Comparative Study of Clinical and Polysomnographic Characteristics of Obstructive Sleep Apnea Among Obese and Non-Obese Patients at Chiang Mai University Hospital
Background
Obstructive sleep apnea (OSA) is a disease characterized by repetitive sleep disruptions due to episodes of upper airway obstruction (UAO), resulting in nocturnal hypoxemia, sleep termination with frequent arousals, and excessive daytime sleepiness [1- 3]. OSA is more common than generally believed. It can also be a serious and life-threatening disorder, which may lead to adverse cardiovascular consequences and increased mortality. Obesity has been recognized as one of the classical risk factors of OSA, with up to 60% of OSA patient being obese, and up to 40% of the obese population carrying a diagnosis of OSA [4]. This may be due to anatomical alterations in obesity predisposing to UAO or collapse during sleep. Recent studies have shown that OSA is not uncommon in the non-obese population, and many have proposed some different characteristics of OSA in this population in regard to clinical, cephalometric and polysomnographic features, suggesting two different disease entities among the OSA population. For non-obese OSA patients, medical comorbidities (e.g. diabetes mellitus, hypertension, and coronary artery disease (CAD), smoking, alcohol use and sedative drug use) were less prevalent. As for cepholometric parameters, thyromental distance was significantly shorter in this population. However, differences in other factors, including adenotonsillar hypertrophy, neck circumference, and symptoms of excessive day time sleepiness (EDS) evaluated by the Epworth Sleepiness Scales (ESS) did not reach statistical significance. On the other hand, OSA was more severe in obese patients as demonstrated by most polysomnographic parameters including the apnea-hypopnea index (AHI) [4-10]. However, related studies were scarce and diverse, with small samples, were rarely conducted in Asian populations. Only one study to date [5] has employed the proposed classification of weight by BMI in adult Asians by WHO (WPRO, 2000), using BMI ≥ 25kg/m2 as the cutoff point for obesity, which is currently used as a reference based on the risk of morbidities [11,12].
Objectives
This study was designed to evaluate the differences in clinical, anthropometric and polysomnographic characteristics between non-obese and obese patients with OSA in a Thai population.
Material and Methods
This retrospective observational study was done by reviewing data from all patients aged ≥16 years referred to Chiang Mai University Hospital Sleep Clinic for suspected OSA who underwent polysomnography confirmation from January 2013 to December 2015. OSA was diagnosed by polysomnography when AHI was > 5 events/h with consistent clinical symptoms, including frequent snoring or EDS. This study was conducted under approval by the local research ethics committee. Patients with pregnancy, uncontrolled congestive heart failure or chronic obstructive pulmonary disease (COPD) were excluded from the study. Data regarding clinical characteristics, anthropometric measurements and polysomnographic parameters was collected from the medical record with review of the polysomnographic report by the authors, including:
a) Baseline clinical characteristics: age, sex, associated comorbidities (DM, HT, DLP, CAD, DCM, CVA, asthma, and COPD) and clinical presentation of OSA (EDS, Epworth Sleepiness Scale (ESS), snoring, morning headache, apnea, awakening, and nocturia).
b) Anthropometric measurements: height, body weight, body mass index (BMI), neck and waist circumferences, Friedman Tongue Position (FTP) classified into grade I-IV, presence of adenotonsillar hypertrophy and grading from 0-4, long uvula, high arch palate, micrognathia, and retrognathia.
c) Polysomnographic parameters: total, REM, and NREM AHI, respiratory arousal index, desaturation index, minimal oxygen saturation, total sleep time with oxygen saturation < 90%, periodic leg movement index (PLMI), CPAP use, and CPAP pressure.
Patients were stratified into obese and non-obese groups, using BMI ≥ 25kg/m2 as the cutoff for obesity. The primary aim of the study was to compare the clinical characteristics, cephalometric measurements and polysomnographic findings between non-obese and obese patients with OSA. The secondary aim was to determine the percentage of OSA patients that were non-obese.
Statistical Analysis
All statistical analysis of the data was performed using SPSS version 22.0(SPSS Inc., Chicago, USA). The quantitative variables were expressed as mean ± standard deviation (SD), and the qualitative variables as frequencies and percentages. χ2 test was used to evaluated categorical data. Numerical data which exhibited normal distribution was analyzed using the student t-test, while data that was not normally distributed was analyzed by the non-parametric Mann-Whitney U test. The Fisher Exact test was used for data with an expected frequency of variable ≤5. In order to determine the relationship between the study variables and OSA, multivariate logistic regression analysis was performed. A P value of < 0.05 was considered statistically significant in all analyses.
Results
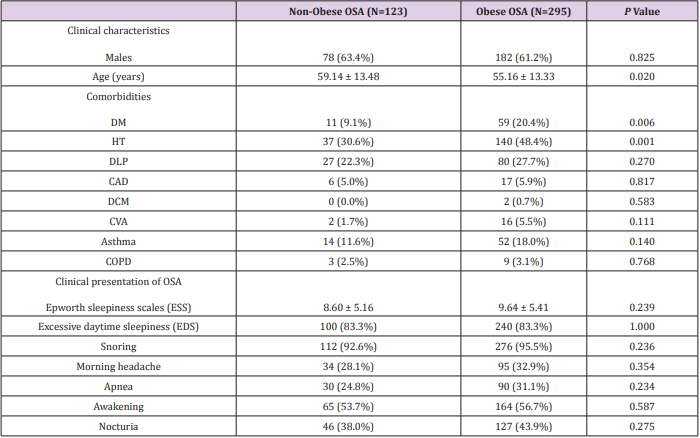
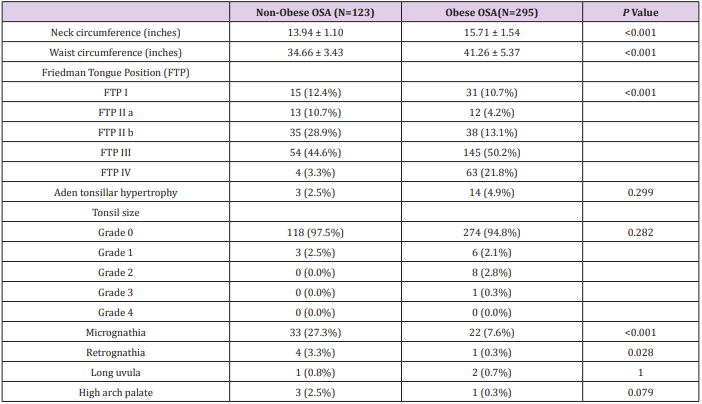
During the study period, 421 patients were evaluated at Chiang Mai University Sleep clinic for suspected OSA and had polysomnography performed. Three of these patients were excluded due to missing data (on BMI). A total of 418 patients remained for analysis, of these, 295 (70.6%) were obese and most patients were male (62.2%). Mean age was significantly higher in the non-obese group (59.14 ± 13.48 yr vs 55.16 ± 13.33 yr, p 0.020). Diabetes mellitus and hypertension were more prevalent in the obese group (20.4% vs 9.1%, p 0.006, and 48.4% vs 30.6%, p 0.001, respectively). However, there were no differences in any other comorbidities, ESS, EDS or other clinical parameters Table 1. Regarding anthropometric measurements, larger neck circumference (15.71 ± 1.54 in vs 13.94 ± 1.10 in, p <0.001) and waist circumferences (41.26 ± 5.37 in vs 34.66 ± 3.43 in, p <0.001) were noted in the obese patients. Also, in the obese population, the Friedmann Tongue Position (FTP) score was significantly higher (p < 0.001), while micrognathia and retrognathia were more common in the nonobese group (27.3% vs 7.6%, p < 0.001, and 3.3% vs 0.3%, p 0.028, respectively). Differences in other parameters including adenotonsilar hypertrophy, tonsil size, and presence of a long uvula or high arched palate did not reach statistical significance Table 2.
Table 1: Frequency of different Candida species isolated from vaginal discharge of women undergoing IVF-ET.
Table 2: Frequency of different Candida species isolated from vaginal discharge of women undergoing IVF-ET.
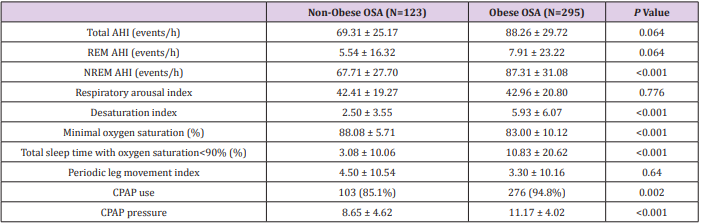
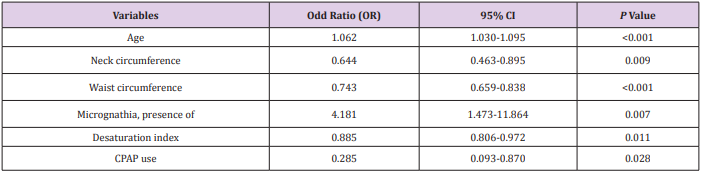
Regarding polysomnographic findings, most patients in both groups had severe OSA, represented by mean total AHI of 88.26 ± 29.72 and 69.31 ± 25.17 in obese and non-obese patients, respectively, and the majority (92%) were using CPAP. Obese OSA patients had significantly worse polysomnographic parameters as demonstrated by higher NREM AHI (87.31 ± 31.08 vs 67.71 ± 27.70), desaturation index (5.93 ± 6.07 vs 2.50 ± 3.55), more total sleep time with oxygen saturation < 90% (10.83% vs 3.08%), more CPAP use (94.8% vs 85.1%) with higher CPAP pressure (11.17 ± 4.02 vs 8.65 ± 4.62 cmH2O), but lower minimal oxygen saturation (83.00% vs 88.08%) Table 3. Multivariate logistic regression analysis showed that only increasing age (OR 1.062, p <0.001), lower neck and waist circumferences (OR 0.644, p 0.009, and OR 0.743, p < 0.001, respectively), presence of micrognathia (OR 4.181, p 0.007), lower desaturation index (OR 0.885, p 0.011), and more CPAP use (OR 0.285, p 0.028) were significantly and independently associated with OSA in the non-obese population Table 4.
Table 3: Frequency of different Candida species isolated from vaginal discharge of women undergoing IVF-ET.
Table 4: Frequency of different Candida species isolated from vaginal discharge of women undergoing IVF-ET.
Discussion
Many previous studies have shown that OSA is not restricted to the obese population, with up to 40% of patients being non-obese [4, 6-8]. A recent study in Thailand [5], on the contrary, discovered that the majority of OSA patients were non-obese (63.4%). Our study finding that 39.4% of OSA patients under evaluation were non-obese is in concordance with the previous literature. Regarding comorbidities, hypertension, dyslipidemia and coronary artery disease have been shown to be more prevalent in obese compared to non-obese patients in several studies [5,8]. Hypertension, obesity and OSA can either co-exist or contribute to the progression of one other, leading to resistant hypertension and adverse cardiovascular outcomes. Our finding of higher hypertension prevalence in the obese patients was similar; in addition, diabetes mellitus was also more common in this group, which the relationship between obesity and insulin resistance and metabolic syndrome may be responsible for. Obese patients with OSA are known to have greater disease severity, represented by worse polysomnographic parameters in many trials [4,5,8,9], including higher AHI, total sleep time with oxygen saturation <90%, respiratory arousal index, and lower minimal oxygen saturation. Our study further confirmed these findings with polysomnographic parameters more severe in nearly all aspects in obese patients, especially higher desaturation index in obese patients with OSA. Moreover, our data on CPAP showed a higher percentage of CPAP usage and higher CPAP pressures in the obese group, possibly due to greater OSA severity.
Surprisingly, the statistical significance of age difference in this study between the two BMI groups has never been elucidated before in the literature. In this study we found that non-obese OSA patients were older than their obese counterparts. One possible explanation of this finding is that the non-obese patients have fewer comorbidities, especially metabolic syndrome, and less OSA severity, which may result in a later presentation and diagnosis of OSA in this population. As for anatomical craniofacial and anthropometric characteristics, obesity is a principle risk factor for OSA due to the anatomical alterations that predispose obese individuals to upper airway obstruction during sleep. Increased soft tissue surrounding the pharyngeal airway within a limited bony closure leads to airway narrowing and collapse. Increased tongue volume from accumulated fat and anterior displacement of the hyoid bone, related to obesity, as well as larger neck circumferences with increased parapharyngeal fat also increase the tendency for upper airway obstruction [9,10]. Larger neck circumference in obese OSA patients compared to non-obese patients in our study supports these previous findings. Furthermore, larger waist circumference in this population as seen in this study is a marker of obesity, especially truncal obesity with increased visceral fat.
On the other hand, non-obese patients with OSA represent a different OSA entity. A study from Sakakibara et al. [9] found the bony structure discrepancies to be a major contributing factor. Short anterior cranial base and mandibular length are the two main predictors [9], accompanied by caudal hyoid, increased soft palate soft tissue, decreased pharyngeal width with airway narrowing at the soft palate level, oropharyngeal and nasopharyngeal narrowing [10]. Higher prevalence of micrognathia and retrognathia in the non-obese OSA group in our study supports findings from previous literature, since such alterations can similarly cause cephalometric imbalance by shortening the length of oropharynx and crowding the upper airway structure.
There were some potential limitations to this study. First, the selection of patients may have been biased. Since our study population was a selected group of patients referred to the sleep clinic for evaluation of suspected OSA, the findings in this study may not be generalizable to the population of patients with milder OSA severity, or those with lower probability of OSA presenting before confirmatory polysomnographic evaluation. Second, this is a retrospective study, with all the implications that this entails. Potential strengths of this study include the relatively large sample size and the large number of variables collected for characteristic studied.
Conclusion
OSA is not uncommon in the non-obese population. Non-obese patients tend to be older, with smaller neck and waist circumferences, and micrognathia as a more prevalent feature. Lower OSA severity was demonstrated by most polysomnographic parameters, especially the desaturation index, and less CPAP use in non-obese patients.
FMR1 Premutation and Demyelinating Syndromes: Case or Causality? A Case Report-https://biomedres01.blogspot.com/2021/03/fmr1-premutation-and-demyelinating.html
More BJSTR Articles : https://biomedres01.blogspot.com


No comments:
Post a Comment
Note: Only a member of this blog may post a comment.