Molecular Study of Staphylococcus Epidermidis Strains Isolated from Clinical Specimens from Different parts of Rouhani Hospital (Babol, Iran)
Introduction
Staphylococci are known as a gram-positive, non-motile and non-spore forming cocci which are divided into two mains coagulase-negative and coagulase-positive staphylococci [1]. Staphylococcus Epidermidis with the highest prevalence rate is recognized as the most significant member of the family of coagulase-negative staphylococci and plays an important role in nosocomial infections [2]. S. epidermidis is considered as the main contributor in medical equipment infections. In recent decades, due to the clinical importance and emergence of methicillin-resistant S. epidermidis strains, this organism has become a challenge in the treatment of patients [3]. Several virulence factors and resistance genes were identified in which the mecA and ica gene are the important one [4]. Many strains of S. epidermidis produce an N acetylglucosamine (PNAG) homopolymer, called PIA which is associated in biofilm formation [5].
Isolation and Identification
A total of 50 S. epidermidis strains were collected from bloodstream, urine, catheter, shunt, body fluids and wound infections from different wards including open heart surgery, orthopedics, neurology, infectious disease, ICU and NICU of Rouhani Hospital. In addition a total of 10 S. epidermidis strains were obtained from hospital staff for RAPD-PCR test. The isolates were referred to the laboratory of the Babol University of Medical Sciences for confirmation by microbiological test such as gram staining, catalase, coagulase, mannitol fermentation on mannitol salt agar media and sensitivity to polymyxin B and finally stored at -20 °C.
Antibiogram test was performed by disk diffusion method according to CLSI 2016 standards. In this test, Muller Hinton Agar (Merck - Germany) and antibiotic disks included Cefoxitin (30 μg), Oxacillin (1 μg), Gentamicin (10 μg), Erythromycin (15 μg), Clindamycin (2 μg), Ciprofloxacin (5 μg), Fusidic acid (10 μg), Levofloxacin (30 μg), Trimethoprim/Sulfamethoxazole (1.25/23.73 μg), Vancomycin (30 μg), and Linezolid (30 μg) (ROSCO - Denmark) was used.
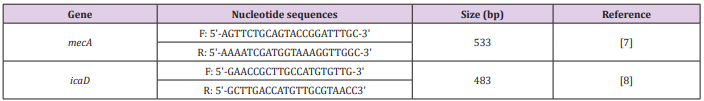
In order to perform PCR, the MasterMix was prepared in a final volume of 25μl, including: 12.5μl Super MasterMix 2X, 1μl of each primer (Forward & Reverse), 3μl DNA template and 7.5μl Sterile Deionized Water. PCR cycles was perform with initial denaturation temperature of 94°C for 5 minutes, then 30 cycles with a denaturation temperature of 94°C for 30 seconds, annealing temperature of 55°C for 30 seconds, and an extension temperature of 72°C for 40 seconds and a final extension cycle was performed at a temperature of 72°C for 5 minutes. The specific primers are shown in (Table 1).
 RAPD Analysis
RAPD AnalysisThe DNA genomic was extracted by commercial kit (Yekta-Tajhiz, Iran) and RAPD-PCR assay was carried out according to procedure described previously by Burucoa [8,9]. PCR was performed in a final volume of 25μl containing 12.5μl Super MasterMix 2X, 1μl Primer (5’-CCG CAG CCA A-3’), 3μl DNA Template and 8.5μl Sterile Deionized Water [10]. The PCR program was done as 95 °C for 1 min as an initial hot start followed by 94 ºC for 1 min, 30ºC for 1 min, and 72ºC for 2 min for 4 cycles, followed by 36 cycles of 94ºC for 1 min, 36ºC for 1 min, and 72ºC for 2 min and a final extension step of 72ºC for 5 min. Finally, RAPD-PCR profiles were analyzed by using GelQuest software with 80% similarity cut-off point with clustered using the Dice’s coefficient, and a dendrogram generated based on the Unweighted Pair Group Method with Arithmetic mean (UPGMA).
A total of 60 S. epidermidis strains were collected from different wards of Rouhani Hospital. Due to our results the infectious diseases and ICU wards had the highest rate of specimens in comparison to other wards. 53% of isolates were belonged to female gender. By disc diffusion method no resistance was reported to vancomycin and linezolid, while the rate of resistance to oxacillin, gentamicin, cefoxitin, clindamycin, ciprofloxacin and erythromycin were 70.5%, 45.9%, 55.7%, 55.7%, 63.9% and 59% respectively. On the other hand, resistance to trimethoprim/sulfamethoxazole (39.4%), fusidic acid (25.4%) and levofloxacin (41%) was noticeable (Figure 1). The prevalence of mecA and icaD genes was 85% and 41.6% respectively. There were no significant correlation between detected genes and gender (P-value > 0.05). In addition, twenty-four different RAPD-Types were analysis by 80% similarity cut-off point which indicates the high genotypic diversity in our isolates (Figure 2). Table 2 is shown the complete details of all studied isolates.
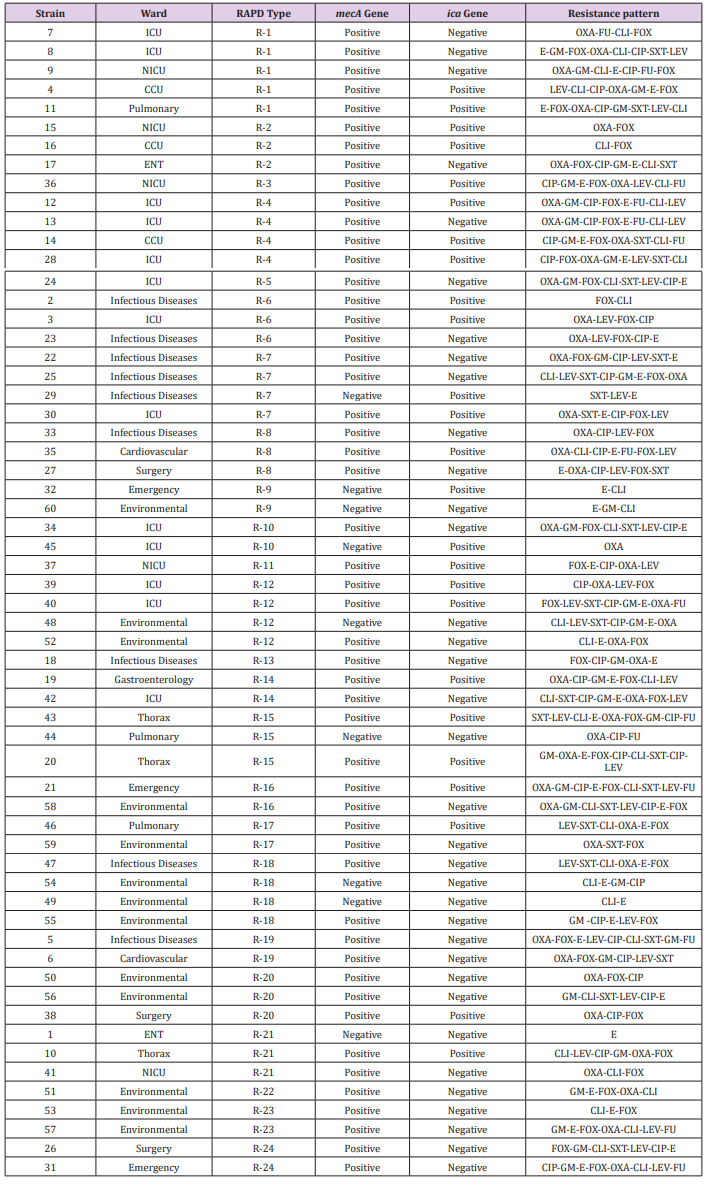 Figure 1: Antibiotic Resistance pattern of S. epidermidis strains isolated from Rouhani Hospital.
Figure 1: Antibiotic Resistance pattern of S. epidermidis strains isolated from Rouhani Hospital.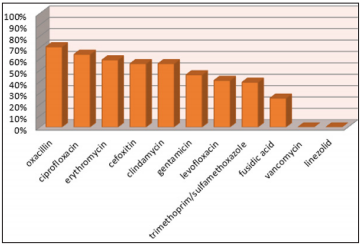 Figure 2: Dendrogram Cluster Analysis of RAPD-PCR Data for 60 S. epidermidis Isolates.
Figure 2: Dendrogram Cluster Analysis of RAPD-PCR Data for 60 S. epidermidis Isolates.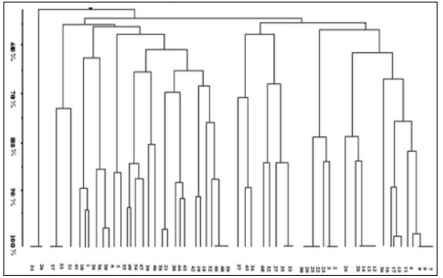 Discussion
DiscussionAccording to the results, the presence of mecA and icaD genes among S. epidermidis strains obtained from Rouhani Hospital in Babol was 85% and 41.6%, respectively. The frequency of these genes among similar studies is reported differently. In a study conducted by Najar-Peerayeh et al. The presence of the mecA gene was 92.2% [11]. In the study of Pourmand et al., the frequency of mecA gene was reported 95%, which is higher than of all conducted studies in Iran. Also, resistance to clindamycin and erythromycin in this study was 77% and 79%, respectively which is higher than our study [12]. Moreover, in Pishva et al. research in Al-Zahra Hospital in Isfahan, 75.3% of S. epidermidis strains harbored mecA gene [13]. In a study by Soroush et al., on 80 S. epidermidis strains which was collected from children, 41% had icaD gene. In this study 90% of isolates were found multi-drug resistance, in which the rate of resistance to co-trimoxazole was reported 91.2%. On the other hand, no resistance was observed to linezolid and vancomycin [14].
More BJSTR Articles : https://biomedres01.blogspot.com



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.