Effect of Coenzyme Q10 Treatment on Clinical Manifestations in a Young Woman with Mitochondrial Diabetes
Abstract
We report the case of a 25-year-old woman with mitochondrial diabetes
mellitus (MDM). She was diagnosed with Wolff-Parkinson-White syndrome
at 12 years old. She was later diagnosed as diabetes mellitus without
autoimmune disorders at 15 years old, and the mitochondrial DNA 3243
mutation was detected by the gene analysis. Neurosensory deafness was
identified at 16 years of age, and hypertrophic left ventricular
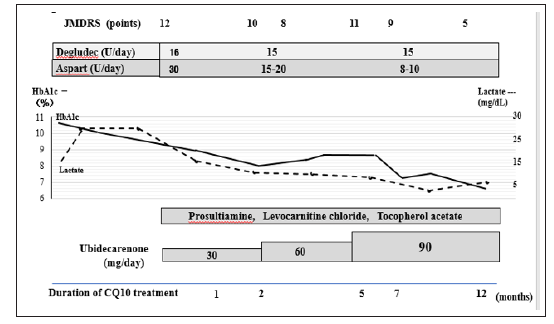
cardiomyopathy was detected at 24 years of age. We started
administration of coenzyme Q10 (CQ10), and subsequently her clinical
symptoms and glycemic control were improved accompanied by decreasing
blood lactate level. We assessed neurological signs of MDM using the
Japanese Mitochondrial Disease Rating Scale (JMDRS). The JMDRS was
improved from 12/80 points at the start of CQ10 to 5/80 points at
12-month period after starting CQ10. These findings suggest that CQ10
treatment could be effective on clinical symptoms, a lactate level and
glycemic control in a patient with MDM.
Keywords: Mitochondrial Diabetes Mellitus; Glycemic Control; Endogenous Insulin Secretion; Neuromuscular Symptom; Coenzyme Q10
Abbrevations: BMI: Body Mass Index, CPR:
C-Peptide Immunoreactivity, CQ10: Coenzyme Q10, FPG: Fasting Plasma
Glucose, HbA1c: Hemoglobin A1c, JMDRS: Japanese Mitochondrial Disease
Rating Scale, MODY: Maturity Onset Diabetes of the Young, MDM:
Mitochondrial Diabetes Mellitus, WPW syndrome: Wolff Parkinson White
Syndrome
Introduction
Mitochondrial disease shows various clinical manifestations such as
neuromuscular disorders, including muscle weakness, encephalopathy,
mental disorder and neurosensory deafness, cardiomyopathy, short stature
and diabetes mellitus. Of these disorders, diabetes mellitus is known
as maternal inherited mitochondrial diabetes mellitus (MDM), which is
identified in up to 1% of all patients with diabetes mellitus. The
mitochondrial DNA 3243A>G mutation is most common genetic abnormality
(80-90%), whereas other mutations, such as 8296A>G and 14577T>G,
are less frequent [1]. Diabetes mellitus is the most common endocrine
disorder in mitochondrial disease, because mitochondrial dysfunction
greatly affects pancreatic β-cells, leading to insulin secretion defect
[2]. Coenzyme Q10 (CQ10) is well known to act as an electron carrier of
the respiratory chain in mitochondria and has been shown to improve the
mutation-associated dysfunction of the respiratory chain in
mitochondria. Various reports demonstrated that administration of CQ10
had some clinical benefits toward neuromuscular symptoms [3], elevated
lactate levels [4], and
neurosensory deafness [5]. On the other hand, there were few reports
showing improvement in glycemic control and endogenous insulin secretion
when using CQ10 in patients with MDM [5,6]. We encountered a case of
MDM with the mitochondrial DNA 3243A>G mutation, and hereby reported
changes in glycemic control and other clinical manifestations after
administration of CQ10.
Case Report
A 25-year-old woman presented to our hospital with leg numbness,
malaise, headache and muscle weakness, which had existed for 1-month
period. She was already diagnosed with MDM and treated with insulin. Her
hemoglobin A1c (HbA1c) levels continued to be 8-9%, despite multiple
daily injections of insulin. She was admitted to our hospital for
examination of neuromuscular symptoms and improvement of glycemic
control.
In the past history, her growth and psychomotor development were
normal. She was diagnosed with Wolff-Parkinson-White (WPW) syndrome at
12 years of age. She was found to have
glucosuria through a urine glucose screening at schools at 15 years
of age and identified as having diabetes in the detailed examination
of the screening program. She was not obese with body mass
index (BMI) of 18.8kg/m2, β-cell associated antibodies were all
negative, and insulin secretion capacity was maintained at the time
of diagnosis. There were no neuromuscular symptoms, including
muscle weakness, fatigue and impaired hearing, at that time.
Subsequently, maturity-onset diabetes of the young (MODY) genes
and mitochondrial DNA genes were analyzed, and the mitochondrial
DNA 3243A>G mutation was detected (Figure 1).
Figure 1: Analysis of mitochondrial DNA 3243 mutations.
Discussion
CQ10 is an essential electron carrier in the mitochondrial
respiratory chain. It acts as an electron carrier in the electron
transport chain from complex I-Ⅱ to complex Ⅱ-Ⅲ, and is present
in all tissues and cells in the inner mitochondrial membrane [10].
CQ10 is also a lipid-soluble antioxidant and scavenges reactive
oxygen species [11]. The mechanisms connecting mitochondrial
DNA 3243 mutations and onset of diabetes are thought to be as
follows:
a) Accelerated production of reactive oxygen species and
increased oxidative stress,
b) Reduced oxidative phosphorylation and decreased ATP
levels in pancreatic β-cells,
c) Damaged signal transduction in pancreatic β-cells and
reduction in their cell numbers due to apoptosis,
d) Exhaustion of insulin secretion [12-14].
CQ10 plays a role in stopping step 1), thereby preventing
progression to steps 2), 3), and 4). Accordingly, administration of
CQ10 might prevent the advance to insulin exhaustion; improving
insulin secretion and glycemic control. Richter et al. [15] reported
that insulin secretory defects may result from anti-oxidation
activities and dysfunction in the mitochondrial respiratory
chain. Administration of CQ10 can stop the dysfunction of the
mitochondrial respiratory chain and insulin secretion could be
improved. The course of the patient described showed important
clinical information of possibility of improvement in glycemic
control and endogenous insulin secretion as well as clinical
symptoms and a blood lactate level with using CQ10 in MDM. There
are some reports showing therapeutic effects on neuromuscular
symptoms and a blood lactate level [3-6].
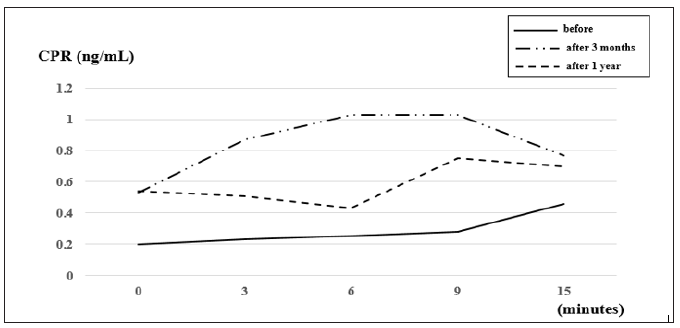
On the other hand, there were few reports showing improvement
in glycemic control and endogenous insulin secretion when using
CQ10 in patients with MDM [5,6]. Okazaki et al. [6] reported a large
dose of CQ10 (60 mg/day) was effective to improve HbA1c levels
from 8.5% to 7.5% and to increase glucagon loading CPR levels
from 1.8 ng/dL to 2.0 ng/mL at the study of 2-year period. There
were some other case reports demonstrating the efficacy of CQ10
on glycemic control for a short period less than 1 year [5,16,17].
Reported more increase in CRR response on glucagon loading
test and urinary excretion of CPR among 28 patients with MDM
compared with 16 patients without receiving CQ10 treatment
for 3-year study period. As compared to the studies conducted
by Okazaki et al. [5,6] our study period for 1 year is shorter, and
it seems too early to judge the effect of CQ10 on glycemic control
and endogenous insulin secretion. Longer-term follow-up should
be necessary to evaluate the effect of CQ10 on diabetic control in
our case. On the other hand, we started some medication, such
as prosultiamine, levocarnitine chloride and tocopherol acetate,
other than administration of CQ10. These drugs could play a role
to improve mitochondrial function with increasing endogenous
insulin secretion and reducing plasma glucose levels. In conclusion,
we reported the clinical course with CQ10 treatment in the case
of MDM presenting with mitochondrial DNA 3243A>G mutation.
CQ10 treatment could be effective on clinical symptoms, a lactate
level and glycemic control in a patient with MDM.
Tubal Stump Pregnancy in ART Patients
Two cases of ectopic stump pregnancy after IVF-ET - https://biomedres01.blogspot.com/2020/02/tubal-stump-pregnancy-in-art-patients.html
More BJSTR Articles : https://biomedres01.blogspot.com



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.