Bilateral Carotid-Cavernous Fistula: A Case Report and Literature
Case Report
We report a case of bilateral carotid-cavernous fistula CF) in a 72-year-old woman who presented with headache and double vision. After diagnosis and treatment in several hospitals, the patient came to our hospital an-accepted cerebral arteriography. It turned to be bilateral CCF and the patient recovered by interventional embolization. This case suggests that the possibility of CCF should be considered in patients with headache accompanied by diplopia. CCF is an abnormal communication between arteries and veins in the cavernous sinus, which can be divided into four types. Type A is the direct communication be-tween the main trunk of the internal carotid artery and the cavernous sinus; Type B is the communication be-tween the internal carotid artery branch and the cavernous sinus; Type C is the communication between the external carotid artery and the cavernous sinus through the Dural branch; Type D is the branch of the internal carotid artery and the external carotid artery communicating with the cavernous sinus at the same time [1]. According to pathology and treatment, CCF can be divided into direct type (type A), indirect type (type B, C or D), mixed type (including direct type and indirect type).
Due to the complex structure of the cavernous sinus, the clinical manifestations of CCF are not specific. As a result, patients with this disease may go to ophthalmology, neurology, otolaryngology, and neurosurgery. Misdiagnosing is likely to occur, which affects the timely diagnosis and treatment of patients. According to the characteristics of blood flow and hemdnamic disorders, CCF can be divided into the high-flow fistula and low-flow fistula, of which the direct type is mostly high-flow fistula, and the indirect type is mostly low-flow fistula [2]. Indirect CCF is usually unilateral, and bilateral is very rare [3-5]. We report a case of bilateral low-flow fistula with a long history of chronic progressive exacerbation. 6 months before admission, the patient developed left migraine headache without obvious inducement, which was a persistent dull pain, not serious, and she did not pay attention to it. She took analgesic by herself and relieved slightly. Four months before admission, the patient developed double vision with dizziness, accompanied by eyes pain, especially the left eye, and blurred vision of both eyes. The dizziness symptom improved after opening eyes. First she went to ophthalmology department of a certain hospital and ruled out ophthalmological diseases. Then she went to neurology department as advised. She took head magnetic resonance imaging, and it is normal.
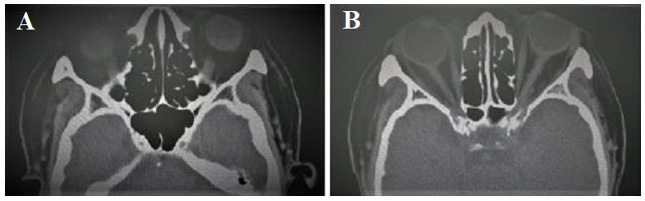
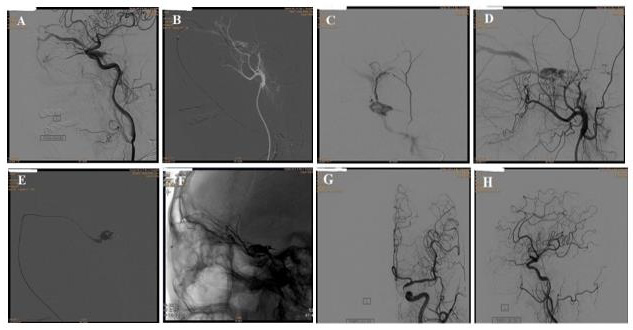
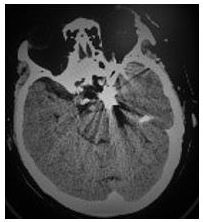
Thus she was diagnosed as “diabetic oculomotor nerve injury”. She was given methylprednisolone and vitamin B. But there was no relief. A few days later, she went to the neurological clinic of another hospital. The doctor considered the possibility of painful ophthalmoplegia and recommended hospitalization. The patient was hospitalized for more than 20 days and was given intravenous hormone, neurotrophic drug, acupuncture and other treatments, but the symptoms were further aggravated, so she came to our hospital. She had diabetes for 3 months, lacunar infarction for 10 years, aortic valve replacement for more than 10 years, no history of infectious diseases, no food and drug allergy history, no positive family history and genetic history. On physical examination consciousness is normal, fluent in speech, the left eyeball is slightly protruding , bulbar conjunctiva hyperemia and edema, bilateral pupils are round but not equal, left: right=5.0:3.0mm, the right eye has direct and indirect light reflection, the left eye has weak direct and indirect light reflection, binocular vision decreased, diplopia, the left eye is relatively fixed, the addiction and abduction of the right eye are slightly restricted, no vascular murmur of periorbital auscultation, no eyeball pulsing, distribution area of the first branch of the left trigeminal nerve is hyperalgesia. Ophthalmic testing shows visual acuity is 20/40 OD and 20/133 OS, left eye lens cloudy, light color of optic disc, right eye lens turbidity, blurred fundus, intraocular pressure 14/15mmHg. Orbital CT scan shows bilateral eyeballs are protruding, bilateral medial rectus muscles are slightly thickened (Figure 1).
Figure 1: Orbital CT: bilateral eyeballs protruding and bilateral medial rectus muscles slightly thickened A and B.
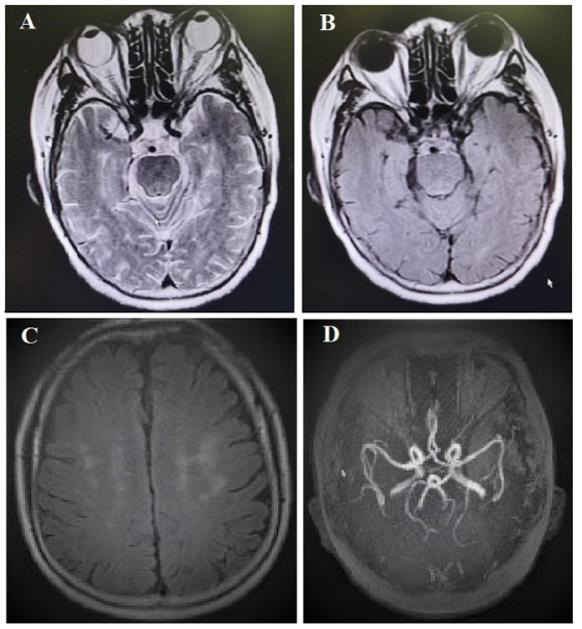
Figure 2: Head MRI: no diffusion-limited signal is seen, long T2 signal of subcortical white matter can be seen on T2-weighted (A) and T2 flair imaging (B and C), and multiple localized vascular stenosis(D).
Head MRI scan: No diffusion-limited signal was seen, long T2 signal of subcortical white matter can be seen on T2-weighted imaging and T2 flair imaging, and multiple localized vascular stenosis (Figure 2). Head MRV: No obvious abnormalities (Figure 3). Related laboratory examination show: no obvious abnormalities in blood cell analysis, urinalysis, biochemical series, immune-related assay, and tumor series. Blood sugar is slightly higher, white blood cells can be seen in urinalysis. The preliminary clinical diagnosis cavernous sinus syndrome (reason to be determined) and diabetes. Because the patient did not improve according to the treatment of diabetic cranial nerve injury and painful ophthalmoplegia, and the patient did not have the common infectious factors of cavernous sinus thrombosis and the characteristics of acute onset and rapid progression, but showed a chronic progression combined with physical ex-amination of cavernous sinus injury and visual impairment. Although the patient did not have typical pulsating exophthalmos and arterial murmurs around the eyes, we still considered the possibility of cavernous sinus fistula and performed digital sub-traction angiography (DSA) after neurosurgery consultation.
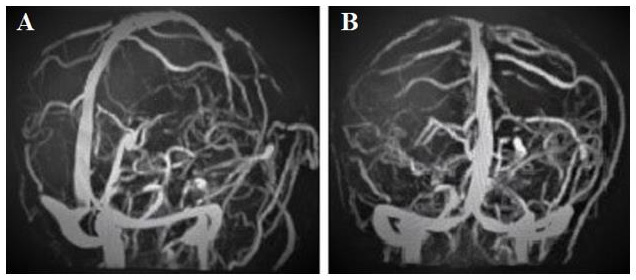
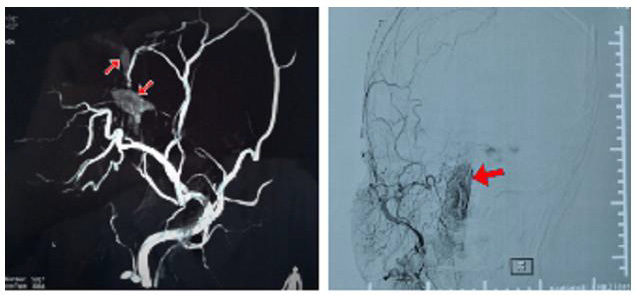
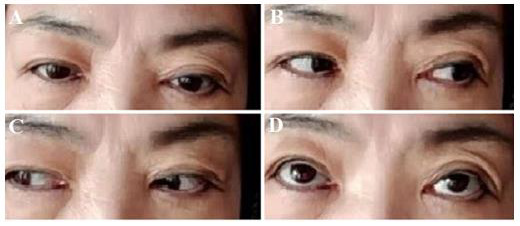
DSA showed bilateral cavernous sinus visualization and left ocular vein visualization in arterial phase, and the bilateral blood supplying arteries were both branches of the maxillary artery of external carotid artery (Figure 4). after the embolization, the arterial fistula disappeared under bilateral common carotid angiography (Figure 5). The postoperative reexamination head CT is shown in (Figure 6). Postoperative follow-up showed that the local swelling and protrusion of the eye completely disappeared on the 12th day after the operation, and the eye movement re-turned to normal on the 41st day after the operation, without diplopia. At present,4 months after the opera-tion, the patient still has a prominent visual impairment, her visual acuity is 6/10 OD and 20/50 OS, accompanying no other symptoms and sign (Figure 7). CCF is caused by the direct injection of arterial blood into the cavernous sinus after the carotid artery and its branches are ruptured. In terms of etiology, the direct type usually occurs in young people, usually caused by trauma (the most common), or medical reasons (such as surgical trauma), fibromuscular dysplasia, ruptured cavernous aneurysm, collagen deficiency and arterial dissection [3-6].
Figure 4: DSA shows: In the Arterial phase, both cavernous sinuses and left ocular veins can be seen. The blood-supplying arteries on both sides are the branch vessels of the maxillary artery, which is the branch of the external carotid artery.
Figure 7: The picture obtaining on the 41st day follow-up after the operation showed that the patient had no eye movement disorders and no diplopia.
The C-type arteriovenous fistulas are more common in postmenopausal women. Most of the fistulas are spontaneous, some can resolve spontaneously, but some patients have a slow progressive aggravation just as we reported here. It is related to cavernous sinus thrombosis, pregnancy, sinusitis, trauma, atherosclerosis, connective tissue disease, hypertension, and diabetes [7-9]. The internal carotid artery passes through the cavernous sinus, also the oculomotor nerve, trochlear nerve, abducens nerve and the ocular branch of trigeminal nerve. Therefore, clinical symptoms such as exophthalmos, diplopia, eye pain, blurred vision, increased intraocular pressure, pulsating tinnitus, headache and ophthalmoplegia often appear after injury [3,4,8-10]. High-flow fistulas can even have orbital murmurs, pulsatile eyeballs, conjunctival edema, ocular surface congestion, vascular distortion (conjunctival spiral blood vessels), dilated and tortuous fundus blood vessels. Compared with direct CCF, indirect CCF is more insidious with milder symptoms and signs. Due to a series of ocular symptoms, many patients are often go to the ophthalmology department firstly. As CCF is mainly manifested by cavernous sinus syndrome and progressive vision loss, it should be identified with orbital apex syndrome, intraorbital congestion, orbital inflammatory pseudotumor, congenital orbital plate defects, endocrine diseases, cavernous sinus tumor com-pression, Tolosa-Hunt syndrome, jugular vein tumors, intraorbital and skull base arteriovenous malformations [11,12].
In terms of diagnostic criteria and auxiliary examinations, because of the diverse clinical manifestations of carotid-cavernous fistula and the low detection rate of CTA/MRV, DSA is the gold standard for CCF diagnosis. It has been reported in the literature that when the difference of the ocular pulse amplitude (OPA) measured by the tonometer exceeds 1.6mmHg, the sensitivity to screen unilateral CCF reaches 100% and the specificity reaches 93%. There is no difference between direct type and the indirect type [13]. Orbital ultrasound can usually show dilated superior ocular veins and orbital hyperemia, thickening of extraocular muscles, etc. It can also be used as a basis for differential diagnosis, such as orbital tumors, thyroid dysfunction, orbital disease, orbital inflammation, scleritis, myositis or endocrine Myopathy [14]. In terms of treatment, most of the indirect CCF are low-flow fistulas. The fistulas may close spontaneously and often do not require invasive treatment. Observation is the main focus. However, if there is an uncontrollable increase in intraocular pressure, persistent ophthalmoplegia and diplopia, severe exophthalmos with corneal expo-sure, optic neuropathy, retinal ischemia, severe murmur on auscultation, and angiography or SWI showing cortical venous fistula drainage, early intervention and treatment should be required [10]. Transvenous endovascular embolization is the preferred treatment for indirect carotid-cavernous fistulas. If the access via the femoral vein is restricted, the direct orbital approach can be selected [15], but the former method is safer and more effective. When the intravascular approach is not feasible or unsuccessful, stereotactic radiosurgery (SRS) can be considered for CCF.
In summary, the symptoms of indirect low-flow cavernous fistula are mild at onset, and the clinical symptoms are not typical, such as dizziness, headache, eye pain, conjunctival congestion and edema, mild eye movement limitation, and often within the normal range of intraocular pressure. There is no abnormality in head MRI, and it is easy to be missed and misdiagnosed clinically. Some lowflow fistulas can close spontaneously, and the clinical symptoms are naturally relieved, while some low-flow fistulas progress slowly, and the symptoms and signs gradually become prominent. When the patient has a headache, eye pain, exophthalmos, and conjunctival congestion and edema, the cranial nerve palsy of the first branch of the third, fourth, Ⅴ, and Ⅵ groups, ac-companied by decreased vision, even if there is no typical pulsating exophthalmos and eye circumference For murmurs, the possibility of CCF should also be considered, and active surgical treatment should be carried out to relieve symptoms as soon as possible to prevent sequelae optic nerve damage.
For more Articles on: https://biomedres01.blogspot.com/



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.