Analgesic Nephropathy: A Silent Killer
Introduction
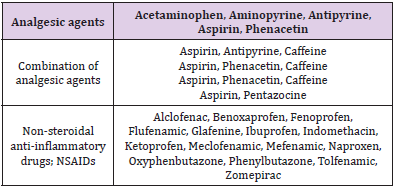
As early as 1950, in a number of European countries, Analgesic Nephropathy (AN) was found to be a highly prevalent renal problem [1]. Formerly considered one of the common causes of End-Stage Kidney Disease (ESKD), a marked decline in the prevalence and incidence of AN in recent decades has occurred. At its peak in the 1980s, AN accounted for 15% to 20% of cases of ESKD but presently, has fallen to approximately 1% in Western countries. Phenacetin was introduced as an analgesic in 1887. Phenacetin, which is metabolized to acetaminophen, was popular due to its long duration of action and its analgesic effect. Phenacetin withdrawal occurred worldwide roughly between 1960 and 1980. Historical epidemiologic data identified a close correlation between AN prevalence and phenacetin. Numerous observational publications, primarily from Australia and Europe, have demonstrated a sharp decrease in AN incidence coinciding with the withdrawal of phenacetin mixtures [2]. AN is a disease resulting from the habitual consumption over several years of a mixture containing at least two antipyretic analgesics usually combined with either codeine or caffeine. It is characterized by renal papillary necrosis and chronic interstitial nephritis, which leads to the insidious onset of progressive renal failure or as a result of urothelial carcinoma [3,4]. Patients are usually females between the ages of 30 and 65 years with a history of analgesic consumption for 5 to 20 years before development of renal injury [5]. Several compounds appear to be correlated with AN. Classic AN was associated with the following combinations:
(1) aspirin and acetaminophen,
(2) aspirin and a pyrazolone, and
(3) acetaminophen and a pyrazolone, all three of which were combined with caffeine, codeine, or both [4].
Pathophysiology
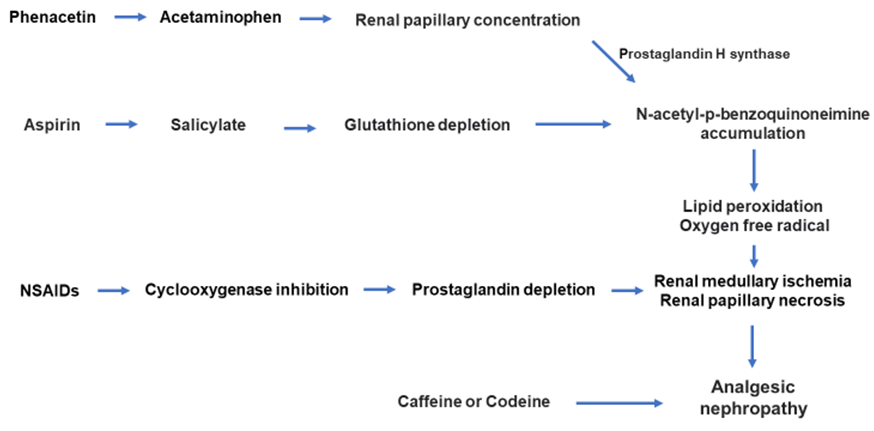
AN is characterized by renal papillary necrosis and chronic interstitial nephritis. The renal injury due to analgesics is mainly in the renal medulla and constitutes ischemic necrosis of the papillae because of reduced blood supply in medullary tissue. Phenacetin is metabolized into acetaminophen, which then undergoes metabolic activation to a reactive radical, N-acetyl-p-benzoquinoneimine (NAPQI), which causes lipid peroxidation that can lead to cell injury. As a result of countercurrent mechanisms, the maximum accumulation of the metabolites occurs in the renal medulla, causing the initial injury to the papillary tip. Acetaminophen undergoes oxidative metabolism by prostaglandin H synthase to form reactive intermediates. These intermediates are detoxified via conjugation with glutathione. If acetaminophen is consumed alone, the glutathione in the papillae is enough to detoxify the reactive intermediates. If acetaminophen is ingested with aspirin, the aspirin is converted to salicylate, which depletes glutathione in both the cortex and papillae of the kidney, causing the reactive intermediates to damage the renal papillae via lipid peroxidation of tissues in addition to NSAID-induced insult at the cellular level from inhibition of the prostaglandin synthesis pathway. Inhibition of the vasodilatory effect of prostaglandins is the most recognized and accepted mechanism of hypoperfusion-related medullary ischemia, which is generally accompanied by papillary damage in the form of necrosis in most cases [6-8].
Clinical Presentation
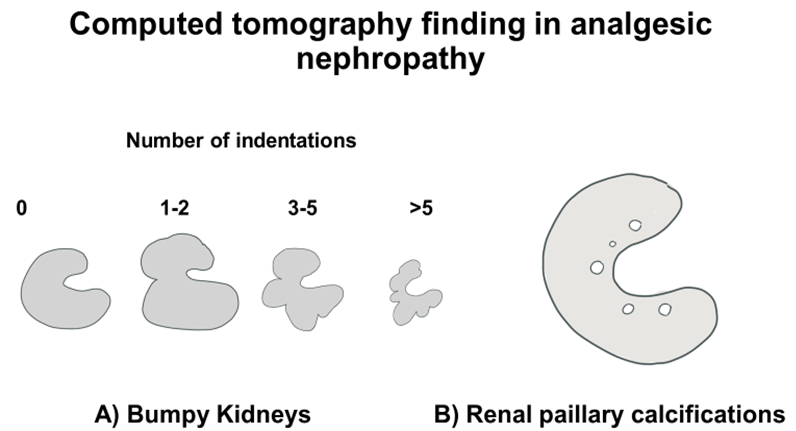
Figure 2: CT imaging criteria used to diagnose AN. Bumpy contours are considered to be present if at least three indentations are evident (panel A). CT can also reveal papillary calcification (panel B).
AN can be difficult to diagnose as the disease has nonspecific symptoms and signs and progresses slowly. Patients are most commonly middle-aged females. In the early phase, nocturia and frequent urination occur because of abnormal renal concentrating capability. Many patients have pyuria and/or symptoms of cystitis due to chronic interstitial nephritis and 25%–85% of patients present flank pain due to calyceal or ureteral obstruction by sloughed papillae. In the chronic phase, many patients develop worsening renal function, hypertension, abnormal proteinuria, and anemia disproportionate to the degree of azotemia. Hematuria, if persistent, should raise the possibility of an underlying uroepithelial tumor [9] (Figures 1 & 2).
Diagnosis
Basic investigations include routine serum studies with a complete metabolic profile and complete blood count. An ultrasound of the abdomen, especially of the kidneys and the urinary bladder, can be useful in ruling out other causes of nephropathy, such as obstruction or infection. A non-contrast abdominal computed tomography (CT) scan is useful for diagnosing this problem. In advanced stages, partial or total papillary necrosis with calcification is demonstrated in 25%–40% of patients, which can be demonstrated on a non-contrast CT scan. Elseviers et al. described CT findings of a small kidney (sensitivity 95%, specificity 10%) with an irregular or bumpy outline (sensitivity 50%, specificity 90%) and medullary calcification (sensitivity 87%, specificity 97%) with renal impairment and background history of analgesic intake suggestive of AN [4].
Management
Table 1: Analgesics, NSAIDs and other drugs and chemicals implicated with causing analgesic nephropathy.
AN is one of the few preventable causes of CKD, and early cessation of NSAIDs can prevent progression of AN. In those with a mild reduction in glomerular filtration rate cessation of NSAIDs prevented further decline in the glomerular filtration rate (GFR). Adequate hydration is essential in the early stages of the disease to achieve restoration of blood perfusion even in normotensive patients. Treatment of infections, especially pyelonephritis, is necessary to prevent any further deterioration. The clinical course of this disease is variable and depends mainly on the extent of renal damage, scarring, and fibrosis at the time of diagnosis along with the reversibility of the parenchymal injury (Table 1).
Conclusion
AN develops due to habitual consumption of combination of analgesics mixture and is characterized by renal papillary necrosis and chronic interstitial nephritis. Although the prevalence of AN is decreasing, AN still remains an important and preventable cause of ESKD, especially in the developing countries in which combination pills are still being manufactured and sold.
For more Articles on: https://biomedres01.blogspot.com/



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.