Gentamicin Wet Compress and Hormone Therapy for Superficial Second-Degree Burns Complicated with Atopic Dermatitis
Background
One of the characteristics of burns is a large area of skin damage. The barrier function of the skin is destroyed, and the burn wound becomes the main way of an invasion of allergens and pathogenic bacteria. As a type of superficial burn, a superficial second-degree burn is usually characterized by local redness, severe pain, blisters of various sizes, and basal flushing containing yellow or reddish plasma like fluid after removal of the epidermis [4]. Once the burn wound is infected and allergic, it will lead to slow healing of the wound, and even after healing, it is often accompanied by scars and pigment deposition. Although it is not a fatal disease, the scars and itching that result from wound healing often adversely affect patients’ quality of life and physical and mental health [5]. Atopic dermatitis secondary to burns is rare and its treatment is unclear. At present, the traditional treatment is mainly glucocorticoid, but the curative effect is just acceptable and the course of disease is long. Allergies may lead to slower wound healing and more obvious scars, so how to treat patients with atopic dermatitis secondary to burns more effectively has become the focus of clinical treatment. We present a case of a superficial second-degree burn complicated with [6,7] atopic dermatitis managed with dexamethasone wet compress, gentamicin wet compress and hormone therapy which turn out to be a satisfying augmentation with less invasion as reported below [8].
Methods
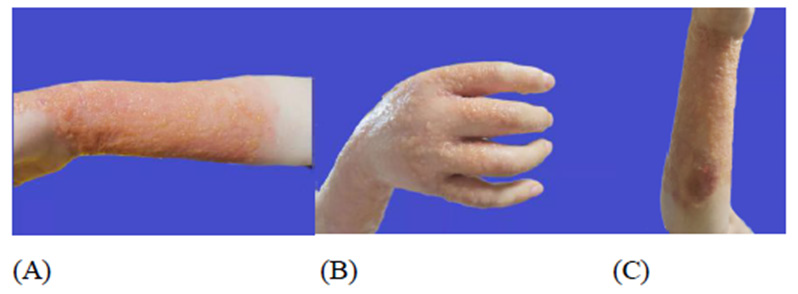
A 24-year-old female patient was admitted with hydrothermal burns 36 hours after the burn. She was diagnosed with superficial second-degree burns on her right forearm and back of the right hand, covering an area of about 3%, without any complications [9]. Physical examination revealed scattered yellowish blisters of different sizes on the right forearm and back of the right hand, with partial epidermal exfoliation, basal flushing, local redness and swelling, accompanied by severe pain and anesthesia, meeting the diagnostic criteria for superficial second-degree burns (Figure 1). Before admission, the patient underwent dressing change for burns at a local hospital. The specific external medication was unknown, and no internal medicine treatment was provided.
Figure 1: Observation before burn treatment.
A. The burned area on the front of the right forearm.
B. The area on the back of the right hand.
C. The area on the back of the right forearm.
Local Treatment
On the first day of her admission, wound care and a dressing change was performed. The next day when removing the old dressing, we saw widely distributed intensive blisters with “needle point” and “green bean” sizes in her right forearm, slow yellow drainage outflow, and intensive and transparent blisters with “needle point” sizes distributed from nearness to farness in the skin surface of metacarpophalangeal joints. The patient complained of “an allergic constitution”, but the allergen was unknown. After consultation with a dermatologist, she was diagnosed as allergic dermatitis secondary to burns. Changing the treatment plan: We used a dilution of normal saline and iodophor according to a ratio of 1 to 1 to disinfect the wounds three times, mixed gentamicin injectable solution 4ml (Henan Runhong Pharmaceutical Co., LTD., GB: H41020318, Specification: 2ml: 80,000 U), dexamethasone injectable solution 2ml (Zhengzhou Zhuofeng Pharmaceutical Co., LTD., GB: H41020055, Specification: 1ml: 5mg) and 100ml 0.9% sodium chloride injectable solution and then soaked the sterile gauze in the mixture. The gauze was spread flat on the wound surface with vascular forceps and tweezers without dripping solution and applied for 20 minutes once a day [10]. After the application, we applied a piece of double sterile gauze to the wound, ensuring aseptic operation during the whole process.
Internal Medicine Treatment
On the first day of admission, two measures were taken: antiinfection: injecting cephalosporin injectable solution 0.5g (Hainan Hailing Chemipharma Co., LTD., GB: H10930215, Specification: 0.25g), and analgesia: dezocine injectable solution (Yangzijiang Pharmaceutical Group Co., LTD., GB: H20080329, Specification: 1ml: 5mg) IV drip treatment. In addition to anti-infection and analgesia treatment, we used methylprednisolone injectable solution (Pfizer Manufacturing Belgium NV approval number: H20170197, Specification: 40mg) IV drip treatment (injecting 80mg methylprednisolone injectable solution into 250ml 0.9% sodium chloride injectable solution at 8:00 a.m. each day and 40mg methylprednisolone injectable solution into 100ml 0.9% sodium chloride injectable solution at 8:00 p.m. each day). Additionally, 1 tablet loratadine BID (Shenzhen Salubris Pharmaceuticals Co., Ltd., GB: H20020092, Specification: 5mg) was taken orally according to the direction of a consultant dermatologist. This therapy was followed by a 4-day methylprednisolone injection reduction (injecting 60mg methylprednisolone injectable solution into 250ml 0.9% sodium chloride injectable solution at 8 a.m. each day) and loratadine discontinuation. Two days later, the drug was discontinued.
Results
During hospitalization, the patient had no adverse reactions and other complications, burn wounds was healed well, the pain was relieved, and blisters disappeared with a little pigmentation. Therefore, using wet compress, combined with anti-infection and anit-allergic therapy for the treatment of atopic dermatitis secondary to burns can obviously accelerate the subsiding of allergic symptoms [11], and the patient’s satisfaction is good, so it is worth clinical application and promotion (Figure 2).
Figure 2: Observation before burn treatment.
A. The burned area on the front of the right forearm.
B. The area on the back of the right hand.
C. The area on the back of the right forearm.
Discussion
Superficial burns are usually burns of less than two degrees. Superficial second-degree burns damage the epidermis and the superficial dermis, which are rich in nerves and sensitive to local pain. The etiology and pathogenesis of eczema secondary to burn wounds are different from that of common eczema. Most researchers argue that this is relevant to traumatic factors such as bacterial colonization and drugs for external use. To name but a few:
• Patients’ constitution are allergic to external medication for burns
• After the burn, the skin basal tissue is subjected to different degrees of heat damage, tissue protein in the wound denatured with a series of inflammatory reactions, tissue liquefied and necrosed, bacterial peptides, toxins and antigen-antibody complexes are recognized by antibodies of the immune system, causing allergic symptoms
• Patients’ burn wounds are in a stress state, and is easily affected by diet, contactants and weather changes during treatment, resulting in allergic symptoms
• The abnormality of the immune system is also one of the causes of allergies secondary to burns. To sum up, both internal factors and environmental factors can be allergens.
But the epidermis of the blisters in this patient did not fall off and rupture, so this may be the reason for the late allergic reaction of the patient. Once allergic symptoms occur, it is necessary to change the treatment in time. In addition to making thorough burn dressing change on the wound in time, applying appropriate antibiotics to avoid infection and using anti-allergic drugs, combined with wet compress therapy such a local treatment can achieve a good therapeutic effect. About the antihistamine for inhibiting allergic symptoms, oral desloratadine is the first choice in our hospital, which has a strong and selective antagonistic effect against peripheral H1 receptors. In addition to counteract histamine in the body, desloratadine also shows antiallergic and anti-inflammatory effects, which is worthy of clinical application and promotion. Glucocorticoid drugs have an anti-allergic effect, can relieve various symptoms of acute inflammatory reaction and prevent some inflammatory sequelae, such as tissue adhesion and scar formation. So local treatment of the wounds combined with methylprednisolone can effectively inhibit allergic reactions. But this kind of medicine has no inhibiting effects on pathogenic microorganism. Furthermore, because it can inhibit inflammatory reactions and immune responses, and weaken the body’s defense ability, it has the potential to activate or spread latent infectious lesions. Moreover, the long-term use of hormone drugs may cause hormone dependence, and more adverse reactions [12], is also very important so joint anti-infection treatment [13]. In conclusion, it’s necessary to combine anti-infective treatment. To sum up, wet compress combined with anti-infection drugs and anti-allergy drugs can significantly promote the wound healing and relieve symptoms in the treatment of burn complicated with allergy, with significant efficacy.
For more Articles on: https://biomedres01.blogspot.com/




No comments:
Post a Comment
Note: Only a member of this blog may post a comment.