Two to Nine Year Review of Breast Conservation Therapy (BCT) for Breast Carcinoma: Clinico-Pathological Features and Outcomes in a Single Centre in East Africa
Introduction
Breast cancer is the most commonly diagnosed cancer and the leading cause of cancer death in women world over. In Africa, it accounts for one in four diagnosed cancers and up to 20% of cancer deaths in women [1-3]. Age-adjusted incidence in non-Hispanic white women in the United States from breast cancer is 127.3 per 100,000 compared to the African-American women’s 118.4. However, age-adjusted mortality is higher in the African-American women at 30.8 per 100,000 women when compared to the non-Hispanic white women, which is at 22.7 per 100,000 women [4]. It is postulated that breast cancer in third world countries occurs less frequently when compared to the resource-rich countries. However, the mortality-to-incidence ratios, is higher in third world countries. For example, case fatality is approximately four times greater in East African women compared to North American women [5]. Most countries in Sub-Saharan Africa do not maintain cancer registries hence limited data. Details of death registration varies from ne 100% in the World Health Organization (WHO) European Region to less than 10% in the African Region. Cancer-specific mortality statistics are available for only three countries, Mauritius, Reunion & South Africa. More than half of African women diagnosed with breast cancer die of the disease [6]. Breast cancer being a heterogeneous disease also manifests racial differences in the age, grade, receptor status, stage and even mortality. It has been postulated that higher mortality and lower survival rates among African-American women are because of factors associated with lower socioeconomic status and late stage at diagnosis [7-11]. Poverty, illiteracy, and a lack of health insurance are also associated with lower survival rates [12,13]. These racial differences in survival persisted even after adjusting for stage at diagnosis, access to health care, treatment, comorbid illness, marital status, and other pathologic and socio-demographic variables [14-17]. Aggressive tumor characteristics associated with poorer prognosis appear to be more common in African American women and may also contribute to lower survival rates [18,19]. By 2010, breast cancer death rates were 41% higher in African American than white women [4]. These Afro-American statistics may reflect the African female breast cancer patients probably due to their shared ancestry [20-23].
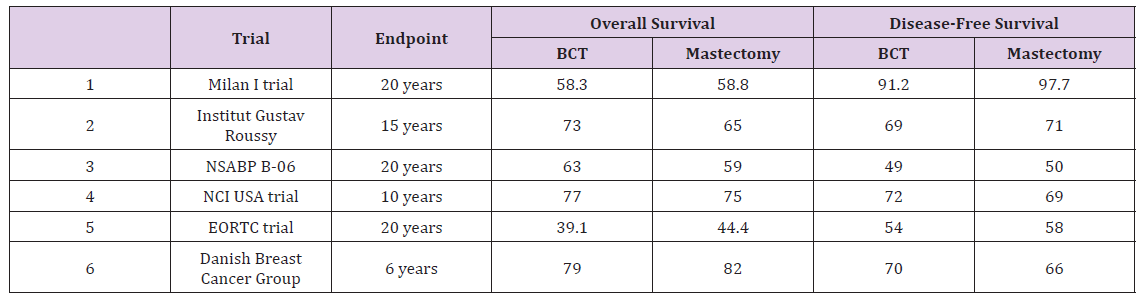
The history of breast cancer treatment is rich. Leonides championed for a wide margin of excision and excision of localized tumor, foreshadowing the oncological principles of contemporary cancer surgical practice [24,25]. Galen, attributing breast cancer to the accumulation of black bile in the blood, suggested that it was a systemic disease [25]. During most of the 20th century William S. Halstead of Johns Hopkins hospital in the United States of America (USA) promoted radical mastectomy (first reported in 1894) and emphasized on removing tissues in one piece to prevent spread [26]. This was the treatment of choice for breast cancer of any stage, regardless of the patient’s age, for about 80 years. Patey and Handley from London advocated for modified radical mastectomy which preserved the pectoralis major muscle [27]. A randomized clinical trial to compare radical mastectomy with breast conservation surgery was then approved by the WHO in 1969. The recruitment of patients began at the Milan Cancer Institute in 1973, after the new procedure was standardized, and preliminary data showed that survival rates were equal after radical and breast conserving surgery were published in 1977 and 1981 [28,29]. The above studies provided necessary information that allowed dramatic reductions in the extent of surgery required for local control of breast cancer with decreases in treatment related morbidity that then popularized BCT [30-36] (Table 1).
 Surgical Treatment of Early Breast Cancer
Surgical Treatment of Early Breast CancerNon-metastatic breast cancer includes early stage defined as patients with clinical stage II or below [37]. Generally, patients with respectable breast cancer can undergo BCT or mastectomy with or without reconstruction. BCT refers to excision of the breast tumor with concentric margin of surrounding healthy tissue and overlying skin island that has the biopsy site included and done in a cosmetically acceptable manner [38]. Its goals are to provide the survival equivalent of mastectomy, a cosmetically acceptable breast, and a low rate of recurrence in the treated breast. BCT allows patients with breast cancer to preserve their breast without sacrificing oncologic outcome. There are few absolute contraindications to BCT [39]:
a) First or second trimester pregnancy
b) Multicentric breast cancer.
c) Previous irradiation of the breast.
d) Persistent positive tissue margins after surgery.
e) Connective tissue disorders like scleroderma.
f) Large tumor size to breast ratio is a relative contraindication to BCT.
For such patients an alternative approach is the use of neoadjuvant chemotherapy to downstage the tumor.
Most patients in Africa typically present approximately 10 years younger than breast cancer patients of western nations and at advanced stages [20,40-43]. African young women suffer a severe form of the disease in terms of higher grade, late stage at diagnosis and a worse prognosis. A higher prevalence of hormone receptor negative and Triple-Negative Breast Cancers (TNBC) has also been previously reported [40-43]. TNBC subtypes account for 12-20% of all breast cancer; however, women of African descent tend to have a high incidence of TNBC translating into poorer outcomes [44]. A study by Sayed et al. [45] at the Aga Khan University Hospital, Nairobi (AKUHN), however indicated that the receptor status may be comparable to that in the west, with 72.8% ER positive breast cancer, 64.8% being PR positive, HER2 in 17.6% and TNBC in 20.2% [45]. The majority of women (over 50% to 70%) present with late stage disease that is not amenable to BCT. This makes mastectomy to be the most common surgical procedure performed [43,46].
The Aga Khan University Hospital, Nairobi (AKUHN), is a tertiary private teaching hospital that has an active breast clinic that is also dedicated to breast cancer screening, diagnosis and management. We have multiple awareness programs including seminars, breast cancer month that have enabled detection of breast cancer at its early stages. The patient profile comprises urban, literate women with access to information, health insurance and healthcare facilities. The age group most affected by breast cancer is in the 45-49-year range with only about 32.5% presenting with early disease. Thirty one percent of the patients under 50 years have early disease. This patient population under 50 years make up about 66% of the breast cancer female patients [51]. BCT is an available option offered to patients who meet its criteria. This has been made possible with the availability of surgeons with experience in oncoplastic techniques, well equipped laboratory with capability of doing frozen section with prompt reporting of the results and radiotherapy services with radio-oncologists. About 20% of the patients with breast cancer undergo breast conservation. BCT has been practiced at the Aga Khan University Hospital Nairobi (AKUHN) since the year 2008 with over 150 cases up to the year 2015 [52].
In terms of adequacy of excision margins, which is a requisite in BCT, Riogi et al. demonstrated that for breast conservation surgeries done in AKUHN up to 85.7% were negative and only 14.3% needed a re-excision or mastectomy [52]. This is comparable to published rates in the western world [53-55].
BCT is a novel therapy for breast cancer in East Africa [56,57]. We intend to evaluate the clinico-pathologic features of our breast cancer patients who undergo BCT and how they fare after such treatment in terms of disease-free survival and overall survival. We also intend to compare their clinico-pathological features and outcomes with the patients who undergo MRM. To our knowledge, no studies in the region have been done on BCT clinico-pathological features and outcomes. This is in the background of differences in the molecular subtypes in the African women and the comparatively younger age affected by breast cancer. Compared with data on the incidence and overall burden of the disease, there is a significant paucity of data on breast cancer outcomes including overall survival and disease-free survival comparing breast conservation therapy and mastectomy. As such most of our practice is based on evidence outside Africa. The evidence for the implementation of BCT as the alternative treatment for early breast cancer to mastectomy is largely from studies done in the western nations. This is in the background that breast cancer in younger women is characterized by a more aggressive disease [58].
The aim of this study was to describe an institutional experience with BCT in terms of the clinico-pathological features and the outcome after such treatment.
To determine the clinico-pathological features, disease free survival and overall survival of breast cancer patients who had undergone BCT between 2008 and 2015 at AKUHN.
To describe BCT and mastectomy in terms of
a) Overall survival and disease-free survival.
b) Stage and grade of breast cancer.
c) The molecular subtypes.
Research Design
This was a single institution historical cohort study of female patients with breast cancer treated with either breast conservation therapy or modified radical mastectomy. The study employed crosssection retrospective design to collect data from records of women that underwent surgery between the periods: 1st January 2008 to 31st December 2015.
Data collection was done via retrieval of records of patients who had breast surgery for breast carcinoma at AKUHN between 2008 and 2015. Data was obtained from the hospital’s medical records department. Pathology reports were obtained from the hospital’s software system ‘care2000’. Patients’ details were assessed for demographics like age, patient’s race and parity; clinical manifestation like breast lump, breast pain, nipple discharge; tumor-related characteristics (tumor size, TNM stage and grade, molecular subtypes), treatment-related characteristics and followup related characteristics. (See Patient Data Capture Sheet: Breast conservation therapy at the AKUHN 2008-2015 and the appendix below). Data on staging were retrieved from the pathology report biopsy specimen, clinical assessment of the admitting physician as recorded in the file or when absent, they were derived by assessing the staging investigations entered in the file. The American Joint Committee on Cancer (AJCC) 7th edition staging system was used [21].
All eligible candidates were recruited. This included all the breast cancer patients underwent breast conservation therapy between 1st January 2008 and 31st December 2015.
January 1st 2008 and December 31st 2015.
–IIIA breast cancer
Records of patients with breast cancer of stage IIIB to Stage IV. Bilateral breast cancer by the time of index surgery Previous history of another cancer. Histology not consistent with a solid breast tumor, including sarcoma, pagets disease of the nipple, lymphoma and hematopoietic tumor
Figure 1: Patients presenting with breast lumps.
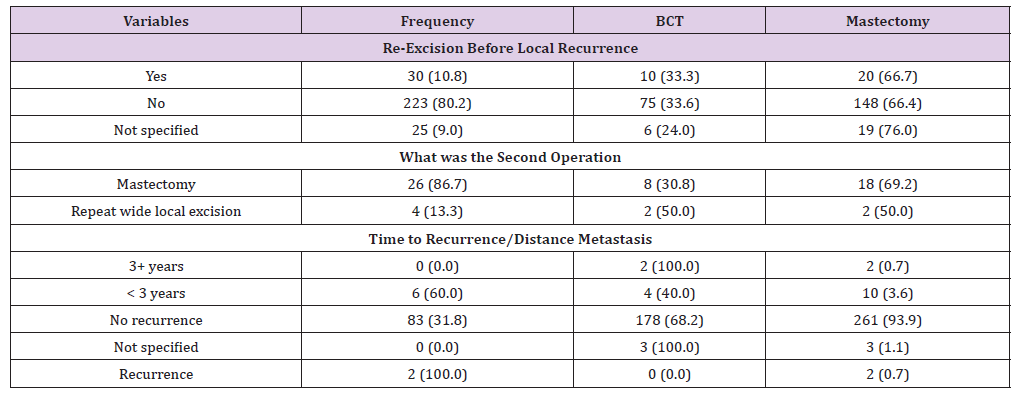
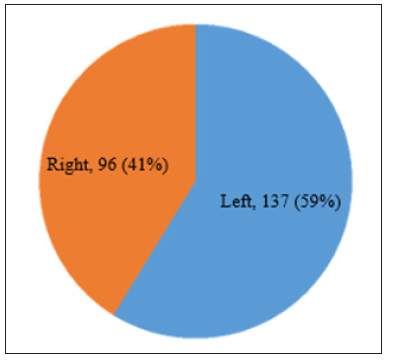 Profiling of patient-related characteristics was done. This included age, race, parity, presenting symptoms and laterality. Tumor- related characteristics was also profiled to include the size, nodal status, histologic subtype and receptor status. Treatmentrelated characteristics included neo-adjuvant therapy, adjuvant therapy, resection margins, conversion to mastectomy rates and hormonal therapy. Follow-up related characteristics included time to recurrence, number of follow up visits and duration of follow-up. We did not obtain data on mortality and therefore did not analyze mortality rates. Data were collected via a data-sheet form designed for the study (see appendix below) and entered into a spreadsheet program. These were then analysed done using stata version 12 and two sample tests of proportion to compare the equality of the proportions. The results (percentages, rates and proportions) were presented in tables and graphs. Data collected were stored in a safe computer with a password only accessible to the principal investigator (Tables 2 & 3) and (Figure 1).
Profiling of patient-related characteristics was done. This included age, race, parity, presenting symptoms and laterality. Tumor- related characteristics was also profiled to include the size, nodal status, histologic subtype and receptor status. Treatmentrelated characteristics included neo-adjuvant therapy, adjuvant therapy, resection margins, conversion to mastectomy rates and hormonal therapy. Follow-up related characteristics included time to recurrence, number of follow up visits and duration of follow-up. We did not obtain data on mortality and therefore did not analyze mortality rates. Data were collected via a data-sheet form designed for the study (see appendix below) and entered into a spreadsheet program. These were then analysed done using stata version 12 and two sample tests of proportion to compare the equality of the proportions. The results (percentages, rates and proportions) were presented in tables and graphs. Data collected were stored in a safe computer with a password only accessible to the principal investigator (Tables 2 & 3) and (Figure 1).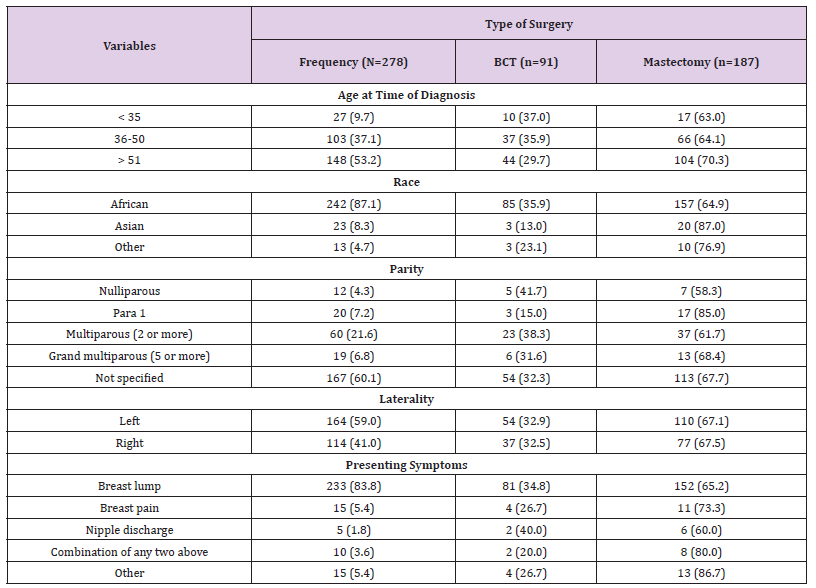 Table 3: Pathological characteristics of patients.
Table 3: Pathological characteristics of patients.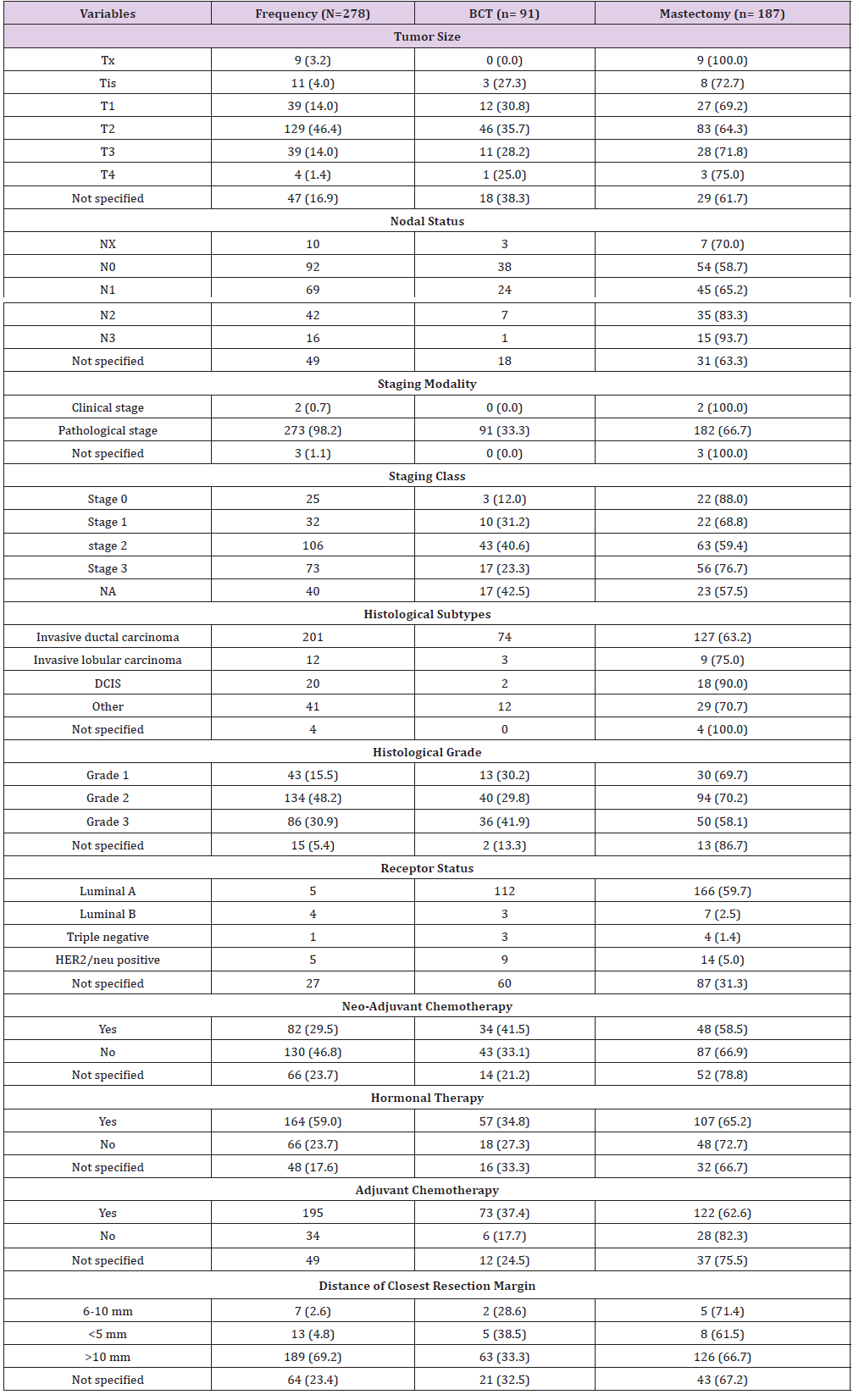 Discussion
DiscussionThe Aga Khan University Hospital, Nairobi (AKUHN), is a tertiary private teaching hospital that has an active breast clinic that is also dedicated to breast cancer screening, diagnosis and management. We have multiple awareness programs including seminars, breast cancer month that have enabled detection of breast cancer at its early stages. BCT is an available option offered to patients who meet its criteria and has been practiced at the Aga Khan University Hospital Nairobi (AKUHN) since the year 2008 with over 150 cases up to the year 2015 [52]. In this study, breast conservation therapy was offered to 32.7% of the breast cancer patients who were eligible for it. Although this is higher than early work done by Riogi and Wasike in which only 21.9% had BCT [52], it is still lower than what other series report of about 48% [61,62] (Table 4). This relatively higher utility of BCT can be attributed to the longer study duration and the higher sensitization of BCT. In terms of age, 53.2% of the patients were over the age of 51 years, which is similar to what Maalej reported in Tunisia [47] and from the global perspective [63,64]. Previous study at AKUHN had indicated an average age of 45 years [51,52]. Young-aged breast cancer (less than 35 years) was 9.7% in our series similar to Korea but higher than in the US and European countries [65,66].
 When BCT was compared to mastectomy, we found that BCT was popular among the younger patients, mastectomy was commoner as the age increased. The sample population was largely African (87.1%), likely due to their predominance in this locality. However, this could also be due to the limited number of patients in this study. BCT was offered in up to 36% of the African which would reflect the relatively higher socioeconomic status of this patient population. This is however anecdotal as we were not able to gather such data due to inadequate record keeping. The Asian race, though relatively common in the hospital’s catchment area only contributed to 8.3%. A surprising finding was the relatively lower proportion of breast cancer in the nulliparous women (4.3%). This was surprising since traditionally this has been a risk factor to breast cancer [20,67-69]. Makanga et al. [51] in his study also found a relatively lower incidence of 16% of the breast cancer patients to be nulliparous [51]. This however could be attributed to the lower number of patients and the inadequacy of documentation in a retrospective study.
When BCT was compared to mastectomy, we found that BCT was popular among the younger patients, mastectomy was commoner as the age increased. The sample population was largely African (87.1%), likely due to their predominance in this locality. However, this could also be due to the limited number of patients in this study. BCT was offered in up to 36% of the African which would reflect the relatively higher socioeconomic status of this patient population. This is however anecdotal as we were not able to gather such data due to inadequate record keeping. The Asian race, though relatively common in the hospital’s catchment area only contributed to 8.3%. A surprising finding was the relatively lower proportion of breast cancer in the nulliparous women (4.3%). This was surprising since traditionally this has been a risk factor to breast cancer [20,67-69]. Makanga et al. [51] in his study also found a relatively lower incidence of 16% of the breast cancer patients to be nulliparous [51]. This however could be attributed to the lower number of patients and the inadequacy of documentation in a retrospective study.The staging modality was predominantly pathological. Early stage disease was noted in this with 58.6% of the patients presenting with stage 0, I or II disease. Twenty six percent presented with stage III disease. This is contrary to what Makanga et al. had earlier found of only 32.5% of breast cancer patients having early stage disease [51]. Our findings in this study could be attributed to the earlier diagnosis in this population of patients but also the exclusion of stage IV breast cancer patients and the limited number of patients cannot be underplayed. Calleb et al. demonstrated late stage of presentation at the coast provincial general hospital [73]. Similar findings were obtained by Vorobiof et al. in South Africa and Fregene et al. [20,74]. The proportion of breast cancer patients in which BCS was appropriate was not stage dependent; 4.1% (n=3) in carcinoma in situ, 14.9% (n=11) in stage I, 58.1% (n=43) in stage II and 22.9% (n=17) in stage III. This is in contradistinction to what Tyldesley et al. [62] found, though for the suitable BCS patient, higher stage is not a contraindication to the operation. When stage was compared to the age groups, it was found that postmenopausal women (over the age of 50 years), were the majority across all the stages of disease. However, there was no statistical significance noted when stage was compared across the different age groups.
This being a retrospective study, the investigator had to retrieve pre-existing data that was not necessarily acquired in a predetermined way and hence inherently susceptible to poor record keeping, lack of standardization and methods of recording. We particularly faced challenges from the private patients where the recording was highly abbreviated and poor follow up was noted. We were not able to estimate disease free survival rates and overall survival rates largely as a result of lack of data on mortality. This could have been due to loss of follow up of our patients or lack of documentation of such. The lack of significant difference to the characteristics analysed may be because of the small sample size used in this study.
Standardization of patients records especially for cancer diagnosis. This will facilitate future population or hospital-based studies with better precision and accuracy. Follow up of the patients was noted to be erratic and led largely to inadequate record keeping. This can be reduced by perhaps calling patients whose appointments is due and finding out their reason for not coming for review or for choosing another facility for continued care. A larger study with prolonged follow up patients will be more generalizable to the population.
This is therefore also recommended.
Concurrent Determination of Danshensu and Hydroxyl Ligustrazine in Rat Plasma Using High-Performance Liquid Chromatography and its Application to the Pharmacokinetic Study of ADTM,
DSS and TMP-OH Following Intravenous Administration-https://biomedres01.blogspot.com/2020/11/concurrent-determination-of-danshensu.html
More BJSTR Articles : https://biomedres01.blogspot.com



No comments:
Post a Comment
Note: Only a member of this blog may post a comment.