Hemostatic Hysterectomy in Rural Areas: New Thinks and Facts
Introduction
Uterus, symbol of femininity, has long been held responsible for all of woman’s supposed or real ailments [1]. So, its removal during pregnancy or in the post-partum is a decision of serious consequences. Bleeding (from the 3rd trimester and immediate postpartum) is the most serious complication of pregnancy and childbirth. It concerns 5 to 10% of pregnancies [2] and is responsible of 150,000 deaths per year worldwide [3]. It remains the leading cause of maternal mortality in developing countries while in developed countries, it represents the 2nd or 3rd etiology of maternal mortality [4]. In Senegal, it represents nearly a third of the maternal mortality ratio (29.6%) estimated at 236 per 100,000 live births in 2017 [5]. The evaluation of Emergency Obstetric and Neonatal Care (EmONC) carried out in 2013 showed that postpartum hemorrhage (PPH) occurred in 3.1% of deliveries and represented 44.2% of the direct causes of maternal death [5].
These bleeding deaths are considered preventable in 70 to 80% of cases [6]. Hemostatic hysterectomy therefore remains, in the whole of the therapeutic arsenal, an essential technique, whether it is carried out following childbirth by natural means or during a cesarean section. It is a surgical removal of the uterus, the incidence of which has steadily decreased over the past 30 years, stabilizing around one (1) per 1,000 births and one (1) per 211 cesarean sections [7]. However, it should be customary for obstetrician and gynecologists because it remains the last-line treatment and the “Gold standard” in the event of failure of conservative surgical treatment for immediate postpartum hemorrhage (IPPH). In view of these facts, it seems important to us to take stock of the practice of hemostatic hysterectomy in obstetric hemorrhages at the reference maternity unit in Tivaouane.
Patients and Method
This is a retrospective, descriptive study, carried out at the Abdoul Aziz Sy « Dabakh » hospital of Tivaoune between the 1st of January 2018 and the 31st of December 2019 on 30 cases. Its objectives were to assess the epidemiological, clinical and prognostic aspects of hemostatic hysterectomies performed in the Gynecology-Obstetrics department of the Abdoul Aziz Sy « Dabakh » hospital of Tivaoune in order to determine the frequency, the socio-demographic profile of the patients, to identify indications for hemostatic hysterectomy, establish the prognosis for hemostatic hysterectomy and make recommendations. All women admitted to the ward before or after childbirth and who underwent a hemostatic hysterectomy were included during the study period. Hemostatic hysterectomies for molar pregnancy were excluded. We studied the socio-demographic characteristics of the patients (age, address, parity, profession, medical and surgical history), clinical data related to childbirth, indication for hysterectomy, data from the surgical intervention, per- and post-operative complications, the length of hospitalization and post-operative consequences. Computer entry and statistical analysis were carried out using EPI Info software version 7.2.2.6.
Results
Hemostatic hysterectomy accounted for 0.6% of all deliveries that occurred during the study period. The mean age of the patients was 30 years (with extremes of 16 and 48 years); the age group from 26 to 35 was the most common (Table 1). The majority of patients (70%) lived in rural areas. The parity was between 1 and 9 with an average of 4. Multiparas were in the majority (50%) followed by paucipara (33.3%) and primipara (16.7%). Among our patients, 46.7% had only two (2) antenatal care (ANC) and only 26.7% did four (4) ANC. The medical history was dominated by high blood pressure (23.3%). Only 13.3% of patients had a history of cesarean section. Among the patients, 86.7% were evacuated from the two (2) Health Centers of the two (2) Municipalities as well as from the 48 Health posts. Only four (4) patients (13.3%) came on their own (Table 1).
Table 1: Characteristics of patients who have undergone a hemostatic hysterectomy at the Abdoul Aziz Sy « Dabakh » hospital of Tivaoune.
Note: *SD= standard deviation
Suspected retroplacental hematoma was the most frequent reason for admission (26.7%) followed by failure of fetal engagement (16.7%). On admission 55.2% of patients had normal consciousness and 20.7% were obsessed. A state of shock was found in 20% of our patients and clinical anemia in 33.3% of the patients. Uterine rupture was noted in 46.7% of patients and abruptio placentae in 33.3%. In our study, 90% of women gave birth by caesarean section and 10% gave birth vaginally. Most deliveries (96%) took place in the ward. Analysis of the birth showed that 70% of them ended in neonatal death. Amoung the live newborns, 44.4% were resuscitated at birth. In three (3) cases (10%), uterine revision accompanied by administration of oxytocics, misoprostol and uterine massage was performed. Only six (6) patients (20%) had conservative surgical treatment, most of them with triple arterial ligation according to Tsurilnikov (50%).
The indications for hemostatic hysterectomy were dominated by uterine rupture (50% of cases), followed by Couvelaire’s uterine apoplexy (33.3%). Hemostatic hysterectomy was performed for uterine atony in 10% of our patients, and 6.7% for coagulopathy (Table 2). The hysterectomy was subtotal and interannexial in 86.7% of cases. Only 6.7% had a total hysterectomy with unilateral adnexectomy. The postoperative effects were straightforward in 73.3% of patients. We had four (4) cases of persistent anemia and two (2) cases of acute renal failure. The average length of hospital stay was seven (7) days. We noted two (2) deaths whose identified causes were disseminated intravascular coagulation (DIC) in one case, and acute renal failure complicated by acute lung edema in the other.
Table 2: Distributions according to operative indications (series of hemostatic hysterectomies between January 1st, 2018 and December 31st, 2019 at the Abdoul Aziz Sy « Dabakh » hospital of Tivaoune, N=30).
Discussion
Frequency
The incidence of hemostatic hysterectomy has been steadily decreasing over the past 30 years, leveling off at around 1 in 1,000 births and 1 in 211 cesarean sections [7]. In our study, a frequency of 0.6% was noted, i.e., one hemostatic hysterectomy for 166 deliveries. This frequency is high compared to those reported in other series (0.016 to 0.4%) (Table 3). In developed countries, the low rate of this intervention is explained by the better conditions of patient care, in particular by the use of new therapeutic methods. The high frequency observed in our series is undoubtedly linked to the referential nature of maternity, which covers two (2) Health Centers and 48 Health Posts. There is a malfunction of the surgical branches of peripheral hospitals due to a lack of qualified personnel, suitable medical equipment, vital consumables and blood products and derivatives. In addition, the inaccessibility to care, both financially and geographically, is an aggravating factor at the rural level, and causes a delay in care at the origin of a radical therapeutic action. It is the same in other African countries, with which we share the same socio-sanitary conditions.
Maternal Age
Age is an important factor in the decision of a hemostatic hysterectomy because of its morbid impact on fertility. The average age is 30 years in our study, it is comparable to that found by most African authors [8,9]. The age group from 26 to 35 was the most represented (46.7%). This age group is usually the period of maximum fertility in our countries. The 16 to 25 age group was remarkable in our series, with a frequency of 30%. This young age could be explained by psychological immaturity, the early marriage of girls and the occurrence of pregnancy linked to sexual precocity. This age criteria may not intervene in a context of hemodynamic instability, which is noted in most of our patients because of geographic inaccessibility.
Parity
Multiparity is a major risk factor. The incidence of hysterectomy increases significantly with parity. We found 50% hemostatic hysterectomy in patients with more than four (4) children. The deleterious role of multiparity has been noted by certain authors [8], it weakens the myometrium, promoting uterine ruptures and inertias. The proportion of nulliparous patients having undergone a hysterectomy in our sample represented a significant slice. It is 16.7% in nulliparas. This large number confirms the notion of risk of pregnancy-puerperium in women with no experience of parturition.
Number of Antenatal Care (ANC)
An insufficient number of antenatal care (ANC) is a contributing factor in the occurrence of serious bleeding during delivery. It is a reflection of the monitoring, compliance and accessibility to care of our patients. Indeed, for 46.7% of our patients, the number of antenatal consultations was less than or equal to 2, while the WHO recommends at least 8 ANC. Some etiologies of serious bleeding during delivery can be controlled by good quality prenatal monitoring, in particular pregnancy-induced hypertension and its complications (placental abruption for example). In Togo, Akpadza found that the frequency of placental abruption (PA) tends to decrease as the number of ANC increases [10]. Patient education as well as continuing medical training for health workers (midwives, nurses and district physicians) is required in our regions. The production of a simplified prenatal care sheet to identify risk factors, the prevention of anemia and malaria is better suited in our regions.
Surgical History
Cesarean section is the only surgical history found in our study (13.3%). Although Stanco considers the Caesarean scar to be the primary risk factor (RF) [11], we have found a significant percentage (86.7%) of those who have no specific history at all. We can therefore conclude that hemostatic hysterectomy has no particular ground. According to the literature, in the majority of cases, no RF is identified [12,13].
Mode of Admission
The evacuated patients represented 86.7% of our patients and came from the two (2) Health Centers of the two (2) Municipalities as well as the 48 surrounding health posts. These evacuations are explained by our geographical position and the lack of operating theaters, resuscitation equipment, in referral centers, and the overflow of reception capacities. This study allowed us to deplore certain inadequacies in the evacuations such as: the poor performance of the partograph, the absence of venous intake, the absence of ABO / Rhesus blood grouping and the patients’ lack of financial means.
Reasons for Admission
They were dominated by the suspicion of placental abruption (PA) in 26.7% of cases. The reason for admission was different from the positive diagnosis on admission for 63.3% of patients. It was the same for Nayama [14] in his study which had before the hemorrhages of the third trimester. Hence the need for continuous training of health personnel in the periphery as well as the facilitation of evacuations.
General Condition
In our study, 20.7% of patients had a clouded consciousness (Glasgow at 13/15). Six (6) of them (20%) presented with shock (systolic BP less than or equal to 8 cmhg). Clinical anemia was noted in 33.3% of patients on admission. Similar results were found by Nayama in Niger [14] and Akpadza in Togo [15]. Mastering quality emergency obstetric care focused on the judicious use of the partograph, the correct use of oxytocics and antispasmodics, is essential.
Positive Diagnosis at Entry
Uterine rupture dominates the indications for hemostatic hysterectomy (46.7%). Our results differ from those reported in the literature where this indication represents 3 to 7% [16-18]. They are the consequence of unrecognized or neglected obstructed labor, abdominal expressions in peripheral maternity hospitals, the excessive use of oxytocics in health centers, the delay in evacuation and the lack of information and awareness among women. Placental abruption, an unpredictable pathology, occupied 33.3% of our indications and 70% of them had hypertension on admission, indicating a pre-existing pathology which should require an earlier referral. Most patients with PA developed coagulopathy due to the difficulty in accessing blood products and derivatives. Our results are similar to those reported by Nayama et al [14] and deplore poor monitoring of pregnancies.
Uterine atony represents 10% of our patients in our series. The factors favoring this atony join those classically found in the literature, great multiparity, obstructed labor, uterine distension [19,15,17,20]. The prevention of bleeding during delivery currently requires health workers to carry out a directed delivery for any patient, a mastery of the technique of artificial delivery and uterine revision.
Type of Delivery
Among the patients, 90% had given birth by caesarean section. According to some authors, caesarean sections cause bleeding. In our study, the indications for cesarean section were themselves risk factors for postpartum hemorrhage [21,22].
Status of the Newborn at Birth
A stillbirth rate of 70% was noted in our study, which is similar to the results of Nayama et al [3] but differs with the other Senegalese and African series. (Table 4). This deplorable prognosis is linked to the etiologies (PA and uterine rupture) and to the reduced possibilities of taking charge of certain emergency situations and finally to the overall delay in treatment.
Conservative Medico-Obstetrical and Surgical Treatment
herapeutic measures were undertaken whether medical, obstetric or conservative surgical before proceeding to radical treatment with 10% uterine revision accompanied by administration of oxytocics, misoprostol and massage uterine, 13.3% triple arterial ligation according to Tsurilnikov, 6.7% padding according to B-Lynch. According to the recommendations for clinical practice [23] and as said by Muteganya et al say, hemostatic hysterectomy forever compromises the obstetrical future of the parturient [17]. We must try at all costs a conservative treatment with the use of injectable prostaglandins or E2, arterial embolization and arterial ligatures. Due to the lack of injectable prostaglandin, the technical platform for embolization, and the unstable hemodynamic state of our patients, hemostatic hysterectomy was required.
Indication for Hemostatic Hysterectomy
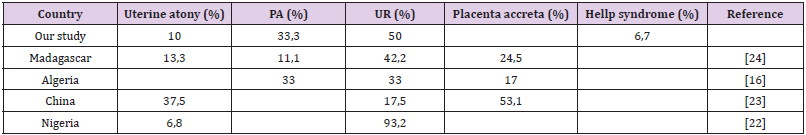
The frequency of hemostatic hysterectomies for uterine rupture in our series was 46.7%. It is found in the literature between 7 and 30% of cases of hemostatic hysterectomy [24,16,15]. In our series, the etiologies of uterine ruptures are either mechanical dystocia (16.7%) or great multiparity (13.3%), while in the literature, the majority occurs in a scarred uterus [24,16]. For ten (10) patients, coagulopathy was associated with the indications for hysterectomy. In Saadi’s series [18] it represents 38.46% of the indications. Coagulopathy was the result of a complication of placental abruption (PA) in the majority of cases in our study (10 out of 12 cases). We believe that consideration of severity indicators and early and appropriate medical resuscitation of PA will help reduce the incidence of hemostatic hysterectomy in this indication. (Table 5) summarizes the indications for different countries.
Type of Hemostatic Hysterectomy
Subtotal hysterectomy is described as the treatment of choice for postpartum hemorrhage [25]. In our series it occupied more than 86% of cases. Dissection is easier and the operating time is shorter, but the anatomical conditions of pregnancy make it difficult to identify the limits of the cervix, especially during labor. In addition, the risk of ureterovesical lesions is lower in case of subtotal hysterectomy. It was associated with unilateral adnexectomy in 6.7% of cases due to persistent bleeding requiring ligation of the lumbo-ovarian pedicle. Our results are comparable to those of the literature by the choice of the subtotal technique: 97.5% of cases for Tete et al [26], 82.2% for Diouf [27], 65.9% for Nayama [14] and 42% for Muteganya [17].
Operative Consequences
maternal mortality from obstetric haemorrhage has been proposed as a marker of the quality of obstetric care because more than 80% of these deaths are considered preventable, linked to non-optimal care [6]. The lethality found in our series is lower than that reported in the literature: Nayama [13] with 21.9% and Saadi [18] with 23.1%. The main cause of death in our series is disseminated intravascular coagulation (DIC), probably aggravated by the subsequent hysterectomy. It should be noted that the lack of red blood cells, blood derivatives (fibrinogen) and macromolecules were decisive in the occurrence of death in these cases of complicated blood depletion. It is urgent that the referral maternities have a deposit of blood products and its derivatives to compensate for wasted time (the blood bank is out of service) as well as better management of services [11]. The health authorities must also get involved to obtain a sufficient supply of consumables (fluids, macromolecules) from the intensive care unit of the referral maternity hospital.
Hospital Stay
the hospital stay was between one (1) and 16 days with an average of 7.5 days. Postoperative anemia was the main cause of morbidity requiring longer hospitalization of patients [26]. This hospital stay depends on the patients’ response to the treatments administered [27].
Conclusion
Hemostatic hysterectomy in obstetrics remains a topical intervention in our countries, especially in rural areas [28]. The use of hemostatic hysterectomy in our series was largely motivated by the few alternatives available to the practitioner and by the rapid and effective curative possibilities of this technique. Indeed, the procedure is simple, life-saving and unsystematic, especially compared to PA in our department, compared to hazardous and uncertain resuscitation in the face of disseminated intravascular coagulation [29]. In addition, in our developing and underequipped countries, we do not benefit from possibilities other than radical surgery, such as interventional radiology (complex logistics, training of radiologists, high cost of the procedure, admission methods patients). But certain inexpensive and easy-touse products (oral and parenteral prostaglandins) should logically be available in referral maternities in order to reduce the rate of hemostatic hysterectomy [30]. However, hemostatic hysterectomy is a necessary, important and vital intervention in many situations in our obstetric practice. The technique must be quickly mastered by the juniors and seniors providing guards and emergencies. It remains a reality and is a common practice in our structures [31].
For more Articles on: https://biomedres01.blogspot.com/



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.