Gastrointestinal Manifestations in Adult Patients Presenting with Dengue Infection, A Local Study from Tertiary Care Hospital
Introduction
Dengue infection is a common disease of tropical and subtropical regions caused by mosquitoes. It is characterized by fever, headache, arthralgia, joint and muscle pain. Occasionally, patients develop abdominal and gastrointestinal symptoms, but little information exists regarding presence of these manifestations. May be asymptomatic or produce Dengue Fever (DF) and Dengue Haemorrhagic Fever or Dengue Shock Syndrome (DHF/DSS). Antigenically related four but distinct viruses, DEN 1, DEN 2, DEN 3, and DEN 4, are considered as aetiological agents of DF1.More than 2.5 billion people reside in areas that may be at risk for dengue infection [1]. It is estimated that each year 50-100 million cases of dengue fever occur out of which the potentially fatal Dengue Haemorrhagic Fever (DHF) constitutes up to half a million cases [2]. The DENV has been endemic for many years in Pakistan because of the temperate climate of the country. Many outbreaks of Dengue infection have been reported since 2006 every year with multiple serotypes [3]. Such outbreaks are primarily because of the vast agriculture land, rich fauna, water reservoirs for power generation, open irrigation channels and floods because of heavy rainfall provides very suitable sites for the breeding of the mosquitoes.
Dengue infection can present with, high grade fever accompanied by any of the following: chilliness, severe muscle ache (one synonym of dengue is “break-bone fever”),retro-orbital pain, photophobia, backache, joint ache and nausea, vomiting, abdominal pain. High fever may be sustained over 5-6 days. Other signs and symptoms include a generalized maculopapular rash, lymph node enlargement, hepatosplenomegaly, a positive tourniquet test, petechiae, and other hemorrhagic manifestations, such as epistaxis and gastrointestinal bleeding. In few cases, common cold and flu like symptoms initially occurred. Convalescence mostly occurs spontaneously and abruptly, but sometimes it may takes several weeks, and accompanied by pronounced asthenia and depression. In DHF , the overall vascular system is damaged, vascular instability, decreased vascular integrity and platelet dysfunction leading to bleeding from many different sites [4]. Although liver is not the main target organ of this infection, but there are cases where histopathological findings, Centro tubular necrosis, fatty alterations, Kupffer cells hyperplasia, acidophilic bodies and monocytic infiltrates of the portal tract, have been detected in patients of Dengue Hemorrhagic Fever (DHF) and Dengue Shock Syndrome (DSS).
The viral disease is self-limited but hepatic insufficiency can occur in some patients [5]. Gastrointestinal different presentations of dengue are acute hepatitis, acute severe liver injury, fulminant hepatic failure, acalculous cholecystitis, acute pancreatitis, acute parotitis and febrile diarrhoea. In Dengue endemic area, any patient presenting with fever and acute abdomen should be evaluated for dengue fever and dengue‐related acute acalculous cholecystitis, acute pancreatitis [6]. Possible mechanisms proposed are direct invasion of the virus into pancreatic cells, damage secondary to shock (hemorrhagic or vasodilatory) and thrombocytopenia, edema of the ampulla of Vater and rarely autoimmune response generated to dengue virus antigen [7-10]. The aim of our study is to evaluate the spectrum of gastrointestinal manifestations in patients presenting with dengue infection depending upon the severity of infection.
Materials and Methods
The study was conducted at Benazir Bhutto Hospital during last epidemic of Dengue infection in Rawalpindi. It was prospective study conducted from August 2019 to November 2019. 100 patients were enrolled with consecutive sample.
Inclusion Criteria
Patients age > 13 years
Patients with NS1, IgM positive or IgG fourfold rise
Exclusion Criteria
• Patients with established decompensated chronic liver disease.
• Patients with diagnosis of acute pancreatitis or cholangitis.
• Patients with cholelithiasis or cholecystectomy.
• Patients having duration of fever more than 14 days.
Patients admitted were diagnosed dengue infection on the basis of NS1 antigen and IgM antibody or a fourfold rise in titres of IgG. Patients were classified in simple Dengue Fever, Dengue hemorrhagic fever and Dengue shock syndrome based upon the WHO classification. Information were collected and detailed history was taken using pre-formed proforma and relevant investigations for Gastrointestinal manifestations were sent and recorded .
Statistical Analysis
Data was entered and analysed using SPSS v22. Frequencies and percentages were calculated for gender, age groups, disease nature (simple DF, DHF and DSS), dengue serology, gastrointestinal symptoms, and atypical GI manifestations. Patients were divided into 3 age groups: 13-35 years, 35-60 years and >60 years. The values of serum ALT, AST and Bilirubin levels were documented. Test of significance was applied for ALT, AST and bilirubin levels and atypical GI manifestations like acalculous cholecystitis, acute pancreatitis, GI bleed, Fulminant hepatitis/severe acute liver injury to find out if they have any relationship with the severity of dengue infection(as shown by spectrum). A P value of <0.05 was considered as statistically significant.
Results
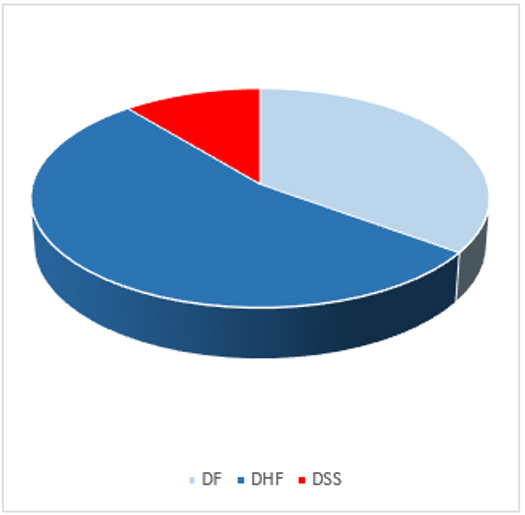
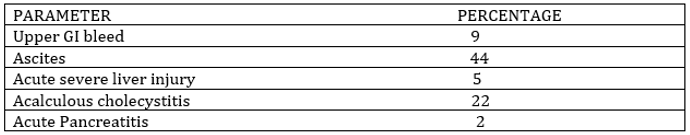
Total 100 patients were included in the study. The age distribution was between 13-72 years and 58 % were males and 42% female patients. Among these, 35% patients have dengue fever, 54% with dengue hemorrhagic fever and 11% had dengue shock syndrome. GI manifestations were present in all patients. Among them, nausea was in 89%, vomiting in 55%, abdominal pain in 59%, GI bleed in 9%, ascites in 44%, hepatomegaly in 14%, diarrhea in 18%, acalculous cholecystitis in 22% cute severe liver injury in 5% and acute pancreatitis in 2%. Either ALT, AST or bilirubin levels were raised in all patients. GI manifestations like abdominal pain, ascites, hepatomegaly, acute severe liver injury, acalculous cholecystitis, and acute pancreatitis were correlated with severity of dengue infection. There was a significant relationship between ALT and AST elevation and severity of dengue infection (p value 0.002 and 0.002 respectively, however, there was no significant relationship between bilirubin rise and severity of disease (Figures 1 & 2).
Discussion
Dengue fever usually presents as an acute febrile illness with musculoskeletal pain, and petechial rash. Atypical manifestations also known as expanded dengue syndrome is not uncommon. It may present as acute abdomen leading to diagnostic dilemma. In our study, all patients have various GI manifestations which included typical manifestations such as nausea, abdominal pain, vomiting, hepatomegaly, diarrhea and atypical gastrointestinal manifestations like acute pancreatitis, acalculous cholecystitis, ascites, acute severe liver injury and gastrointestinal bleed. In previous study, common GI manifestations noted were Nausea (43.3%), vomiting (40.2%), pain abdomen (41.3%), dyspepsia (32%) and loose stools (12%) [11] but in our study GI symptoms were found in a greater number of patients. Acalculous cholecysitis was confirmed on ultrasound (Gallbladder wall thickness>5mm and inflammation without gallstones) along with clinically tender upper abdomen and sonologically and clinically positive murphy’s , with pericholecysytic fluid and no ascites was found in 22 % of the patients in our study. In a previous study significant correlation of acalculous cholecystitis with severity of dengue fever was seen [12]. Acute pancreatitis was found in 2% of the patients with dengue shock syndrome in our study. Pancreatitis was confirmed by specifically raised serum amylase and lipase in the absence of other known causes of pancreatitis. Characteristic abdominal pain of acute pancreatitis was not observed in our patients. Abdominal pain in patients with dengue fever secondary to acute pancreatitis was found [13]. In a study conducted in Karachi, pattern of liver damage and relation of AST /ALT elevation with severity of dengue and its complications was observed [14].
Acute severe liver injury was found in 5 % of the patients in our study. The cause of liver injury in DI remains unclear. Liver cells may be damaged through one or more of the following mechanisms:
(i) Direct cytopathic effect of the virus
(ii) Killing of virus-infected cells by the host immune response
(iii) A non-specific effect of shock and hypotension [15].
In recent years, dengue-specific CD4+ and CD8+ T-cells have been shown to play a part in the pathogenesis of severe forms of DI occurrence of more severe liver injury in patients with complicated dengue may thus suggest a role for host immune responses in the causation of liver injury as well [16]. Ascites was found in 44% of the patients in our study, these patients had clinically DHF III / IV classification of disease severity. Patients having ascites due to other causes such as chronic liver disease were excluded from the study. Sonographic findings included pleural effusion in 21 patients (53%), thickening of the gallbladder wall in 17 (43%), and mild ascites in 6 (15%) [17]. Hepatomegaly was present in 14 % of the patients with dengue fever confirmed upon ultrasound with a liver span of between 14-18 cm in our patients all the patients had deranged liver function test and a clinically severe dengue syndrome. GI bleed was found in 9% of the patient, endoscopy was done to evaluate the cause of the GI bleed, patients having variceal bleed were excluded. Among our patients the prominent endoscopic findings were gastric erosions and ulceration. Patients were managed conservatively with high dose PPI and blood products as required. None of the patients received aspirin, nonsteroidal anti-inflammatory drugs or steroids before or during hospital stay. Upper GI bleed manifestoed as haemetemesis in 2% of the patients and malena in the remaining 7%.
In a study conducted, hemorrhagic(and/or erosive gastritis) was the most common finding in patients (67.0%), followed by gastric ulcer (57.7%),duodenal ulcer (26.8%), and esophageal ulcer (3.1%). There was no significant difference in histories of peptic ulcer disease between the ulcer and non-ulcer groups. Of the 73 patients with peptic ulcer, 42 (57.5%) had endoscopic findings that met the criteria of recent hemorrhage [18].
Of these GI manifestations atypical presentations like hepatomegaly, fulminant hepatitis, acute pancreatitis, ascites acalculous cholecystitis and abdominal pain correlated with the severity of dengue fever. In another study conducted abdominal pain and tenderness, gastrointestinal bleed, jaundice and hepatomegaly were all predictors for need of intensive care. Signs of plasma leakage such as ascites and pleural effusion, as expected, were also predictors of serious disease that needed intensive care. Symptoms of nausea and vomiting, though very common, were not associated with serious disease [19].
Conclusion
our study revealed high frequency of gastrointestinal symptoms in patients with dengue fever. These GI manifestations were significantly more frequent in patients who were admitted in hospital, this indicates a strong correlation of gastrointestinal symptoms with the severity of dengue infection and their presence should be considered by decision making health authorities for better patients management. The differential diagnosis of an acute febrile syndrome with abdominal pain or atypical gastrointestinal symptoms in patients living in endemic areas should include dengue infection.
For more Articles on: https://biomedres01.blogspot.com/



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.