Long-Term Health Related Survey Outcome of Pediatric Idiopathic Kidney Stone Formers
Introduction
In adults, the overall kidney stone prevalence has increased from 2.6% in the late 1960s to 8.8% in 2012 [1]. This trend was similarly seen in pediatric patients, as the incidence of kidney stone disease (hereafter, KSD) doubled from 6.9% between 1984- 1990 to 14.9% between 2003-2008 [2]. Numerous studies have demonstrated an association between adult KSD and systemic diseases, such as hypertension, diabetes mellitus, and obesity [3-6]. However, in pediatric patients, risk factors such as obesity remain poorly defined [7]. Risk factors causing idiopathic stones and the long-term sequela both remain poorly defined in pediatric patients. It is estimated that up to 75% of all pediatric stones are idiopathic in nature, the other 25% having an identifiable secondary cause, such as congenital urinary tract anomalies, metabolic deficiencies, or neurological disease [8]. Bonzo et. al, in a 2017 systematic review of pediatric and adult studies, suggest it is possible, but not yet proven, that pediatric stone forming patients have a higher lifetime risk of developing comorbid conditions, such as coronary heart disease, chronic kidney disease, bone mineral density problems, and hypertension later in life [9].
Their study also proposed that KSD presents in childhood will typically exist over one’s lifetime and is thus associated with these comorbid conditions. However, such a longitudinal lone-standing study has yet to be confirmed by others and there is a paucity of information on the long-term health outcomes and sequela of pediatric idiopathic stone formers [9]. Our hypothesis was those with idiopathic pediatric stone disease develop systemic medical conditions earlier compared to the age-matched general population (ages 18-44). Our study examined the development of future stones and development of chronic medical conditions in these pediatric idiopathic stone diseases.
Methods
After an Institutional Review Board (IRB-300000241) approval, a retrospective chart review from 1999-2005 of all pediatric kidney stone formers from Children’s of Alabama was performed. Patients with underlying conditions or stones secondary to another identifiable cause were excluded and only those who were idiopathic stone formers were included in the study. Survey responses were recorded between January 1st 2018 and December 31st 2019. Four hundred and twenty idiopathic stone formers were identified. Twenty-seven participants responded via a self-reported telephone survey and completed the survey interview (Supplement 1). Additional attempt to recruit more patients via mailed survey was not successful. Information gathered from participant’s medical record included: current age, age at first stone, number of stones before and after age 18, history of stones in first-degree relatives, and management of stones [conservative (i.e., medical expulsive treatment) vs surgical intervention (i.e., ureteroscopy, shockwave lithotripsy)]. Basic demographic information such as gender and race were recorded (Table 1). Patients who met the inclusion criteria were contacted by telephone based on their last known address. Development of health issues including diabetes, hypertension, chronic kidney disease, obesity, stroke, dyslipidemia, cardiovascular disease, inflammatory bowel disease, liver disease was assessed. Marital status, educational history, and employment status was obtained from participants.
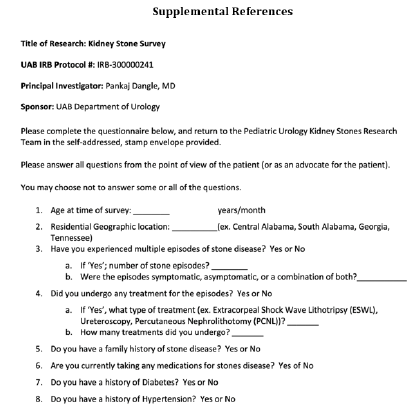
Supplement 1:Telephone survey utilized to assess the long-term outcomes in patients diagnosed with idiopathic kidney stones as children.
Results
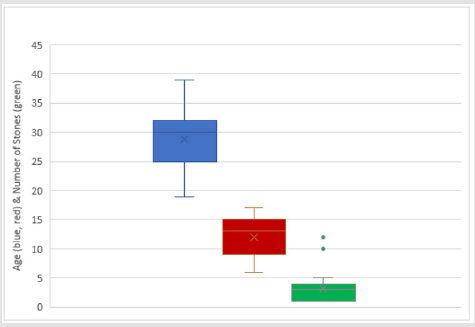
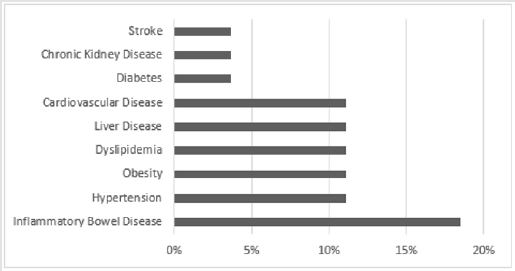
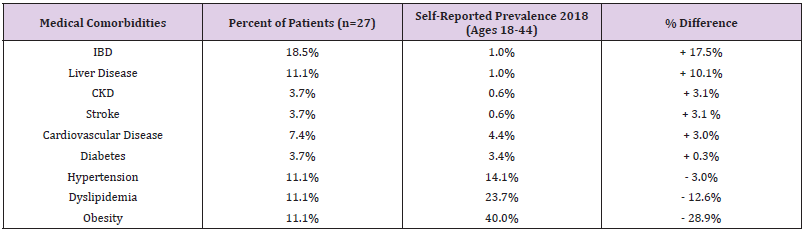
A total of 27 (6.4%) patients responded to our survey and were included in our analysis, 48% were male and 52% were female. The majority (96%) were white. Participants mean age was 29 years old (range 19-39; SD 4.5). Mean age of first stone event was 12 years old (range 6-17; SD 3.4) and the mean number of stone events after age 18 was 2.44 (median 2; range 0-7) (Figure 1). Patients reported less than one procedure (0.71) on average (median 0; range 0-4). Fifty-six percent (56%) of patients reported having a family history of KSD. At the time of the survey, fifteen percent (15%) of patients were still receiving regular follow up care from a urologist for management of their stone disease. All these patients actively seeing a urologist had also undergone a surgical procedure at some point, either shockwave lithotripsy or ureteroscopy. The majority of patients reported their health as good (56%) and outstanding (37%) with few reporting some chronic issues (7%) and none rating their health as poor. The prevalence of diseases surveyed were as follows: inflammatory bowel disease (19%), hypertension (11%), obesity (11%), dyslipidemia (11%), liver disease (11%), cardiovascular disease (7%), diabetes (4%), chronic kidney disease (4%), stroke (4%) (Table 2 and Figure 2).
Figure 1:Box and Whisker plot of age at time of survey (blue), age at time of first stone (red), and number of stones before age 18 (green).
Table 2: Medical comorbidities of pediatric stone formers during adult survey compared to self-reported prevalence of age groups 18-44 [18-23].
Discussion
There is a paucity of data surrounding the long-term health related outcomes of pediatric idiopathic stone formers. Based on our retrospective study, a subset of pediatric idiopathic stone formers may have an increased risk of chronic diseases. Of our population who responded to our survey the southeastern United States (Alabama), nearly 1 in 5 patients who suffered from idiopathic KSD during childhood were diagnosed with inflammatory bowel disease later in life. This is a particularly important finding as these disease states typically present as a malabsorptive disease, affecting gut permeability and subsequently glomerular filtration [10,11]. Crohn’s disease increases fecal fat, which binds luminal calcium, leading to a decrease in total calcium levels in the gut, causing increased delivery of oxalate to the colon [12,13]. This free oxalate is then absorbed and may cause a hyperoxaluria state in the tubules, predisposing patients to calcium oxalate stones. Hypothetically, a pediatric idiopathic oxalate stone may be secondary to undiagnosed, early inflammatory bowel disease, a finding seen here, and theoretically possible as discussed by Bianchi, et al. [14].
However, given that less than 10% of our patient population responded to this survey, there may be a component of response bias present. Patients who developed diseases may have been more likely to respond to our survey, compared to patients who did not develop one of these diseases, and thus may not have responded to our survey, artificially increasing the proportion of those who did develop a chronic disease, such as Crohn’s. Our study is a retrospective cohort study, conducted considering the findings suggested by Bonzo et al. in their 2017 landmark review, The Emergence of Kidney Stone Disease During Childhood-Impact on Adults [9]. Utilizing the Nurses’ Health Studies I and II, in addition to several other cohort studies, found that pediatric nephrolithiasis may increase the risk of coronary heart disease, bone mineral density issues, and hypertension independent of other known risk factors. However, the limitation of their review articles was utilizing notable amounts of adult findings and deriving pediatric conclusions. Our study is an attempt to assess the long-term impact of pediatric KSD on medical comorbidities and how to best establish follow up with them to identify new diagnoses years and decades later in adulthood. About 10% of patients who responded to the survey developed one or more of the following: hypertension, obesity, dyslipidemia, liver disease, and cardiovascular disease. Of note, our oldest patient population at the time of survey was only 39 years old, thus the development of these diseases in a relatively young population (<40 years of age) is noteworthy.
Stroke, chronic kidney disease, and diabetes were the least prevalent diseases found in our patients, each affecting only one patient in our study (Table 2). A total of 63% of our study cohort continued to have recurrent stone disease over the age of 18. This finding may suggest that having at least one idiopathic stone event in childhood predisposes to more stone events later in adulthood. One proposed mechanism or underlying etiology of these recurrent stones are chronic inadequate hydration and poor nutrition as primary factors [15,16]. Of the 27 pts, 63% of our patients had stones in adulthood, and several of our patients (15%) continued to see a urologist for regular follow up. Compared to the general United States population, ages 18-44, per the Center of Disease Control and Prevention Data and Statistics, our sample population of twenty-seven patients had an increased prevalence of diabetes (3.7% vs 3.3%), cardiovascular disease (7.4% vs 4.4%), inflammatory bowel disease (18.5% vs 1.0%), liver disease (11.1% vs 1.0%), stroke (3.7% vs 0.6%) and chronic kidney disease (3.7% vs 0.6%) (Table 2) [17-23].
Limitations
This was a single center, retrospective study, utilizing telephone interview surveys. Patients were not diagnosed by our clinical team within an in-patient or out-patient setting, but rather by this remote modality. There was no verification of data, with regards to the medical comorbidities reported by the patients. There is significant selection bias as well as recollection bias by the patients on the timing of stone disease, number of stones, procedures performed etc. This is a single center study with a relatively small sample size, we utilized the equal prevalence of disease assumption. On the survey, patients may have had selection bias and/or recall bias.
Conclusion
Pediatric idiopathic kidney stone formers continue to have
stones into adulthood and should have their care transitioned to
urologist and/or nephrologist for long-term care and management.
Select number of patients also appear to suffer from an increased
risk of developing chronic medical diseases, such as diabetes,
cardiovascular disease, inflammatory bowel disease and lover
disease compared to age matched general population. Larger
retrospective and prospective studies are needed to elucidate the
long-term health outcomes of these patients.
For more Articles on : https://biomedres01.blogspot.com/



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.