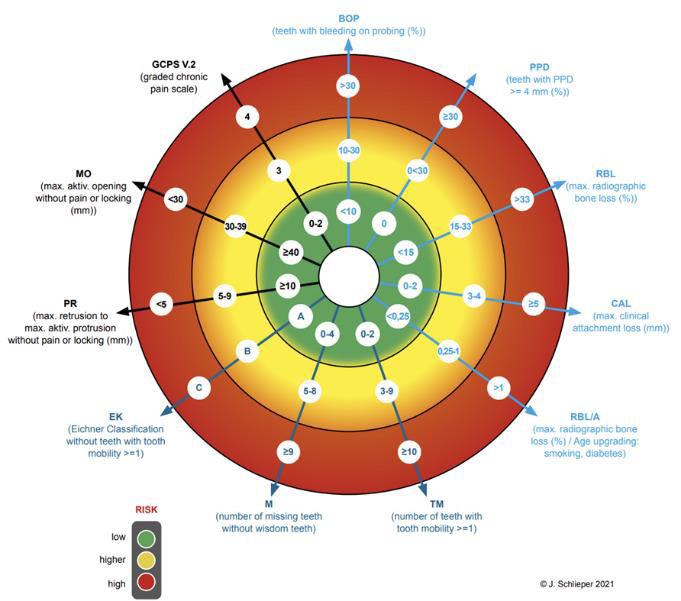
Both at the beginning and throughout the MAD therapy [1,2] it is critical to measure specific indicators to help guide decisionmaking. Thus, we can effectively weigh risks and opportunities of the MAD therapy against one another and craft an effective treatment plan. A comprehensive and tailored risk profiling [3] is a viable solution here and creating a framework to standardize the process of identifying these so-called predictors can greatly increase efficiency [4]. Said framework which i developed can be seen in Figure 1 in the form of a vector diagram, which allows us to visually compose a risk profile for each patient. This visual representation further allows for a swift comparison between consecutive risk assessments, to allow for the evaluation of progress throughout the treatment [5]. The predictor values are segmented into three risk groups and color-coded via a traffic light system (red: high risk; yellow: moderate risk; green: low risk).
Utilizing this visual aid allows for a quicker assessment that can be intuitively grasped by both the practitioner and the patient. This not only facilitates the interdisciplinary decision-making between the dentist and sleep specialist, but also aids the dentist with educating the patient, thus also informing the patient’s decisionmaking process. Moreover, the vector diagram helps guide the therapeutic decision-making throughout the entire MAD therapy. Therefore, the framework helps to both optimize the starting conditions for the MAD therapy and reduces the risks throughout the therapy. However, this diagram is not intended for the precise recording of all dental parameters. Nor shall it be used to assess the quality of oral health overall. The diagram’s intention is to primarily increase the quality, effectiveness, and efficiency of the therapeutic decision-making process for MAD. Above all, it aims to lay the foundation for treating large patient populations and thus making it a viable tool for the use with public health insurance providers. The risk assessment covered by the vector diagram spans the three areas of biological, mechanical, and functional values of the stomatognathic system.
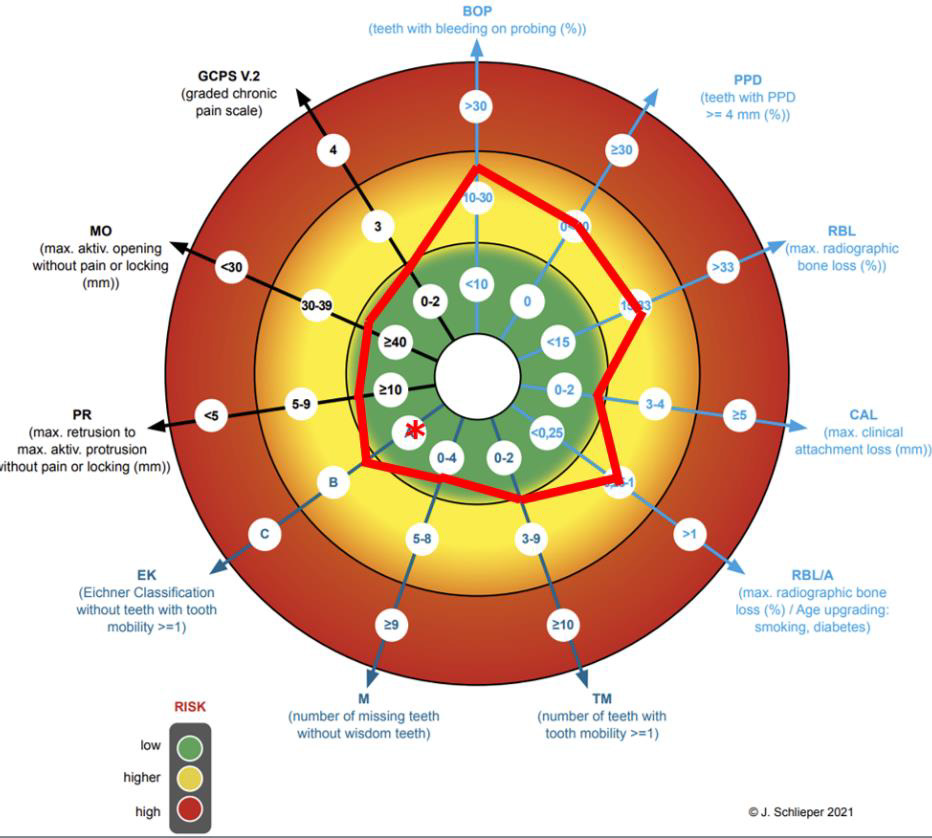
The biological area relates to periodontics [6], the mechanical area to prosthetics [7] and the functional one to the function [8]. The vectors and the labelling of these 3 areas are shown with different colors light blue, dark blue and black for better visual differentiation. The collected values are marked in the diagram, either with its value in the given selection or scaled on the vector ray. This makes it easier to identify minor changes during a followup. The line connection results in the individual biological risk profile for the MAD therapy. The mechanically relevant findings for tooth loosening, the number of teeth and the profile of the support according to the Eichner classification are also collected. The Eichner classification is subdivided into the profile of the dental or implant logical support and the profile of the occlusal support. The Eichner classification is basically only a classification of the gap dentition according to the profile of the dental support zones intended for prosthetic therapy. However, this classification is not sufficient here for the risk analysis in MAD therapy. In the vector diagram, this classification is therefore further subdivided into a dental and implantological support zone profile without prosthetic gap closure, as well as the occlusal support zone profile at the time of the examination, possibly with prosthetic gap closure. The dental classification is marked without, while the occlusal classification is marked with an asterisk in the vector diagram (Figure 2).
Finally, the 3 relevant functional findings, which include active degree of protrusion, active degree of mouth opening and the graded chronic facial pain after DC/TMD need to be assessed. The active degree of protrusion is measured from the maximum retrusion into the maximum protrusion in the lying position after three attempts. In my opinion and in the opinion of many other colleagues, this is the most precise measurement method. Only values that can be achieved without locking of the jaw or pain are measured. The same procedure is used to measure the active mouth opening. Finally, the GCPS grade is entered from the assessment of the corresponding questionnaire according to DC/TMD, which completes the creation of the risk profile for the function. In (Figure 2) you can see an example of a fully completed primary assessment.
Adjustment and registration with bite gauges (JS-Gauge®)
Once the decision for or against MAD therapy and for or against preparatory measures has been made and these have been completed, the second, most important treatment step follows: the adjustment and registration of the starting position, which is critical to produce a MAD [2].
From January 1, 2022, onwards the MAD therapy will be covered by public health insurance in Germany and the requirements to receive the needed coverage include an individual three-dimensional registration of the starting position [9]. This registration must be tailored to the individual circumstances of the patient as well as to the individual design of the MAD that is to be used. Bite gauges are used as aids for this [10,11]. They offer the advantage of flexible adjustments under functional, neuromuscular conditions when compared to the use of no bite gauge or the axiographs. All bite gauges currently on the market neither fully nor ideally meet these requirements. Bite gauges, which are held between the rows of teeth by the patient biting down, are subject to variability during adjustment and registration, which reduces precision. The precision can be increased considerably by securely fixing the bite gauge to the upper jaw [12]. A bite spoon is fixed to the upper jaw with A-silicone and the lower jaw is supported by means of a support pin registry.
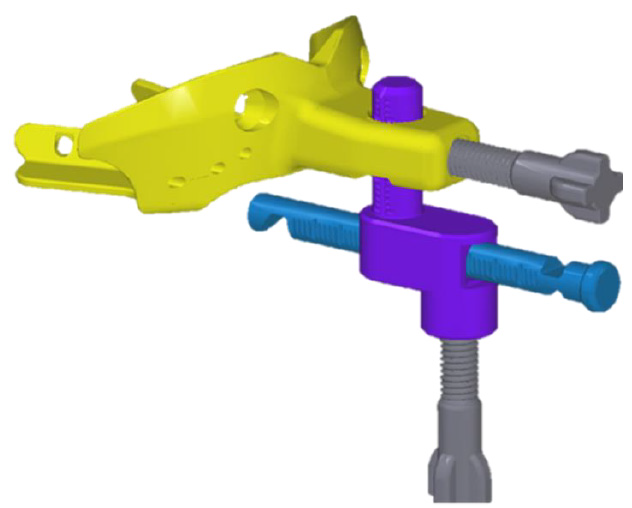
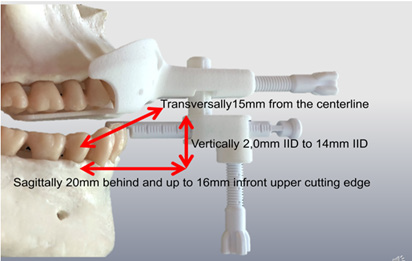
This allows for more comfort due to a relaxed jaw, interferencefree adjustments and a registration in the lying treatment position without a forced bite. The JS-Gauge® (Figure 3) which i developed consists of the bite spoon, in yellow, the vertical pin, here in turquoise, and the horizontal pin, marked in blue, as well as two fixing screws, colored gray. A standout feature of the JS-Gauge® is that it can be continuously adjusted in all three spatial dimensions sagittally, vertically and transversely. The support of the horizontal pin on the tooth edges of the mandibular incisors, can be continuously adapted for a safe adjustment of the mandible on the JS-Gauge®. The adjustment and registration range (Figure 4) extends sagittally from 20 mm behind and up to 16 mm in front of the upper edge of the incisor. A vertical bite lock can be set from 2,0 mm IID to approx. 14 mm IID. Transversally, the JS-Gauge® allows adjustment 15 mm from the centerline. This transversal adjustment should also be adjusted habitually in a lying position without functional symptoms occurring. We want the patient to be as relaxed as possible.
The adjustment with the bite gauge should be tailored to the individual patient’s situation and the design of the MAD [13,14]. With increasing bite blockage with the same protrusion, which can be measured as inter incisor distance (IID) in relation to the upper jaw, the load on the craniomandibular system increases [15]. We can gather from this that the percentage of the same protrusion in relation to the maximum protrusion increases with increasing bite blockage [16]. In this respect, registration with bite gauges should be carried out with as little bite blockage as the bite conditions, the functional findings and the MAD Design allows. The protrusion should be adjusted from the maximum retrusion to approx. 5 mm in the comfort zone of the patient. I recommend a 5 - 10 minute control of this position with regard to the functional findings and the comfort findings of the patient. The 3D adjustment of the starting position is complete if no pathological functional findings occur, and the patient does not complain about discomfort within 5-10 minutes (Figure 5). After use, the JS-Gauge® is reprocessed with the help of the tray and the box. The reprocessing meets the requirements of the MDR (Medical Device Regulation, EU 2017/745) in all stages.
MAD (F-UPS®)
From this starting position, sleep medical titration continues after the MAD has been inserted [2,9]. In order to be able to achieve the lowest possible bite blockage, especially in patients with a deep bite or a flat Spee curve, I developed a MAD (H-UPS®) as early as 1997 [17] that enables this. This leaves the front teeth mostly free. This makes the plastic construction more unstable, yet this instability is absorbed by a steel arch to which the Herbst hinges are attached by laser welding. Although this construction has many advantages, the disadvantage is the mechanics of the Herbst hinge. As every time the patient opens his mouth during the night, a retrusion occurs, frontal elastic bands are intended to prevent this but unfortunately cannot do so completely. If the Herbst telescope is mounted on the MAD in reverse, unphysiological stresses arise on both the MAD and the dental arches as well as on the craniomandibular system when the mouth is opened. Therefore, no desired physiological conditions can be achieved. Inclined planes attached to the side also do not allow a physiological opening of the mouth and do not reliably prevent an opening of the mouth. Frontal elastics are also required here. As we can see all these approaches are at least somewhat flawed.
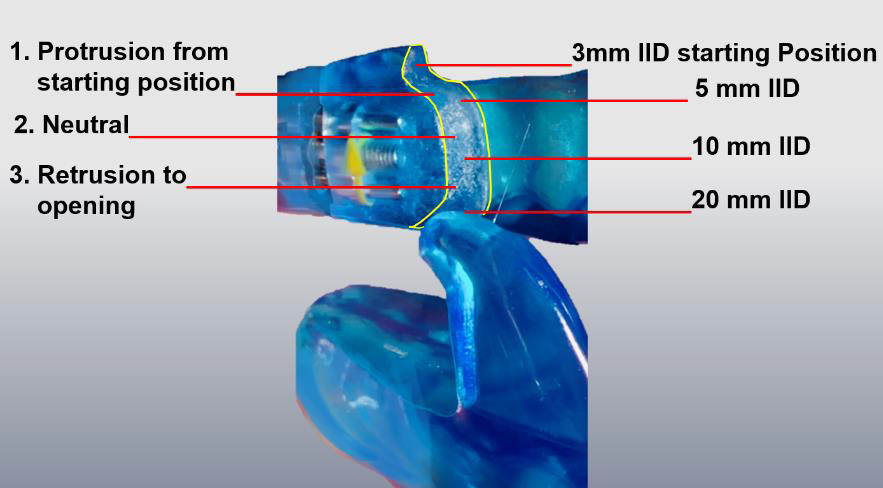
In my opinion, the solution lies in the fin-like design with the lateral guide elements. I developed a MAD (F-UPS®) in 2018 (Figure 6) that enables this. With these it is possible for the typically mouth openings up to 10 mm IID [18] to physiologically occur during sleep without retrusion, which constitutes a physical adjustment of the guide way of the lateral elements without any loss of effectiveness of the MAD. The guide way of the lateral elements is divided into three parts (Figure 7). From the starting position, the first part starts with a jaw opening with a protrusion movement of up to approx. 5 mm. The protrusion is intended to reflexively prevent the number of further jaw openings with a larger IID during sleep. If there is still another jaw opening, the second part of the movement follows with a jaw opening with unchanged protrusion up to 10 mm IID. Only from 10 mm IID, which normally does not occur during sleep [18], is 3. the further jaw opening with retrusion up to the disconnection of the two splint parts with release for maximum jaw opening. The fins of the F-UPS® are not made separately. In this design, the upper and lower jaw splints are CAD designed and milled from a single block. This is the only way to produce the F-UPS® with this fin design for an optimized function without retrusion and with the ideal recess in the anterior tooth area for the least possible bite blockage with very high stability.
Optionally, this sagittal guideway of the lateral elements can be made more precise from the starting position by a further registration in 10 mm IID to be able to shape the guideways transversely. This is e. g. recommended if the jaw opening-path shows a lateral deviation. For this purpose, after the first registration of the starting position, the sagittal, vertical, and transversal setting values are adopted from the JS-Gauge® the IID setting is increased to 10 mm and readjusted, if necessary, according to functional aspects. After frontal and lateral coating with A-silicone, the JSGauge ® is removed. This procedure is possible because the jaw relation can be transferred from a first registration to the second registration by adopting the 3D setting values of the JS-Gauge®. It is therefore not necessary to keep registrations for later new MAD productions. Knowledge of the 3D setting values of the JS gauge is sufficient for this.
Conclusion
During the development of these three aids, the treatment of my patients has steadily improved and due to the use of these aids in conjunction with each other the treatment quality has improved yet again.
For more Articles on: https://biomedres01.blogspot.com/





No comments:
Post a Comment
Note: Only a member of this blog may post a comment.