Pulmonary Neuroendocrine Tumor with Pancreatic Metastasis: A Case Report
Introduction
Neuroendocrine tumors are a group of tumors that share
morphological, immunohistochemical and ultrastructural
pathology and molecular features. The incidence of pulmonary
neuroendocrine tumor is gradually increasing, leading to distant
metastasis of liver, bone, brain, and adrenal gland [1]. However,
pancreatic metastasis is rare, which accounted for about 0.7% [2].
In addition, majority of patients with metastatic pancreatic cancer
had normal serum carbohydrate antigen 19-9 (CA19-9) levels [3].
We herein reported a case report of pancreatic metastases from
pulmonary neuroendocrine tumor with abdominal symptoms and
elevated serum CA19-9 levels. Previous studies were reviewed in
order to provide some experiences regarding the diagnosis and
treatment of such diseases.
Case Presentation
A 56-year-old male was admitted to the People’s Hospital of Suichang County on May 10, 2019 with epigastric dull pain radiating into the posterior back for more than 20 days and had no obvious aggravation and relief factors. There were no nausea or any change in bowel movement habits and weight, and no pulmonary and nerve system symptoms were observed. Some medications for gastritis were taken by him, but no effect was achieved. The patient denied previous medical history of cardiovascular disease, pulmonary disease, gastrointestinal disease, tuberculosis, and denied history of food and drug allergy. He has smoking history of 40 cigarettes/day for more than 30 years (smoking index > 1200). A 4cm*4cm mass was found in the left chest wall, with clear boundary, hard texture, and well activity. His abdomen was soft, with slight tenderness in the right upper abdomen. No enlarged systemic superficial lymph nodes were observed. No positive signs of cardiovascular system, pulmonary system and nervous system were found. Laboratory tests revealed elevated levels of carcinoembryonic antigen (CEA) 9.82ng/ml (reference range: 0-5ng/ml), and CA19-9 44.50U/ml(reference range: 0-37U/ml). Enhanced CT scan showed multiple pancreatic tumors with lymph node metastasis in the retroperitoneum. Pulmonary CT showed left lung tumor with multiple metastasis (of lung in the left chest wall and lymph nodes in the hilum, mediastinum, axilla). (Figure 1) Cranial MR suggested multiple abnormal signal nodules in both cerebellar hemispheres and considered it as metastatic.
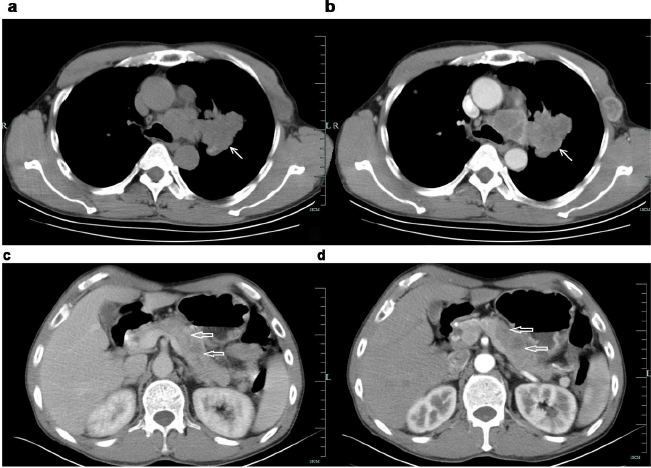
Figure 1: Enhancement CT of the patient.
a. a&b: Irregularly lobulated uniform-density soft tissue mass was found in the lateral hilar region of the upper lobe of the left lung, with mild enhancement in enhanced scanning. Bronchial stenosis and occlusion of the upper lobe of the left lung ⬉.
b. c&d: Multiple low-density lesions in the body and tail of enlarged pancreas, with delayed enhancement in enhanced scanning. The distal pancreatic duct was slightly dilated. The local fat space was not clear, and no enlarged lymph node was observed ⇐.
A multidisciplinary discussion (MDT) was conducted and concluded that the patient had a short course of disease and was generally in good condition, while radiology results suggested multiple occupying lesions in lung and pancreas, and advanced malignant tumors with multiple metastases. Metastatic process and elevated CA19-9 levels revealed lung metastasis from pancreatic cancer. However, according to radiological images, an irregular lobulated uniform-density soft tissue mass in the left lung was observed and was tended to be primary. Pathological diagnosis is considered extremely important. It is difficult to obtain a biopsy of lung and pancreatic lesion, for the limitation of medical equipment (such as endoscopic ultrasonography) in county hospital, and the patient was reluctant to be transferred. So coarse needle puncture biopsy of left chest wall mass was performed. The pathological results suggested (left chest wall puncture biopsy) neuroendocrine tumor (poorly differentiated neuroendocrine carcinoma), confirming it to be the origin of small cell carcinoma of the lung. Immunohistochemical results showed CgA (+), Syn (+), CD56 (+), CK18 (±), CK(±), CA199 (+), P53 (-), P63(-), P40 (-), Ki-67 (50%), ERCC-1 (+), CK7 (-), TTF1 (+), and Napsin-A (-). (Figures 2 & 3) Thus, the final diagnosis revealed extensive-stage small cell lung cancer with multiple metastases of pancreas, intracranial and left chest wall. The patient currently underwent six courses of chemotherapy and one course of cranial radiotherapy (30Gy/10F). The chemotherapy regimen used was etoposide (100mg/m2, d1-3) combined with cisplatin (75mg/m2, d1), and each course lasted for 21 days, according to the NCCN guidelines. After the first-course chemotherapy, the patient’s symptoms were improved. Follow-up CT after four courses of chemotherapy showed that the lesions in the lung, pancreas and left chest wall were obviously shrunken. (Figure4) The patient was closely followed up. The patient’s lung lesions developed later and eventually died of respiratory failure. The total survival time is 9 months. Patient’s informed consent was obtained to publish this case report.
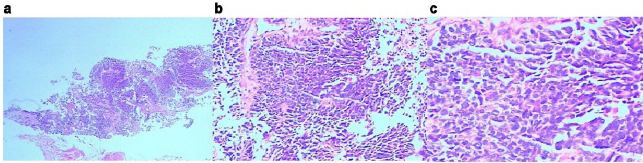
Figure 2: Pathological biopsy of the left chest wall.
a. HE, x2.
b. HE, x200.
c. HE, x400.
The cell layers were clustered and nested, and organ-like structures were seen. The cells were small with less cytoplasm, unclear nucleoli, partial vacuoles in the nucleus and chromatin. Karyokinesis was observed with local coagulation necrosis.
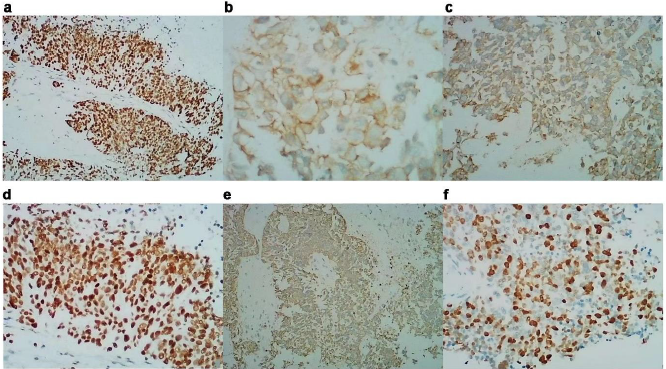
Figure 3: Immunohistochemistry of the patient
a. CgA(+);
b. Syn(+);
c. CD56(+);
d. TTF-1(+);
e. CK(±);
f. Ki67(50%)
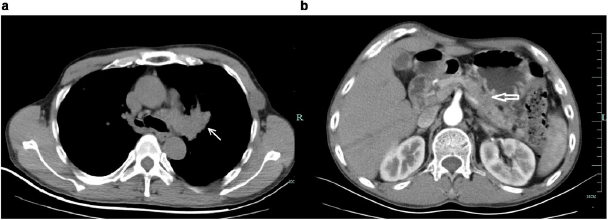
Figure 4: Enhancement CT of the patient after treatment.
a. Mass in the left lung was shrunken after treatment ⬉.
b. Lesions in the body and tail of enlarged pancreas were shrunken after treatment ⇐.
Discussion
Barnard has first reported neuroendocrine tumors in 1926 [4], and occurred in all parts of the body, including gastrointestinal tract, pancreas, bile duct, liver, lung, etc. Gastrointestinal neuroendocrine tumors are the most common neoplasms, accounting for 55-70% of all neuroendocrine tumors [5]. Recently, the incidence and prevalence of lung neuroendocrine tumors have increased linearly, and previous literature has reported as 1.35~1.57/ 100,000 people [6-7], accounting for 25% of primary lung tumors and 20%~25% of all neuroendocrine tumors [8]. Lung neuroendocrine tumors were divided into four histological types: small cell lung cancer (SCLC) (20%), large cell neuroendocrine cancer (LCNEC) (3%), typical carcinoid (TC) (2%) and atypical carcinoid (AC) (0.2%) [9]. SCLC is associated with smoking, mainly occurs in middle-aged and elderly men, and most commonly occurs in the hilum of lung. The 5-year and 10-year survival rates are 10% and 5%, respectively [10]. This patient has a previous risk of long-term smoking, and the primary lesion is located in the left hilum of the lung, which was consistent with the previous report [11].
Primary pulmonary neuroendocrine tumors are more prone to distant metastases, and the most common tissues included liver, bone, brain, and adrenal [1,12,13]. But pancreatic metastasis is quite rare, which accounted for about 0.7% [2]. Most of the metastases are still dominated by pulmonary symptoms, which might be related to the fact that the tumor cells metastasize to the pancreas through hematogenous or lymphatic routes, but there was no infiltration of the biliopancreatic duct wall. In this case, abdominal symptoms (abdominal pain) were the first symptoms, which were relatively rare, and may be related to the tumor compression of biliopancreatic duct. In addition, different from primary pancreatic cancer, majority of the patients with metastatic pancreatic cancer had normal serum CA19-9 levels [3]. He [14] analyzed 25 patients with pancreatic metastases and found that the CA19-9 levels were significantly increased in only one case of gallbladder cancer and one case of colon cancer with pancreatic metastases. Lung neuroendocrine neoplasms with elevated serum CA19-9 levels are rarely reported in the literature. According to the images of abdominal CT and elevated tumor markers (CA19-9 and CEA), our patient was misdiagnosed with pancreatic cancer. However, according to CT, and combined with patient’s advanced malignant status and good general conditions, the possibilities of uncommon tumors should also be considered, suggesting a multidisciplinary discussion. Thus, wide range of tumor properties should be considered during pathological and immunohistochemical examination. In addition, we also needed to consider the possibility that both the pancreas and lungs are primary lesions.
While the evidence supporting pancreatic metastases is as follows:
1. Miltifocal pancreatic masses
2. Slightly elevated CA19-9
3. Good condition and
4. The imaging finding supported the lung lesion tended to be primary.
For the limitaion of medical equipment (especially the endoscopic ultrasonography) in county hospital, and the the patient was reluctant to be transferred to the superior hospital, it is difficult to obtain a biopsy of lung and pancreatic lesion. The differentiation points of SCLC and other neuroendocrine tumor types included the cell size, the ratio of nucleoli to cytoplasm and the presence of nucleoli. Immunohistochemical markers of pulmonary neuroendocrine tumors were CgA (chromogranin A), Syn (synaptophysin), CD56, thyroid transcription factor 1 (TTF1), ki-67, et al. TTF-1 is a specific molecular marker of lung tissue and thyroid gland [15-17]. Syn, CD56 and CgA were considered as neuroendocrine markers. Among these, CD56 is more sensitive, while CgA and Syn are more specific [18,19]. The expression rates of Syn, CgA and CD56 were 91%, 54% and 87% in carcinoid (including typical carcinoid and atypical carcinoid), 91%, 54% and 87% in SCLC, and 76%, 97% and 92% in LCNEC, respectively [20]. In this patient, CgA, Syn, CD56, TTF1 and other lung neuroendocrine tumor markers were all positive, while CK7 and other gland sources and exocrine differentiation markers like Napsin-A were negative, and so the pancreatic sources were not considered. The diagnosis of left upper lobe SCLC remained clear.
The staging of SCLC was according to the AJCC TNM method and Veterans Administration Cancer Study Group (VALG) phase II method [21,22]. Surgery (T1-2) and concurrent chemoradiotherapy was performed within a limited stage, and chemoradiotherapy was performed for extensive stage [21-24]. The chemotherapy regimen used was platinum combined with etoposide or irinotecan [25- 28]. Patients with brain metastases should be treated with wholebrain radiation therapy, while prophylactic brain radiotherapy should be used by considering the disease carefully [29,30]. The brain metastasis of the patient was in extensive stage and received partial remission after 6 courses of etoposide and cisplatin (EP) chemotherapy, followed by whole-brain radiotherapy. After the first-course chemotherapy, the patient’s symptoms were improved. Follow-up CT after four courses of chemotherapy showed that the lesions in the lung, pancreas and left chest wall were obviously shrunken. However, the patient’s lung lesions developed later and eventually died of respiratory failure. The total survival time is 9 months.
Conclusion
We herein reported a case of pancreatic metastases from
small cell carcinoma of the lung with abdominal symptoms and
slightly elevated serum CA19-9 levels. The possibility of other rare
tumors should be considered in patients with multiple systemic
metastases but were in good general condition. Pathology and
immunohistochemistry should adequately used by considering
such situations.
For more Articles on : https://biomedres01.blogspot.com/


No comments:
Post a Comment
Note: Only a member of this blog may post a comment.