Clinical Evaluation, STOP BANG, Epworth Somnolence Scale and Polyssonography Indexes helps OSAS Screen in Patients with Sleep Complaints: Our Experience in Rio De Janeiro State
Introduction
Obstructive sleep apnea (OSA) is an important public health issue, since epidemiological studies and observations of OSA patients have consistently shown the prevalence of hypertension, type II diabetes, cardiovascular disease, and stroke to be higher in this population (SOMERS 2008). Mental conditions and carotid plaque burden are also associated with low oxygen saturation related to sleep-disordered breathing (SDB) [1,2] OSA derives not only relevant consequences but also presented high prevalence in many studies. According to the population-based study of Hipnolaus in Switzerland, the prevalence of moderate-to-severe SDB (≥15 events per hour) was 23.4% in women and 49.7% in men, which was associated with hypertension, metabolic syndrome, diabetes, and depression [3]. Besides, of 1,042 volunteers selected independently of sleep complaints in São Paulo, OSA was observed in 32.8% and associated with obesity and male sex [4]. The aims of this study were to correlate STOP BANG score, Epworth Somnolence Scale and desaturation to OSA in a Rio de Janeiro population with sleep complaints from a public reference hospital and to highlight OSA severity features in this population.
Methods
This retrospective analysis assessed OSAS severity and the profile of adults with sleep complaints from our database after Research Ethics Committee approval (CAAE 42785214.1.0000.5258). A total of 185 patients with sleep complaints aged 18 to 80 years old (yo) were included. They were systematically evaluated between April 2015 and December 2017 in the sleep ambulatory with a physical exam, translated and validated questionnaires (Epworth Sleepiness Scale [ESS] [5,6] and STOP BANG score [7-9], and laboratory polysomnography studies. Exclusion criteria were: Polyneuropathy; active heart and lung diseases; craniofacial malformations; immunodeficiency; systemic vasculitis; and neoplasia. We used the 2015 Portuguese version of STOP-BANG [7-9] to measure the risk of OSA, whereby three or more affirmative answers indicated a high risk of OSA [8,9] and the Epworth Sleepiness Scale (ESS) [6] to measure diurnal somnolence. In the ESS, sleep propensity was measured in 8 routine situations on a scale from 0 (indicating no chance of falling asleep) to 3 (indicating a high chance of dozing off). The final score ranged from 0 to 24 points accordingly, with excessive diurnal somnolence being defined as a score higher than 10 [6].
Polysomnography parameters: The subjects underwent transcutaneous pulse oximetry, with the respiratory effort recorded using inductance plethysmography. Apnea was measured by an oronasal thermistor and was defined as a drop in baseline airflow by 90% or more for at least 10 seconds. Hypopnea was measured by a nasal pressure cannula and was defined as a partial obstructive event with airflow drop by more than 30% from baseline for at least 10 seconds. Besides, hypopnea was also considered present with oxygen desaturation of 3% or more, with electroencephalographically confirmed arousal. The polysomnography data were measured based on polysomnography recordings (EMSA Equipamentos Médicos, Rio de Janeiro, Brazil). OSAS criteria using the Apnea–Hypopnea Index (AHI) of 5 or higher were defined according to the American Academy Sleep Manual. Our data were analyzed with SPSS 13.0 for Windows. The continuous variables distribution between groups was compared by the Mann–Whitney U test. Categorical variables comparison was performed by Chi-square or Fisher test when indicated. Correlations were performed by Spearman Correlation Coefficient. The significance level was fixed at 5%.
Results
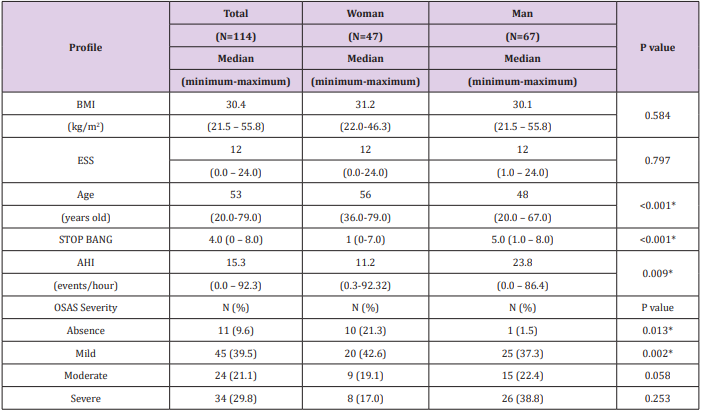
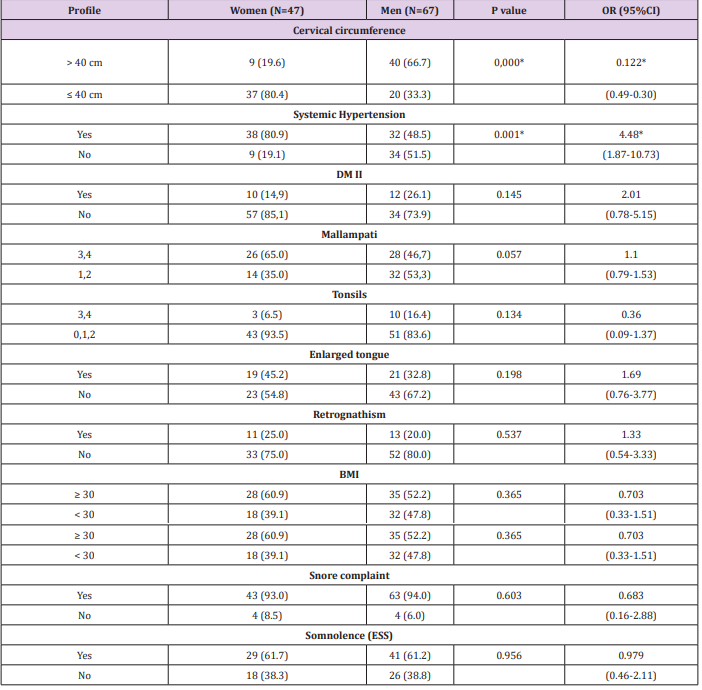
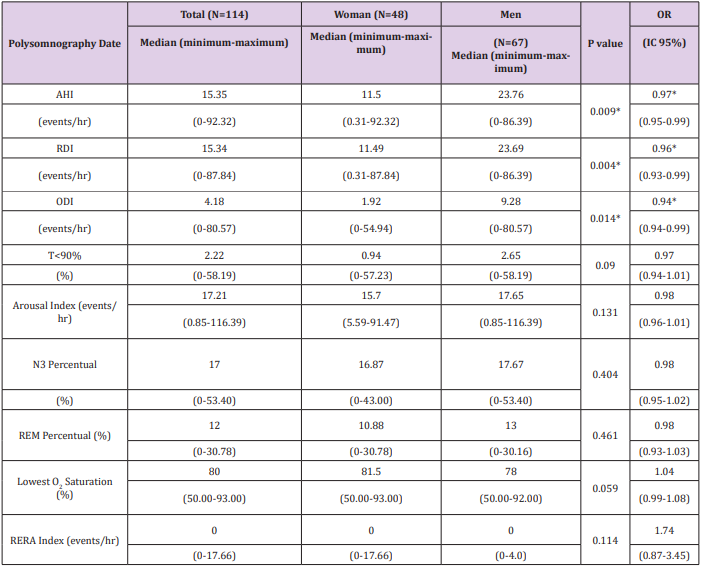
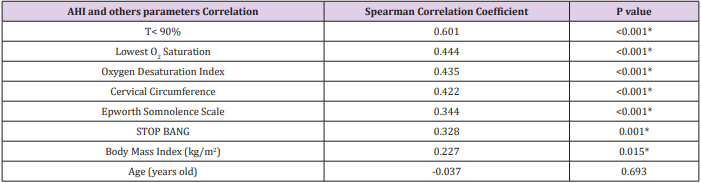
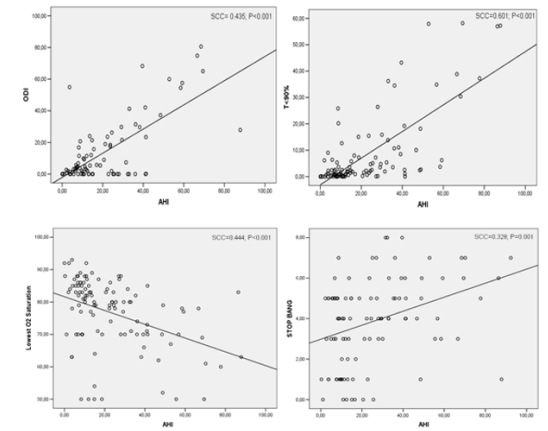
A total of 114 subjects (67 men, 58.8%) were included in this study. The median age was 53.0 yo; median BMI=30.4kg/m2 and median ESS score=12.0 (Table 1). In this population, there were predominantly men with significantly lower age (P<.001), higher median AHI (P=.009), and higher median STOP BANG score (P<.001) than the women’s group (Table 1). Table 2 showed that the prevalence of systemic hypertension in women was four times higher than in men (P=.0001). Despite high body mass index (BMI), type II diabetes prevalence was low in both genders. Although both groups reported snore and somnolence, there was a low prevalence of enlarged tongue, retrognathism, tonsil hypertrophy, and Mallampati grades 3 or 4 (Table 2). In Table 3, AHI, Respiratory Disturbance Index (RDI), and Oxygen Desaturation Index (ODI) were significantly higher in men. The Rapid Eyes Movement (REM) percentage was reduced and the arousal index was elevated in all groups (Table 3). The AHI was correlated with sleep time spent below 90% oxygen saturation (T<90%), lowest O2 saturation, ODI, cervical circumference, ESS score, STOP BANG, and BMI (Table 4 and Figure 1).
Table 1: Patients Demographics.
Note: BMI: Body Mass Index (National Heart, Lung and Blood Institute); ESS: Epworth Somnolence Scale; AHI: Apnea-Hypopnea Index; OSAS: Obstructive Sleep Apnea Syndrome; *statistically significant.
Table 2: Population with sleep complaints medical evaluation.
Note: DMII: Diabetes Mellitus type 2; *statistically significant; BMI: Body Mass Index; ESS: Epworth Somnolence Scale.
Table 3: Polysomnography Date.
Note: AHI: Apnea-Hypopnea Index; RDI: Respiratory Disturbance index; ODI: oxygen desaturation index; O2 : Oxygen; T<90%: sleep time spent below 90% oxygen saturation; *statistically significant.
Table 4: Correlation of Apnea-hypopnea index with others sleepy parameters.
Note: SatO2 : Oxyhemoglobin saturation; O2 : Oxygen; T<90%: sleep time spent below 90% oxygen saturation; AHI: Apnea-hypopnea index; *statistically significant.
Figure 1: Correlation of Apnea-hypopnea index with Oxyhemoglobin saturation and STOP BANG. Note: O2 : Oxygen; T<90%: Sleep time spent below 90% oxygen saturation; ODI: Oxygen Desaturation Index; AHI: Apneahypopnea index; SCC: Spearman Correlation Coefficient.
Discussion
This is the first profile of the population with sleep complaints in Rio de Janeiro. It is a specific mixed ethnic population, different from homogeneous populations from other countries. The ODI, AHI, and RDI were significantly higher in men, who had increased prevalence of OSA risk factors, such as large neck circumference, obesity, male gender, and snore. These features are included in STOP BANG score and previous studies performed in homogeneous populations had already suggested this tool for population screening [10-12]. After bivariate correlation, the AHI was associated with these classic risk factors (cervical circumference, STOP BANG, and BMI), and also with oxygen desaturation (T<90%, ODI, and the lowest O2 saturation), as Guilleminault and cols. (1988) had already reported. Besides, the AHI was correlated to the ESS in this study, as somnolence is a known consequence of moderate and severe OSAS [14]. In our study, there was a low prevalence of hypertrophied tonsils, enlarged tongue, and retrognathism in both genders, despite snore and somnolence were presented in high prevalence. In the current study, although obstructive events associated with oxygen desaturation were higher in men, both genders had a high arousal index and reduced REM percentage, which shows impaired sleep architecture due to sleep fragmentation [14].
Although AHI<15 was prevalent among women, their snore complaint and ESS score were similar to men´s, as previous literature [11,12]. Epidemiological studies have shown that OSAS has been predominantly a disease of obese middle-aged men, and it is generally twice as common in men, in order to women’s OSAS begins after menopause14. The clinical study with 2,827 patients suggests that the severity of the disease is lower in females and is more associated with nocturnal choking, morning headache, fatigue, insomnia symptoms, and impaired memory, while men experienced more witnessed apnea [11]. Shepertycky and cols. (2005) also have described different tolerance of symptoms and clinical OSAS presentation between genders, such as fatigue, insomnia, and depression [12]. These findings suggest that women at the same AHI level may be under-evaluated for OSAS, using STOP BANG as the reference. Whereas obesity and diabetes prevalence were similar characteristics between genders, systemic hypertension was 4.48 times as likely in women, although OSAS severity was lower than men. However, in previous literature, hypertension and diabetes were also more common in women [11]. One limitation of this study is that transversal studies should not determine OSAS consequences. Besides, additional studies are necessary to compare sensitivity, specificity and predictive values to clinical consequences.
Conclusion
In conclusion, our data suggest that pulse oximetry, and STOP BANG score, may be used to screen this mixed ethnic population in adults with sleep complaints in order to prevent cognitive and cardiovascular effects.
Comparative Study of Clinical and Polysomnographic Characteristics of Obstructive Sleep Apnea Among Obese and Non-Obese Patients at Chiang Mai University Hospital-https://biomedres01.blogspot.com/2021/03/comparative-study-of-clinical-and.html
More BJSTR Articles : https://biomedres01.blogspot.com


No comments:
Post a Comment
Note: Only a member of this blog may post a comment.